Nora Osemene, MS, PharmD
Associate Professor and Chair
Department of Pharmacy Practice
College of Pharmacy and Health Sciences
Texas Southern University, Houston, Texas
Herpes zoster infection (shingles) results from the reactivation of varicella zoster virus infection. Within the spinal ganglia and sensory nerves lay clinically dormant varicella zoster virus acquired during the primary varicella (chickenpox) infection.1 The reactivation of the varicella zoster virus is associated with progressive decline in varicella zoster—specific, cell-mediated immunity related to aging or conditions with diminished immunity such as cancer and diabetes. This reactivation and the accompanying inflammation lead to central nervous system dysfunction, which is manifested as debilitating pain. Low levels of immune globulin have been shown to predispose patients to recurring herpes zoster infection.
While varicella virus infection mostly affects the young, shingles and its complications mainly affect older persons. In excess of 60% of people older than 60 years, especially those with diminished immunity due to diabetes and cancers, are afflicted by herpes zoster. More than 50% of people who live to be 85 years will develop shingles. About 20% of people with herpes zoster develop postherpetic neuralgia (PHN).2 The pain associated with postherpetic neuralgia is very debilitating and lasts long after the herpetic rash is cleared. Postherpetic neuralgia is very resistant to treatment and results in decreased quality of life.
PATHOPHYSIOLOGY AND PRESENTATION
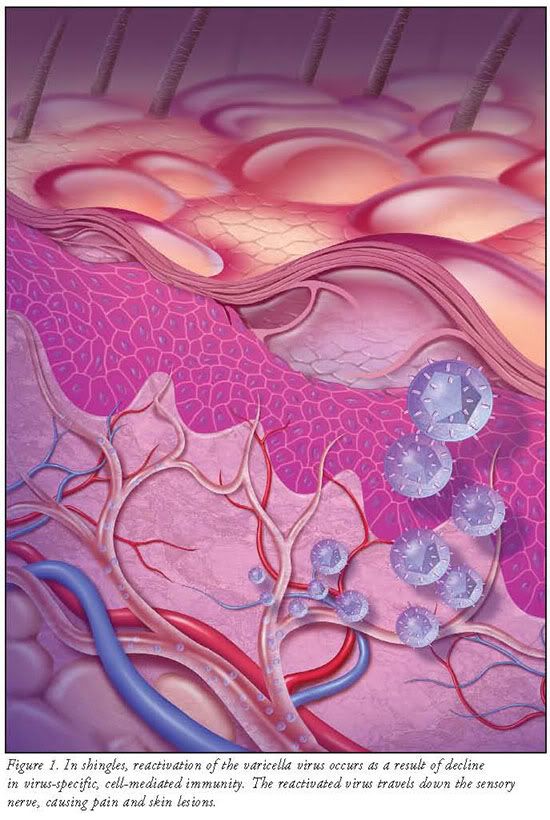
Varicella virus infection is the primary infection in patients with compromised immunity. The virus gains entry into nerve cells in the sensory dorsal root ganglia.3 The mechanism of the virus's entrance into the dorsal ganglia and the nerve cells is not completely understood. Initially, the host is able to produce varicella zoster virus—specific, cell-mediated immunity during the infection. This ensures that the virus remains latent within the host ganglia. Periodically, endogenous and exogenous boosting of the immunity against varicella results in the virus remaining dormant for decades. Eventually, reactivation of the virus occurs as a result of decline in virus-specific, cell-mediated immunity. Normal age-related decline and diseases such as malignancies and HIV impact the reduction in cell-mediated immunity and the reactivation of dormant varicella virus. The reactivated virus travels down the sensory nerve, causing pain and skin lesions (FIGURE 1). Shingles usually develops in stages.4,5
Early Stage
The initial stage of shingles precedes the active stage with a conundrum of symptoms that last several days or weeks before the shingle rash appears. Patients with early signs of shingles complain of headaches, hypersensitivity to light, flulike symptoms without fever, itching, tingling, and burning or pain around the affected area. The affected nerves are usually found on the trunk of the body but may sometimes be distributed on the face, neck, arm, leg, or abdomen. The lymph nodes may be swollen and tender as well. These symptoms last a short time and are followed by skin rash.
