From Expert Review of Clinical Pharmacology
Pancreatic Cancer: Advances in Medical Therapy
Andrew Weickhardt; Michael Michael
Published: 07/06/2009
Abstract
Progress in the treatment of pancreatic cancer has been notably slow and modest in contrast to other cancers of the GI tract over the last 5 years. Pancreatic cancer still continues to be a devastating illness that is marked by the appearance of early metastatic disease, despite curative surgery and the relative chemoresistance of the disease. However, small incremental benefits have been seen, and point to areas of research and development over the subsequent years. Developments in adjuvant chemotherapy and the use of gemcitabine in combination with other cytotoxic agents or with biological agents have changed clinical practice. Given its poor outlook and the paucity of active therapies, even modest gains can lead to regulatory approval and, therefore, pancreatic cancer represents a common target for pharmaceutical companies. Newer agents are in development with the promise of further refinement in treatment selection based on molecular tumor characteristics.
Adjuvant Chemotherapy
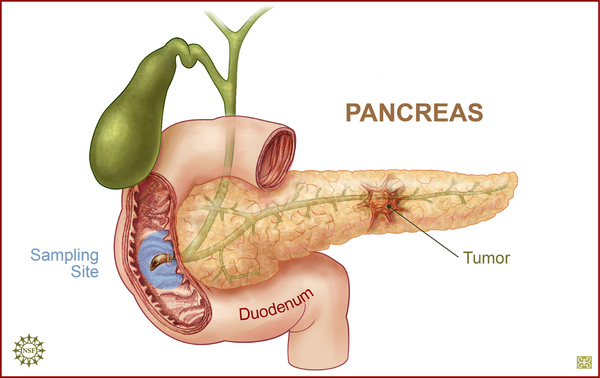
A significant development in pancreatic cancer is the maturation of data showing support for adjuvant chemotherapy in resected localized disease. Surgical resection offers the only chance of cure in patients with localized disease;[1] however, only 20% of cases are potentially resectable. Even then, prognosis is poor in patients with resected disease, with 5-year survival rates of between 10 and 25%.[2]
The weight of evidence to show the role of postoperative chemotherapy in patients with resected pancreatic cancer emerged from two randomized Phase III trials. The first was the European Study Group for Pancreatic Cancer (ESPAC)-1 trial,[3] which was constructed to answer, with a 2 × 2 factorial design, the relative benefit of chemotherapy and also chemoradiation in patients with resected pancreatic cancer, utilizing a 5-fluorouracil (5FU) backbone. The trial demonstrated a survival advantage of 6 months (19.7 vs 14 months) for the postoperative chemotherapy arm. However, there were major flaws with this trial. These include the fact that physicians and patients chose which treatment they would be allocated, the delivery of 'background' chemoradiation or chemotherapy, regardless of the arm patients were randomized to, and the lack of quality control for surgery and radiotherapy.[3] Despite these shortcomings, there were some important useable messages. Chemoradiation seemed to have no advantages, with possibly a detrimental effect, with a median survival of 15.5 versus 16.1 months. The 5-year survival rates were also much higher in the group receiving chemotherapy compared with chemoradiotherapy (21 vs 8%). A smaller trial randomizing patients to postoperative adjuvant combination chemotherapy, 5FU, doxorubicin, mitomycin C (AMF; n = 30) once every 3 weeks for six cycles, or into an observation group (n = 31), also showed a significant increase in median survival (23 vs 11 months); however, 5-year survival rates were similar (8 vs 4%).[4] The role of adjuvant 5FU in pancreatic cancer is further supported by a recently published meta-analysis that looked at the results from ESPAC-1 and similar trials.[5] The pooled hazard ratio (HR) of 0.70 (95% confidence interval [CI]: 0.55-0.88; p = 0.003) and the median survival of 23.2 months (95% CI: 20.1-26.5) with 5FU/folinic acid (FA) vs 16.8 months (95% CI: 14.3-19.2) with resection alone further supports the use of adjuvant 5FU/FA in pancreatic cancer.[5]
The second recently published important trial of adjuvant therapy is Charite Onkologie (CONKO)-001,[6] which aimed to compare postoperative gemcitabine with observation alone in patients with fully resected pancreatic cancer. It involved 368 patients, and randomized patients on the treatment arm to six cycles of gemcitabine 1000 mg/m2 on days 1, 8 and 15 of a 4-weekly cycle. The updated data show a 5-year survival rate of 21% in the gemcitabine arm versus 9% in the observation arm.[7] The median survival was 22.8 versus 20.2 months, with a disease-free interval of 13.4 versus 6.9 months in the observation arm, both of which were statistically significant results (p < 0.001). Patients were stratified by resection margins and also nodal status, and chemotherapy was also associated with significant improvements in the above measures. The terminal tail of the overall survival (OS) curve suggests that, although the median survival difference is not large, there is a significant group of long-term survivors who benefit from the use of gemcitabine in the postoperative setting.[7]
There have not been adequate trials to answer whether neoadjuvant chemotherapy is superior to adjuvant therapy for the treatment of patients with resectable pancreatic cancer. While neoadjuvant chemotherapy has theoretical advantages, such as increasing resectability and allowing those patients with rapidly progressive chemotherapy-refractory disease to declare themselves prior to operation, there have been no direct comparisons. Almost all the neoadjuvant trials have used chemoradiotherapy and have had small numbers of patients and, therefore, lack adequate statistical power to be recommend as routine care for this condition.[8,9]