Active Stage
The rash develops from maculopapular lesions forming a beltlike pattern on the patient's trunk, but the band of rash may appear anywhere on the body including the eyes. Some patients get very mild rash or none at all. The rash evolves into vesicles and blisters that are extremely painful, often described as like a piercing needle in the skin, accompanied by anxiety and flulike symptoms. These vesicles become crusted within 7 to 10 days and are shed, leaving scarring and pigmented changes on the skin. Pain is the primary complaint with active-stage shingles and the symptom for which patients seek medical care. The pain is described as persistent, with a burning or stinging sensation.6 In patients who are immunocompromised, zoster initially presents in a typical fashion. However, the rash in these patients tends to be more severe with prolonged duration. One specific risk for patients who are immunocompromised is dissemination of the zoster rash. Cutaneous dissemination generally occurs only among immunocompromised patients, occurring in up to 37% of zoster cases in the absence of antiviral treatment. While cutaneous dissemination is not life-threatening, it is a marker for potential virus seeding of the lungs, liver, gut, and brain and can cause pneumonia, hepatitis, encephalitis, and disseminated intravascular coagulopathy in 10% to 50% of episodes.
Complications
Many complications can occur with herpes zoster infection. In 10% to 25% of cases, patients contract herpes zoster ophthalmicus (HZO). Keratitis occurs in approximately two-thirds of patients with HZO, often causing corneal ulceration. Other complications include conjunctivitis, uveitis, episcleritis and scleritis, retinitis, choroiditis, optic neuritis, lid retraction, ptosis, and glaucoma. Extraocular muscle palsies can also occur. Prolonged or permanent sequelae of HZO include pain, facial scarring, and loss of vision. Occasionally, zoster can cause motor weakness in noncranial nerve distributions, calledzoster paresis. The weakness develops abruptly within 2 to 3 weeks after onset of the rash and can involve upper or lower extremities. Diaphragmatic paralysis has also been described. Rarely, patients will experience acute focal neurologic deficits weeks to months after resolution of the zoster rash, involving the trigeminal distribution contralateral to the initial rash. This ischemic stroke syndrome is termed granulomatous angiitis. Mortality from this syndrome is substantial. Other rare neurologic complications of herpes zoster include myelitis, aseptic meningitis, and meningoencephalitis. The risk for neurologic zoster complications is generally increased in immunocompromised persons. The most common chronic complication of shingles remains PHN.
Postherpetic Neuralgia
The main symptom associated with postherpetic neuralgia is pain, which persists for a long period beyond the resolution of the shingles rash. The features of PHN pain vary from mild to excruciating in severity, can be constant or intermittent, or triggered by trivial stimuli. Patients complain of pain in response to nonnoxious stimuli such as pressure from clothing, bed sheets, or the wind. Approximately half of patients with zoster or PHN describe their pain as horrible or excruciating, ranging in duration from a few minutes to constant on a daily basis. The pain, which is characterized as burning and lancinating, is chronic, intractable, and distressing. It can disrupt sleep, mood, work, and activities of daily living, adversely impacting the quality of life and leading to social withdrawal and depression. The pain is stipulated to be due to persistent C-fiber nociceptor activity in the nerve cells, although studies have shown chronic neural loss and scarring in nerves affected by herpes zoster injury. What has not been established or shown is how the associated inflammation causes pain. The pain of PHN commonly affects the forehead or chest.
MANAGEMENT OF SHINGLES
There are three main objectives in the management of shingles. The first objective is to treat the acute viral infection. The second objective is to treat the associated pain in the acute phase and in PHN, and the third objective is to prevent the occurrence of PHN and other complications. To achieve these objectives, antiviral agents, oral corticosteroids, and pain management are utilized.
Antiviral Therapy
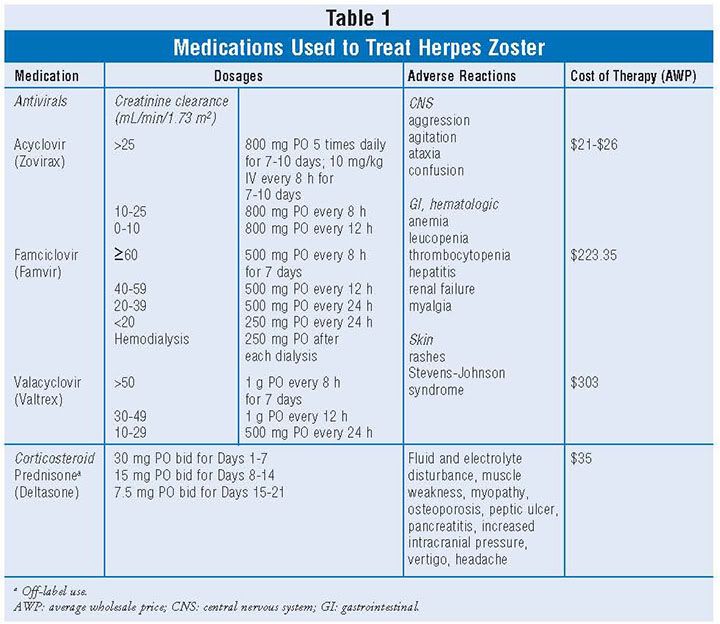
The choice of antiviral agent should be individualized with considerations for dosing frequency, clinical outcomes, and cost.7 TABLE 1 shows the available antiviral agents and dosing schedule. Acyclovir is a DNA polymerase inhibitor. It is available for both oral and intravenous use. The main disadvantages when acyclovir is administered orally are low bioavailability and the 5-hour dosing frequency. Acyclovir's multiple-dosing requirements often lead to noncompliance. The parenteral route is available for patients who are unable to utilize the oral dosing route. Valacyclovir is a prodrug of acyclovir with less frequent administration of every 8 hours. Another advantage of valacyclovir compared to acyclovir is better bioavailability, producing comparable blood levels to parenteral acyclovir. Valacyclovir appears to be more efficacious in decreasing the severity of pain associated with acute herpes zoster and the duration of the PHN when compared to acyclovir. Famciclovir is also a DNA polymerase that is administered every 8 hours. Famciclovir has the advantage of having longer intracellular half-life compared with acyclovir and a superior biovailability compared to both acyclovir and valacyclovir. When antiviral therapy starts within 72 hours of the onset of herpes zoster, acyclovir, valacyclovir, and famciclovir have been shown to significantly shorten the periods of acute pain, virus shedding, rash, and acute and late-onset complications. Both valacyclovir and famciclovir have been shown to lessen the incidence and severity of PHN. No antiviral agents as of yet prevent the development of PHN.
Corticosteroids
Oral corticosteroids are useful in the treatment of acute herpes zoster.8,9 Clinical trials have shown variable results. Prednisone use in conjunction with acyclovir resulted in the reduction of the pain associated with acute herpes zoster. It has been postulated that the mechanism of the steroid effect is due to decrease in the degree of neuritis caused by the active infection, decreasing the resulting damage to affected nerves. Despite the usefulness of prednisone in managing the associated pain with herpes zoster infection, it has not been shown to decrease or prevent the incidence of PHN. The risk of immunosuppression may hinder the use of steroids in high-risk patients.
Pain Management of PHN
The main objective in the treatment of PHN is pain relief. Frequently, PHN does not respond well to treatment. The pain relief is partial, and pain may last the remainder of the patient's lifetime. The pain is chronic, intractable, and distressing for the patient. Pain therapy may involve the use of multiple agents including topical analgesics, tricyclic antidepressants, anticonvulsants, narcotics, and intervention therapy (TABLE 2).