This approach with adjuvant chemotherapy has been followed mostly in Europe, rather than the American approach of adjuvant chemoradiotherapy. As with the debate between neoadjuvant and adjuvant therapy, this debate has been shaped by small, underpowered studies that enable few firm conclusions. The Gastrointestinal Tumor Study Group (GITSG) trial managed to only recruit 43 patients, and randomized patients to observation only or 5FU-based chemoradiotherapy followed by adjuvant chemotherapy. Despite the low numbers of patients, there was a significant survival benefit for the chemoradiation group, at 20 compared with 11 months.[10]
No trial has compared 5FU-based chemoradiotherapy with gemcitabine-based treatment, but the Radiation Therapy Oncology Group (RTOG) 9704 trial evaluated the benefit of adding gemcitabine pre- and post-5FU chemoradiotherapy after surgical resection relative to the 5FU pre- and postchemoradiotherapy.[11] There was a modest benefit in improvement in median survival (20.5 vs 16.9 months; p = 0.09) that favored the gemcitabine arm in those patients with pancreatic head tumors.[11] The ESPAC-3 trial comparing adjuvant gemcitabine with adjuvant fluorouracil is currently ongoing and its results may guide clinicians in their choice of adjuvant therapy.
Whether chemotherapy alone is superior to chemoradiotherapy in the adjuvant setting is still to be answered in an adequately powered and well-executed and -designed randomized trial. Future trials are necessary to ascertain when the chemotherapy should be given, what the best chemotherapy regimen is and what the contribution of radiotherapy is to the adjuvant treatment plan. Identifying those patients at high risk of disease relapse in the future will need to be based on both well-characterized and validated clinical and potential molecular markers.
Systemic Treatment of Pancreatic Cancer
Benefit of Chemotherapy
The interpretation of the clinical trials in pancreatic cancer requires an understanding that many of the trials enrolled both locally advanced and metastatic cancer patients, and that many of the trials were underpowered. Whether locally advanced patients should be evaluated separately has not been clarified, this is despite randomized trials observing a longer OS for these patients relative to the metastatic cohort.[12]
Promising Phase II trials results have not been confirmed in the larger Phase III settings. Response rates have been more difficult to interpret than other tumor types as the cancer often causes an inflammatory response and desmoplastic reaction in the surrounding tissues, which make accurate radiological assessment difficult. More recently, trials have incorporated quality of life and 'clinical benefit' as objective end points, which have shown discrepancies between the tumor size response and these more patient-focussed variables.[13]
Single-agent 5FU or Gemcitabine
The outlook for untreated metastatic pancreatic cancer is poor, and early trials had demonstrated only very modest improvements with 5FU-based chemotherapy over best supportive care.[14,15] These trials used other drugs, such as adriamycin, mitomycin or etoposide,[16] in combination with 5FU, and achieved median survivals of between 6 and 12 months, which is much greater than that seen with most trials of single-agent 5FU.[17] A Cochrane meta-analysis has supported the benefits of chemotherapy over supportive care,[18] with a reduction in the risk of death of 37% at 1 year (95% CI: 0.25-0.57), which is similar to the 36% reduction found in a more recent meta-analysis.[19]
After 5FU, the next advance in this area has been the use of gemcitabine, a pyrimide analogue that inhibits DNA synthesis by an inhibition of DNA polymerase and ribonucleotide reductase. Gemcitabine was evaluated in a Phase II trial of patients with prior therapy with 5FU. The primary end point was clinical benefit response, which is defined as:
- At least a 50% reduction in pain intensity
- At least a 50% reduction in daily analgesic consumption
- At least a 20-point improvement in Karnofsky Performance Status (KPS) that was sustained for at least 4 consecutive weeks
In total, 17 out of 63 patients (27.0%) attained a clinical benefit response (95% CI: 16.0-38.0%). The median duration of clinical benefit response was 14 weeks (range: 4-69 weeks). The median survival for patients treated with gemcitabine was 3.85 months (range: 0.3-18.0+ months). Therapy was generally well tolerated with a low incidence of grade 3 or 4 toxicities.[20]
A subsequent Phase III trial randomized patients with chemo-naive advanced pancreatic cancer to single-agent 5FU versus single-agent gemcitabine, the results of which subsequently led to the registration of gemcitabine as first-line therapy in this disease.[13] Despite 5FU being given without leucovorin, and at a nonstandard dose of 600 mg/m2/week as a bolus, the 126-patient trial was able to demonstrate an increased 1-year survival (18 vs 2%) in favor of gemcitabine. There was also a favorable clinical benefit response of 24 versus 5%. The median survival was 5.65 months in the gemcitabine cohort versus 4.41 months in the 5FU group.[13] The results were considered to be significant enough, in particular the improved survival, to warrant widespread approval of gemcitabine in this disease.