Topical Analgesics
Capsaicin, an extract of chili peppers, is approved in the United States for treatment of PHN.10,11 Clinical trials have demonstrated capsaicin's efficacy compared to placebo in the management of PHN pain. The application of capsaicin to the skin produces a burning sensation, which triggers the release of substance P, a neuropeptide, from pain fibers. The depletion of substance P in the nerve fibers from repeated exposure to capsaicin results in analgesia. Capsaicin cream must be applied three to five times daily to achieve substance P depletion from the pain fiber and analgesia. The need for regular application of capsaicin must be emphasized to patients to maintain pain relief. Additionally, patients must understand that the pain may initially increase within the first week of initiating the therapy because it initially acts as an irritant by stimulating the nerve endings before desensitizing afferent C-fibers. It is important to educate patients on the need for thorough hand washing after each application of capsaicin. Hand washing prevents accidental transfer of capsaicin to other areas. Tolerability of capsaicin in the elderly may be a problem.
The lidocaine 5% patch has been shown to be easy to use, safe, tolerable, and efficacious in the management of PHN pain. Lidocaine is an amide-type local anesthetic agent that stabilizes neuronal membranes by inhibiting the ionic fluxes required for the initiation and conduction of impulses. In patients with PHN, the lidocaine 5% patch has demonstrated relief of pain and tactile allodynia with a minimal risk of systemic adverse effects or drug—drug interactions. Because of its proven efficacy and safety profile, the lidocaine 5% patch has been recommended as a first-line therapy for the treatment of PHN pain.12 The systemic absorption of lidocaine from the patch is minimal in healthy adults even when applied for up to 24 hours, and lidocaine absorption was even lower among patients with PHN than among healthy adults at the recommended dosage. The highest blood lidocaine level measured was 0.1 mcg/mL, indicating minimal systemic absorption of this agent. Lidocaine-containing patches significantly reduce pain intensity throughout the dosing interval for up to 12 hours. Lidocaine patches were superior to both no treatment and vehicle patches in averaged category pain relief scores. Most adverse events were at patch application sites. No clinically significant systemic adverse effects were noted, including when used long-term or in an elderly population.
Oral Agents
Tricyclic Antidepressants: Tricyclic antidepressants (TCAs) are effective adjuncts in the management of PHN pain.13 TCAs inhibit the membrane pump mechanism responsible for uptake of norepinephrine and serotonin in adrenergic and serotonergic neurons. Pharmacologically, this action may potentiate or prolong neuronal activity since reuptake of these biogenic amines is important physiologically in terminating transmitting activity. TCAs relieve PHN pain by stabilizing nerve pathways that have undergone degeneration and interruption due to herpes zoster infection. TABLE 2 shows commonly used TCAs in the management of PHN. TCA therapy should be initiated with low doses to improve tolerability and be administered at bedtime. The dose can be titrated every 2 to 4 weeks until maximum tolerated dose to achieve results. TCAs act slowly and may require up to 3 months before achieving adequate response in patients. Combining TCAs with antiviral drugs during herpes zoster infection has been shown to decrease the intensity of PHN pain but does not prevent it. The main side effects expected from TCA therapy are sedation, dry mouth, postural hypotension, blurred vision, and urinary retention. These side effects are related to the anticholinergic activities of TCAs. Nortriptyline tends to produce less anticholinergic effects and is better tolerated. Cardiac conduction impairment or liver toxicity may develop in some patients, especially in elderly patients or those at high risk.