Gemcitabine requires intracellular phosphorylation catalyzed by the enzyme deoxycytidine kinase for its activation; the reaction is rate limiting. The agent is normally given as a 30-min infusion; however, changing the infusion time to a fixed dose rate (FDR) infusion may increase the extent of intracellular phosphorylation and, thus, enhance its activity. Given that the enzyme is saturated at rates of approximately 10 mg/m2/min,[21] the FDR dosing can give a maximum-tolerated dose, such as 4800 mg/m2 over 480 min. This method has been evaluated in several early Phase I and II trials; however, this theoretical benefit has not been translated to a clinical benefit in larger trials.
For instance, the Phase II trial of standard infusion of gemcitabine at a dose of 2200 mg/m2 was compared with a FDR infusion of gemcitabine at 1500 mg/m2 at 10 mg/m2/min (i.e., over 150 min) showed a median survival in the standard arm of 5.0 versus 8.0 months in the FDR arm (p = 0.013). The 2-year survival was significantly better in the FDR arm: 18.3 versus 2.2% (p = 0.046).[22] However, an interim report of the Intergroup study in 2006 failed to confirm the benefit of this strategy.[23] In this study, 833 patients with advanced pancreatic cancer were randomized to standard gemcitabine given at 1000 mg/m2 over 30 min, FDR gemcitabine 1500 mg/m2 at 10 mg/m2/min or a third arm that contained gemcitabine plus oxaliplatin. There were no significant differences in response rates and there was only a trend towards improved survival of 4.9 versus 6 months of the standard versus the FDR arm, respectively (HR: 1.21 with a stratified log rank of 0.053).[23] Given these results, there has not been an adaption of this scheduling to the clinical use of gemcitabine.
Further work has been conducted into elucidating the population that may derive the most benefit from gemcitabine. Gemcitabine requires equilibrative nucleoside transporters (hENTs) and concentrative nucleoside transporters (hCNTs) for transport into the cell.[24,25]
In vitro studies suggest that gemcitabine is mostly reliant on hENT1s[26] and that high expression of hENT1 is associated with survival benefit in pancreatic cancer patients.[27]
Other relationships have also been observed with the activity of the gemcitabine catabolic and metabolic enzymes. The levels of deoxycytidine kinase (dCK) has been correlated with sensitivity to gemcitabine.[28] A further important enzyme is cytidine deaminase (CDA), which inactivates gemcitabine. As expected, high levels of this enzyme have been correlated with gemcitabine resistance.[29]
At present, there is a paucity of reliable consistent genetic data in this regard.[30,31] In one promising study, single-nucleotide polymorphisms (SNPs) in the DNA damage response/repair genes were observed to have had a significant impact on the OS.[32] Overall, 13 SNPs of eight DNA damage response/repair genes in 92 patients with potentially resectable pancreatic adenocarcinoma were analyzed.[32] All patients were treated with neoadjuvant concurrent gemcitabine and radiotherapy.[32] Overall, four genotypes had a significant effect on OS with log-rank p-values of less than 0.02. Patients with none of the adverse genotypes had a mean survival time of 62.1 months, while those with one, two or three or more at-risk alleles had median survival times of 27.5, 14.4 and 9.9 months, respectively (log-rank p < 0.001).[32]
Another study of 126 patients with resectable pancreatic cancer treated with neoadjuvant gemcitabine-based chemotherapy plus radiation analyzed SNPs of similar enzymes with regards to treatment outcomes.[25] Specifically, there was a significant combined genotype effect on OS observed for the metabolic or target gene SNPs CDA111CC, CDA-76AA, RRM1 42GG and DCTD-47CT (p < 0.001) and for the transporter gene SNPs hCNT1-16AA/AG, hCNT2-17CC and hENT1 913CC (p = 0.006). CDA 111C and dCK-1205TT alleles were associated with poorer survival but less treatment toxicity.[25]
These results could now be potentially utilized in upcoming trials to stratify patients based upon their predicted response to gemcitabine. Hence, trials could be designed to answer the question of whether the subgroup predicted to have a poor response to gemcitabine would benefit from an alternative first-line chemotherapy.
Gemcitabine & Cytotoxic Doublets
Not surprisingly, much effort has gone into improving this dismal survival rate, mostly by using gemcitabine as a comparator to other agents or in combination with these newer drugs. The more promising of these latter efforts include the combination of gemcitabine with a platinum, such as cisplatin or oxaliplatin, as well as the combination of gemcitabine with capecitabine ( Table 1 ).
Table 1. Potential Cytotoxic Drugs to Use With Gemcitabine

Among the disparate data on the benefits of combination therapy with platinum analogues, the most compelling comes from the pooled analysis of two separate trials that used either cisplatin[33] or oxaliplatin.[34] The pooled analysis showed benefits in progression-free survival (PFS; HR: 0.75; p = 0.003) and OS (HR: 0.81; p = 0.031) that were significantly in favor of the combination group.[35]
A meta-analysis is only as good as the trials that are included. These results need to be interpreted cautiously in the light of two other Phase III trials not included in this analysis that do not show an advantage when cisplatin is combined with gemcitabine compared with gemcitabine alone.[36,37] Additionally, there have been two other trials of gemcitabine with oxaliplatin that have not shown significant improvements in OS over gemcitabine alone.[23,34] Two separate meta-analyses support the view that there is no significant improvement in survival when using either cisplatin or oxaliplatin.[18,38] Currently, the combination cannot be recommended, except in the case of younger patients with a good performance status.
Gemcitabine has been used in combination with 5FU in several trials and, more recently, with the oral 5FU prodrug capecitabine. A meta-analysis evaluating the benefit of these combinations showed that there was no significant improvement with the addition of 5FU in the three trials of this combination (n = 879); HR: 0.98; 95% CI: 0.86-1.11).[19] By contrast, the results seemed favorable for the capecitabine combination (three trials, n = 935); HR = 0.83; 95% CI: 0.72-0.96).[19] The most favorable of these three trials is the UK NCRI GEMCAP study, which enrolled 533 patients.[12] This demonstrated a median survival of 7.4 months in the gemcitabine-capecitabine arm, compared with 6.0 months with gemcitabine alone, with a response rate of 14.2 versus 7.1% (p = 0.008). The trial was presented at the European Cancer Conference in 2005; as yet, it has not yet been fully published.
These promising results were not replicated in the only published Phase III Swiss and Central European Cooperative Group (CECOG) trial of the combination of gemcitabine and capecitabine.[39] This trial enrolled 319 patients and showed no significant differences in survival between the two groups (8.4 vs 7.3 months; p = 0.234). This trend may have been significant as the trial was possibly underpowered. Post hoc analysis was required to find a subgroup that derived a statistical benefit from the combination: those patients with a good KPS score (90-100) who had a median OS of 10.1 versus 7.4 months (p = 0.014). The response rates were 15 versus 12%, respectively, for the combination versus single-agent gemcitabine. There were no significant differences in toxicity between the two groups. Apart from being possibly underpowered, another reason for the discrepancy in the results between the two trials is the difference in capecitabine dosing. The GEMCAP study used 1660 mg/m2/day for 21 days every 4 weeks, but the Swiss Group used 1300 mg/m2/day for 14 days of a 21-day cycle.[39] The Swiss group have subsequently published an update on their study, which did not show any significant difference in quality of life between the combination and single-agent arms of their trial.[40]
Gemcitabine & Biological-targeted Therapy Doublets
The area of most interest in recent years, as with most other areas in oncology, has been developing targeted therapy for pancreatic cancer. The most promising of these efforts are those that target the EGF receptor (EGFR) or the VEGF. Although many other strategies have been trialled and are in the pipeline, none have so far shown results that have moved them from research into the clinical domain. The major trial highlights of such an approach will be considered below, in addition to the weaknesses of current trial design.
The rationale for targeting the EGFR grew from the observation that many pancreatic cancers overexpress the receptor, which is an adverse prognostic factor.[41-43] The EGFR signals through downstream pathways including the K-ras protein. Mutations of the K-ras gene are present in approximately 90% of pancreatic cancers, which is higher than any other solid organ cancers.[44] However, recent studies in colorectal cancer[45] and lung cancer[46] have shown that tumors bearing the K-ras mutation do not benefit from therapies that target the EGFR, and the same resistance is likely to apply to pancreatic cancer. This information was not known when trials were designed targeting the EGFR, and future research may point to only a small subgroup of patients that benefit from this approach, bringing forward this class of agents into mainstream clinical practice.