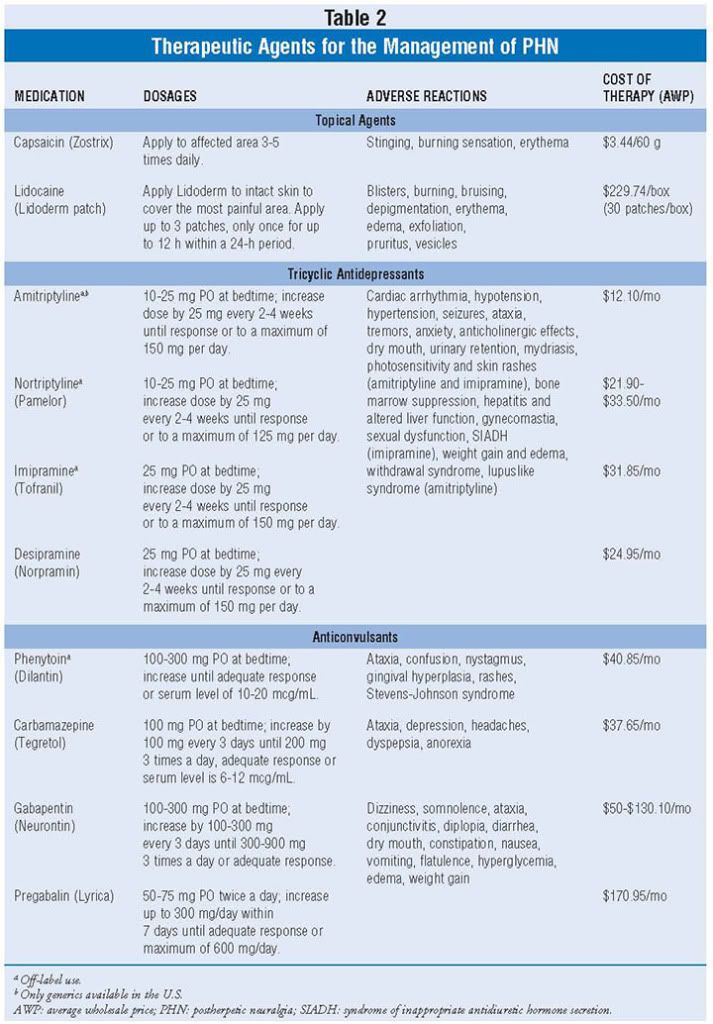
Anticonvulsants: Phenytoin, carbamazepine, gabapentin, and pregabalin are useful to control PHN pain.14,15 Phenytoin is an anticonvulsant drug related structurally to barbiturates. Phenytoin produces its beneficial effect in PHN through its antinociceptive activity. The side effects to be concerned about, especially in the elderly, include nystagmus, ataxia, skin eruptions, hematological complications, and gingival hyperplasia.
Carbamazepine greatly reduces or abolishes pain induced by stimulation of the nerve. It depresses thalamic potential and bulbar and polysynaptic reflexes. Carbamazepine is chemically unrelated to other anticonvulsants or other drugs used to control PHN pain. The drawback to using carbamazepine is the serious and sometimes fatal dermatologic reactions, including toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome. These dermatologic adverse events commonly affect patients of Asian ancestry. Also, severe blood disorders such as aplastic anemia and agranulocytosis may occur. Complete baseline and periodic hematologic monitoring for the patient is essential.
Gabapentin prevents allodynia and hyperalgesia associated with PHN pain as well as the associated sleep disorder. Gabapentin is structurally related to the neurotransmitter gamma-aminobutyric acid (GABA), but it does not bind directly to GABAA or GABAB receptors. The adverse events with its use are dizziness, somnolence, and peripheral edema.
Pregabalin is a structural derivative of the neurotransmitter GABA and does not bind directly to GABAA or GABAB receptors. It binds with high affinity to the alpha2-delta site (an auxiliary subunit of voltage-gated calcium channels) in central nervous system tissues to produce antinociceptive effects.
Anticonvulsants have been shown to be equally efficacious; however, drug selection may involve trial and error. If there is inadequate response to one anticonvulsant agent, another agent should be tried. Doses required for the analgesic activity are lower than those used to treat seizures. These agents may be combined with TCAs or the lidocaine patch to improve pain relief. The risk of side effects, however, is increased with the use of multiple medications. The side effects that are associated with anticonvulsants include sedations memory disturbance, electrolyte abnormalities, liver toxicities, and thrombocytopenia. These side effects can be minimized by initiating therapy with low doses and slowly titrating doses upward over several weeks.