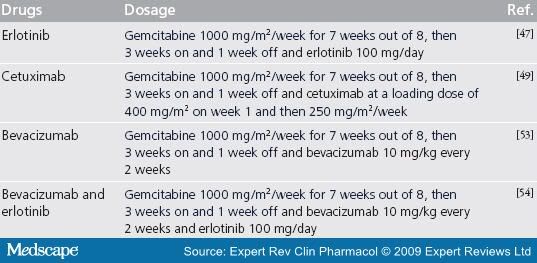
Although trials targeting the EGFR in pancreatic cancer have at best produced modest statistically significant results, these are not results that the majority of oncologists would accept as clinically significant. The most widely reported of these trials was the National Cancer Institute of Canada (NCIC) trial[47] that compared gemcitabine alone or combined with erlotinib 100 mg daily. The trial included patients with locally advanced and metastatic disease, and enrolled 569 patients. There were no differences in response rates. Although survival at 1 year was improved with the combination (23 vs 17%; p = 0.023), the median survival was modestly improved (6.24 vs 5.91 months; p = 0.038). There was a 6% incidence of grades 3 and 4 skin rash versus 1% in the treatment arm with erlotinib, as well as a similar increase in the rate of grades 3 and 4 diarrhea. There has not yet been a retrospective review of the pathology published to see if response and clinical benefit was confined to the predicted small number of patients who were K-ras wild-type or those with an increased EGFR gene copy number or gene mutation.
Cetuximab is a chimeric human-mouse monoclonal antibody (mAb) directed against the EGFR1. A Phase II trial in patients with EGFR-expressing pancreatic cancer treated with a combination of cetuximab and gemcitabine showed a response rate of 12.2% with a median survival of 7.1 months.[48] This led to the Phase III South West Oncology Group S0205 trial comparing this combination with single-agent gemcitabine.[49] Disappointingly, the OS was not significantly changed in this large 735-patient trial (6.4 vs 5.9 months). Similarly, the PFS was also not significantly different (3.5 vs 3.0 months). Again, further analysis on the basis of K-ras mutation status has not yet been reported, but would prove valuable in identifying a subset of patients most likely to benefit from the cetuximab combination.
Another approach to targeted therapy in pancreatic cancer is the use of the antiangiogenic agents. Some preclinical work suggests that pancreatic cancer cell lines overexpress VEGF, and that targeting this receptor and pathway may suppress the growth of pancreatic cancer.[50] VEGF receptors (VEGFRs) are transmembrane proteins that have tyrosine kinase activity and are located predominantly on the surface of endothelial cells. Signaling via VEGF to the VEGFR regulates angiogenic development in tumors,[51] and is a pathway that has been the subject of much preclinical and clinical progress in many other cancers.
The humanized mAb to VEGF, bevacizumab, showed potential in a Phase II trial when it was combined with gemcitabine.[52] The trial enrolled 52 patients and combined fortnightly bevacizumab at 10 mg/kg with gemcitabine 1000 mg/m2 given on days 1, 8 and 15 every 28 days. All patients had metastatic disease. The median survival was 8.8 months, leading investigators to develop a Phase III trial that unfortunately did not confirm superiority over standard gemcitabine.[53] In this larger trial of 602 patients, the median survival was 5.7 months in the combination arm versus 6.0 months in the single-agent arm. The response rates and disease control rate were similar. Presumably, the higher proportion of better performance status patients in the Phase II trial could explain the discrepancy in the data between the trials.[53]
Despite this failure to confirm benefit of bevacizumab, a Phase III trial was completed in an effort to analyze the additional benefit bevacizumab would add to the combination of erlotinib and gemcitabine, which, as discussed earlier, had shown a very small benefit over gemcitabine alone. The trial was reported at the American Society of Clinical Oncology meeting in 2008,[54] and had enrolled 607 patients beginning in 2005 before the disappointing results of the Kindler trial were published. Although there was not a benefit in OS (6.0 vs 7.1 months; HR: 0.74-1.07), there was a statistically significant improvement in PFS favoring the bevacizumab arm (3.6 vs 4.6 months; p = 0.0002). The response rate was 8.6% in the gemcitabine-erlotinib arm versus 13.5% in the bevacizumab-containing arm. Thrombotic events were similar in both groups and gastrointestinal perforations were uncommon in both groups. The lack of meaningful clinical improvement makes it unlikely that bevacizumab will have a role for clinical management of pancreatic cancer patients in the future unless good predictive biomarkers can enrich the target population to receive this costly medication in pancreatic cancer.
Other drugs that target the angiogenic pathway include the small-molecule tyrosine kinase inhibitors. These include axitinib,[55] which is an oral potent inhibitor of VEGFR1, 2 and 3. Axitinib was added to gemcitabine in an underpowered, small, randomized Phase II trial of 103 patients that showed a nonsignificant trend towards improved survival using combination therapy (6.9 vs 5.6 months). Grade 3 fatigue was significantly increased in the combination arm (15 vs 3%). It is unclear whether the fate of axitinib in the Phase III trial will be similar to that of bevacizumab, as the Phase III trial is still recruiting (clinicaltrials.gov ID NCT00471146),[101] with an estimated completion date of August 2009.[55]
Valatanib is similar to axitinib and is an oral pan VEGFR tyrosine kinase inhibitor that targets VEGFR1, 2 and 3. A Phase I/II trial of valatanib and gemcitabine is currently recruiting patients.[56] The trial has enrolled 26 patients evaluable for toxicity and response with ten patients in the Phase II component. Phase I dose-limiting toxicities include diarrhea, hypokalemia, neutropenia, fatigue and thrombosis. Three out of 26 patients (12%) had a partial response by response evaluation criteria in solid tumors (RECIST). The remaining patients had stable disease as the best response (62%) for a period ranging from 2 to 6 months.[56]
Sorafenib is a multitargeted oral tyrosine kinase drug that has inhibitory effects of Raf-1, VEGFR2/3, PDGF receptor, FLT-3 and c-KIT. A Phase II trial of sorafenib plus gemcitabine in advanced pancreatic cancer had 17 patients enrolled.[57] The median OS was 4 months, and there were no objective responses. Thus, there appears to be no role for sorafenib in metastatic pancreatic cancer ( Table 2 ).
[ CLOSE WINDOW ]
Table 2. Potential Targeted Drugs to Use With Gemcitabine
Expert Commentary
Pancreatic cancer still remains a difficult disease to treat with much progress needed to improve survival beyond its current dismal state. Surgery remains the only possibility for cure, and adjuvant chemotherapy has been shown to have a role. Palliative chemotherapy has traditionally revolved around single-agent gemcitabine, and clinical trials have focused on the addition of cytotoxics and other biological agents to this, with underwhelming results. Although the addition of a platinum agent or capecitabine, or the addition of erlotinib or bevacizumab to gemcitabine, have all been shown in respective trials to have, at best, modest benefits in survival at 1 year that border on statistical significance, there have equally been other trials that have suggested the futility of adding these agents, and they have yet to be accepted into clinical oncology.
Five-year View
Rational trial design centered around plausible biological agents with prespecified biomarkers are the future of pancreatic cancer trials and, potentially, this will translate into clinical practice. Prerandomization stratification on this basis may enable derivation of enriched populations that derive maximal benefit from new agents, while sparing toxicity to those destined to not respond. Further trials are also likely to reject the notion that new agents must be added to gemcitabine, as often required by regulatory authorities, and allow direct comparisons with single-agent gemcitabine with trials large enough to derive statistically significant answers. Many pathways are potential targets for pancreatic cancer, but their translation to clinical utility depends on better trial design and biomarker use. Until this happens, it seems unlikely that there will be a revolutionary approach to the disease.
Key Issues
- Adjuvant gemcitabine chemotherapy significantly prolongs survival after surgical resection, creating a sizable difference in long-term survivors.
- Single-agent gemcitabine is still considered the gold standard for treatment of metastatic pancreatic cancer.
- The addition of capecitabine or a platinum cytotoxic to gemcitabine offers marginal benefits in terms of survival.
- Targeting the EGF receptor has shown some statistical significant improvements when using erlotinib in addition to gemcitabine; however, the clinical improvement is marginal.
- The angiogenesis pathway may also be targeted; however, the only trial to show statistical significant results used gemcitabine in combination with erlotinib and bevacizumab, which is a costly combination that had very minor improvements in survival.
- Further research is needed into biomarker use to enrich the population of pancreatic cancer agents used in clinical trials.
[ CLOSE WINDOW ]
References
- 1. Doi R, Imamura M, Hosotani R et al. Surgery versus radiochemotherapy for resectable locally invasive pancreatic cancer: final results of a randomized multi-institutional trial. Surg. Today 38,1021-1028 (2008).
- 2. Hawes RH, Xiong Q, Waxman I et al. A multispecialty approach to the diagnosis and management of pancreatic cancer. Am. J. Gastroenterol. 95,17-31 (2000).
- 3. Neoptolemos JP, Stocken DD, Friess H et al. A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. N. Engl. J. Med.350,1200-1210 (2004).
Large randomized trial of adjuvant therapy that established 5-fluorouracil (5FU) as an important treatment option. - 4. Bakkevold KE, Arnesjo B, Dahl O et al. Adjuvant combination chemotherapy (AMF) following radical resection of carcinoma of the pancreas and papilla of Vater - results of a controlled, prospective, randomised multicentre study. Eur. J. CancerA29,698-703 (1993).
- 5. Neoptolemos JP, Stocken DD, Tudur Smith C et al. Adjuvant 5-fluorouracil and folinic acid vs observation for pancreatic cancer: composite data from the ESPAC-1 and -3(v1) trials. Br. J. Cancer 100,246-250 (2009).
- 6. Oettle H, Post S, Neuhaus P et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 297,267-277 (2007).
- 7. Neuhaus P, Riess H, Post S et al. CONKO-001: final results of the randomized, prospective, multicenter Phase III trial of adjuvant chemotherapy with gemcitabine versus observation in patients with resected pancreatic cancer. J. Clin. Oncol.26(20 Suppl.) (2008).