Opioid Analgesics: Opioids such as codeine, oxycodone, and morphine provide PHN pain relief by their interaction with opioid receptors in the central nervous system.16 Specifically, they provide pain relief through inhibition of the ascending transmission of nociceptive signals, activation of descending inhibitory pain pathways, and modulation of limbic system activity. Opioid analgesics in combination with acetaminophen or nonsteroidal anti-inflammatory drugs may be useful as a last resort in patients with severe PHN pain unrelieved by other drugs. Opioid analgesic side effects include nausea, vomiting, constipation, dizziness, headache, and respiratory depression. Long-term use is of concern because of the abuse potential. Tramadol, a centrally active synthetic opioid analgesic, is a useful alternative because it lacks the abuse potential associated with other opioids.
Other Interventions
Transcutaneous Electric Nerve Stimulation: The application of electrical current through the skin for pain relief is known as transcutaneous electrical nerve stimulation (TENS). TENS has been shown to be beneficial in the management of PHN pain.17 TENS produces analgesic effects by activation of opioid receptors in the central nervous system. High-frequency TENS activates delta-opioid receptors both in the spinal cord and supraspinally (in the medulla), while low-frequency TENS activates mu-opioid receptors both in the spinal cord and supraspinally. Further, high-frequency TENS reduces excitation of central neurons that transmit nociceptive information, reduces release of excitatory neurotransmitters (glutamate), increases the release of inhibitory neurotransmitters (GABA) in the spinal cord, and activates muscarinic receptors centrally to produce analgesia by temporarily blocking the pain gate.
Biofeedback: Patients may use biofeedback techniques that employ the mind to control body functions such as skin temperature, muscle tension, heart rate, and blood pressure.18 Biofeedback may also be used to control problems such as chronic pain. There are two types of biofeedback techniques. The first type is electromyography. This type uses a device that measures muscle tension while the patient practices a relaxation technique such as meditation, progressive muscle relaxation, or visualization. The second technique is hand-temperature biofeedback. This type of biofeedback uses a device that measures the skin temperature of the hand. Patients can decrease their pain by increasing their body temperature through visualization or guided imagery.
Nerve Block: Nerve block injections have been shown to be useful in the management of PHN pain. Nerve blocks provide periods of dramatic pain relief, which promotes the desensitization of sensory pathways. In this technique, local anesthetics, steroids, and opioid medications are injected around the affected nerve to relieve pain. The nerve block with anesthetic may relieve PHN pain for several days, but the pain often returns.19 Nerve block injections need to be repeated several times over the course of a week to be effective.
Herpes Zoster Vaccine: The medical and social costs of shingles and PHN are high, particularly in elderly people. The outcome of treatment of shingles is often unsatisfactory, although the antiviral medications reduce the duration of pain during the acute phase but do not prevent PHN complications and pain. A live, attenuated vaccine has been shown to reduce the incidence of shingles and PHN as well as reduce the burden of the illness in patients older than 60 years.20 The zoster vaccine licensed in the United States (Zostavax, Merck) is a lyophilized preparation of the Oka/Merck strain of live, attenuated varicella zoster virus, the same strain used in the varicella vaccines (Varivax, Proquad). The Oka strain was isolated in Japan in the early 1970s from vesicular fluid from a healthy child who had varicella; the strain was attenuated through sequential propagation in cultures of human embryonic lung cells, embryonic guinea pig cells, and human diploid cells (WI-38).21 Further passage of the virus was performed at Merck Research Laboratories in human diploid cell cultures (MRC-5). The cells, virus seeds, virus bulks, and bovine serum used in the manufacturing are all tested to provide assurance that the final product is free of adventitious agents. The CDC Advisory Committee on Immunization Practices recommends routine vaccination of all persons age >60 years with one dose of zoster vaccine. Persons who report a previous episode of zoster and persons with chronic medical conditions (e.g., chronic renal failure, diabetes mellitus, rheumatoid arthritis, and chronic pulmonary disease) can be vaccinated unless those conditions are contraindications or precautions. Zoster vaccination is not indicated to treat acute zoster, to prevent persons with acute zoster from developing PHN, or to treat ongoing PHN. Before routine administration of zoster vaccine, it is not necessary to ask patients about their history of varicella (chickenpox) or to conduct serologic testing for varicella immunity.