Large trial with 5-year follow-up showing ongoing benefit for gemcitabine in the adjuvant setting for pancreatic cancer. - 8. Jessup JM, Steele G Jr, Mayer RJ et al. Neoadjuvant therapy for unresectable pancreatic adenocarcinoma. Arch. Surg.128,559-564 (1993).
- 9. Evans DB, Rich TA, Byrd DR et al. Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas. Arch. Surg.127,1335-1339 (1992).
- 10. Kalser MH, Ellenberg SS. Pancreatic cancer. Adjuvant combined radiation and chemotherapy following curative resection. Arch. Surg.120,899-903 (1985).
- 11. Regine WF, Winter KA, Abrams RA et al. Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: a randomized controlled trial. JAMA 299,1019-1026 (2008).
- 12. Cunningham D, Chau I, Stocken C et al. Phase III randomised comparison of gemcitabine (GEM) versus gemcitabine plus capecitabine (GEM-CAP) in patients with advanced ponacreatic cancer. Eur. J. Cancer 18(Suppl. 7),APS11 (2005).
- 13. Burris HA 3rd, Moore MJ, Andersen J et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J. Clin. Oncol.15,2403-2413 (1997).
Registration trial of gemcitabine that showed benefit over 5FU. - 14. Mallinson CN, Rake MO, Cocking JB et al. Chemotherapy in pancreatic cancer: results of a controlled, prospective, randomised, multicentre trial. BMJ 281,1589-1591 (1980).
- 15. Palmer KR, Kerr M, Knowles G et al. Chemotherapy prolongs survival in inoperable pancreatic carcinoma. Br. J. Surg. 81,882-885 (1994).
- 16. Glimelius B, Hoffman K, Sjoden PO et al. Chemotherapy improves survival and quality of life in advanced pancreatic and biliary cancer. Ann. Oncol. 7,593-600 (1996).
- 17. Van Rijswijk RE, Jeziorski K, Wagener DJ et al. Weekly high-dose 5-fluorouracil and folinic acid in metastatic pancreatic carcinoma: a phase II study of the EORTC GastroIntestinal Tract Cancer Cooperative Group. Eur. J. Cancer 40,2077-2081 (2004).
- 18. Yip D, Karapetis C, Strickland A et al. Chemotherapy and radiotherapy for inoperable advanced pancreatic cancer. Cochrane Database Syst. Rev.3,CD002093 (2006).
Cochrane review of the role of chemotherapy in metastatic pancreatic cancer. - 19. Sultana A, Smith CT, Cunningham D et al. Meta-analyses of chemotherapy for locally advanced and metastatic pancreatic cancer. J. Clin. Oncol.25,2607-2615 (2007).
Alternate meta-analysis on the role of chemotherapy in metastatic pancreatic cancer. - 20. Rothenberg ML, Moore MJ, Cripps MC et al. A Phase II trial of gemcitabine in patients with 5-FU-refractory pancreas cancer. Ann. Oncol. 7,347-353 (1996).
- 21. Grunewald R, Kantarjian H, Keating MJ et al. Pharmacologically directed design of the dose rate and schedule of 2´,2´-difluorodeoxycytidine (gemcitabine) administration in leukemia. Cancer Res. 50,6823-6826 (1990).
- 22. Tempero M, Plunkett W, Ruiz Van Haperen V et al. Randomized Phase II comparison of dose-intense gemcitabine: thirty-minute infusion and fixed dose rate infusion in patients with pancreatic adenocarcinoma. J. Clin. Oncol. 21,3402-3408 (2003).
- 23. Poplin E, Levy DE, Berlin J et al. Phase III trial of gemcitabine (30-minute infusion) versus gemcitabine (fixed-dose-rate infusion[FDR]) versus gemcitabine + oxaliplatin(GEMOX) in patients with advanced pancreatic cancer (E6201). J. Clin. Oncol. 24,LBA4004 (2006).
- 24. Saif MW. Translational research in pancreatic cancer. Highlights from the 44th ASCO Annual Meeting. Chicago, IL, USA, 30 May-3 June (2008). JOP 9,398-402 (2008).
- 25. Javle MM, Okazaki T, Evans DB et al. Polymorphisms of genes involved in gemcitabine metabolism correlate with prognosis in patients receiving neoadjuvant therapy for pancreatic cancer. J. Clin. Oncol. 26(Suppl.),A4501 (2008).
- 26. Garcia-Manteiga J, Molina-Arcas M, Casado FJ et al. Nucleoside transporter profiles in human pancreatic cancer cells: role of hCNT1 in 2´,2´-difluorodeoxycytidine-induced cytotoxicity. Clin. Cancer Res. 9,5000-5008 (2003).