In conclusion, age is the most important risk factor for developing shingles. More than 50% of the people who live to be 85 years old will develop shingles, and 80% to 85% of PHN complication occurs in patients older than 50 years. Thus, early management of shingles is essential to prevent the many complications, especially the chronic, debilitating, difficult-to-treat PHN pain that often results from the condition.
REFERENCES
- Johnson RW, Wasner G, Saddler P, et al. Herpes zoster and postherpetic neuralgia: optimizing management in the elderly. Drugs Aging. 2008;25(1):991-1006.
- Choo PW, Galil K, Donahue JG, et al. Risk factors for postherpetic neuralgia. Arch Intern Med. 1997;157:1117-1124.
- Straw SE. Overview of the biology of varicella zoster virus infection. Ann Neurol. 1994;35(suppl):S4-S8.
- Stankus SJ, Dlugopolski M, Packer D. Management of herpes zoster (shingles) and post herpertic neuralgia. Am Fam Physician. 2000;61:2437-2444.
- Gudmindsson S, Helgason S, Sigurdsson JA. The clinical course of herpes zoster: a prospective study in primary care. Eur J Gen Pract. 1996;2:12-16.
- Oaklander AL. Mechanism of pain and itch caused by herpes zoster shingles. J Pain. 2009;9(suppl):S10-S18.
- Langston P. Herpes zoster antivirals and pain management. Opthalmology. 2008;115(suppl 2):S13-S20.
- MacFarlane LL, Simmons MM, Hunter MH. The use of corticosteroids in the management of herpes zoster. J Am Board Fam Pract. 1998;11:224-228.
- Mcfarlane LL, Simmons MM, Hunter MH. The uses of corticosteroids in the management of herpes zoster. J Am Board Fam. 1998;11:224-228.
- Zin CS, Nissen LM, Smith MT, et al. An update on the pharmacological management of post herpetic neuralgia and painful diabetes neuropathy. CNS Drugs. 2008;22(5):417-442.
- Watson CP, Tyler Kl, Bickers DR, et al. A randomized vehicle controlled trial of topical capsaicin in the treatment of postherpetic neuralgia. Clin Ther.1993;15:510-526.
- Lin Pl, Fan SZ, Huang CH, et al. Analgesic effect of lidocaine patch 5% in the treatment of acute herpes zoster: double blind and vehicle controlled study.Reg Anesth Pain Med. 2008;33(4):320-325.
- Davis PS, Galer BS. Review of lidocaine 5% patch studies in the treatment of post herpetic neuralgia. Drugs. 2004;64(9):937-947.
- Wu CL, Raja SN. An update on the treatment of postherpetic neuralgia. J Pain. 2008;9(suppl 1):S19-S30.
- Beydoun A. Postherpetic neuralgia: role of gabapentin and other treatment modalities. Epilepsia. 1999;40(suppl 6):S51-S56.
- Watson CP, Babul N. Efficacy of oxycodone in neuropathic pain: a randomized trial in postherpetic neuralgia. Neurology. 1998;50(6):1837-1841.
- Tulgar M. Advances in electrical nerve stimulation techniques to manage chronic pain: an overview. Adv Ther. 1992;9(6):366-372.
- Ahmad M, Goucke CR. Management strategies for treatment of neuropathic pain in the elderly. Drugs Aging. 2002;19(12):929-945.
- Ashkenazi A, Levin M. Three common neuralgias: how to manage trigeminal, occipital, and postherpetic pain. Postgraduate Medicine. 2004;116(3):16-48.
- Johnson R, McElhaney J, Pedalino B, et al. Prevention of herpes zoster and its painful and debilitating complications. Int J Infect Dis. 2007;22(suppl 2):S43-S48.
- Takahashi M, Otsuka T, Okuno Y, et al. Live vaccine used to prevent the spread of varicella in children in hospital. Lancet. 1974;2:1288-1290.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 