- 27. Spratlin J, Sangha R, Glubrecht D et al. The absence of human equilibrative nucleoside transporter 1 is associated with reduced survival in patients with gemcitabine-treated pancreas adenocarcinoma. Clin. Cancer Res. 10,6956-6961 (2004).
- 28. Kroep JR, Loves WJ, van der Wilt CL et al. Pretreatment deoxycytidine kinase levels predict in vivo gemcitabine sensitivity. Mol. Cancer Ther. 1,371-376 (2002).
- 29. Giovannetti E, Mey V, Nannizzi S et al. Pharmacogenetics of anticancer drug sensitivity in pancreatic cancer. Mol. Cancer Ther. 5,1387-1395 (2006).
- 30. Ogawa K, Utsunomiya T, Mimori K et al. Differential gene expression profiles of radioresistant pancreatic cancer cell lines established by fractionated irradiation. Int. J. Oncol. 28,705-713 (2006).
- 31. Garcea G, Neal C, Pattenden C et al. Molecular prognostic markers in pancreatic cancer: a systematic review. Eur. J. Cancer 41,2213-2236 (2005).
- 32. Li D, Frazier M, Evans DB et al. Single nucleotide polymorphisms of RecQ1, RAD54L, and ATM genes are associated with reduced survival of pancreatic cancer. J. Clin. Oncol. 24,1720-1728 (2006).
- 33. Heinemann V, Quietzsch D, Gieseler F et al. Randomized Phase III trial of gemcitabine plus cisplatin compared with gemcitabine alone in advanced pancreatic cancer. J. Clin. Oncol. 24,3946-3952 (2006).
- 34. Louvet C, Labianca R, Hammel P et al. Gemcitabine in combination with oxaliplatin compared with gemcitabine alone in locally advanced or metastatic pancreatic cancer: results of a GERCOR and GISCAD Phase III trial. J. Clin. Oncol. 23,3509-3516 (2005).
- 35. Heinemann V, Labianca R, Hinke A et al. Increased survival using platinum analog combined with gemcitabine as compared to single-agent gemcitabine in advanced pancreatic cancer: pooled analysis of two randomized trials, the GERCOR/GISCAD intergroup study and a German multicenter study. Ann. Oncol. 18,1652-1659 (2007).
Meta-analysis of benefit of addition of platinum to gemcitabine. - 36. Colucci G, Giuliani F, Gebbia V et al. Gemcitabine alone or with cisplatin for the treatment of patients with locally advanced and/or metastatic pancreatic carcinoma: a prospective, randomized Phase III study of the Gruppo Oncologia dell'Italia Meridionale. Cancer 94,902-910 (2002).
- 37. Wang X, Ni Q, Jin M et al. Gemcitabine or gemcitabine plus cisplatin for in 42 patients with locally advanced or metastatic pancreatic cancer. Zhonghua Zhong Liu Za Zhi 24,404-407 (2002).
- 38. Xie de R, Liang HL, Wang Y et al. Meta-analysis of inoperable pancreatic cancer: gemcitabine combined with cisplatin versus gemcitabine alone. Chin. J. Dig. Dis. 7,49-54 (2006).
- 39. Herrmann R, Bodoky G, Ruhstaller T et al. Gemcitabine plus capecitabine compared with gemcitabine alone in advanced pancreatic cancer: a randomized, multicenter, Phase III trial of the Swiss Group for Clinical Cancer Research and the Central European Cooperative Oncology Group. J. Clin. Oncol. 25,2212-2217 (2007).
- 40. Bernhard J, Dietrich D, Scheithauer W et al. Clinical benefit and quality of life in patients with advanced pancreatic cancer receiving gemcitabine plus capecitabine versus gemcitabine alone: a randomized multicenter Phase III clinical trial - SAKK 44/00-CECOG/PAN.1.3.001. J. Clin. Oncol. 26,3695-3701 (2008).
- 41. Lemoine NR, Lobresco M, Leung H et al. The erbB-3 gene in human pancreatic cancer. J. Pathol. 168,269-273 (1992).
- 42. Dong M, Nio Y, Guo KJ et al. Epidermal growth factor and its receptor as prognostic indicators in Chinese patients with pancreatic cancer. Anticancer Res. 18,4613-4619 (1998).
- 43. Tobita K, Kijima H, Dowaki S et al. Epidermal growth factor receptor expression in human pancreatic cancer: Significance for liver metastasis. Int. J. Mol. Med. 11,305-309 (2003).
- 44. Bos JL. Ras oncogenes in human cancer: a review. Cancer Res. 49,4682-4689 (1989).
- 45. Benvenuti S, Sartore-Bianchi A, Di Nicolantonio F et al. Oncogenic activation of the RAS/RAF signaling pathway impairs the response of metastatic colorectal cancers to anti-epidermal growth factor receptor antibody therapies. Cancer Res. 67,2643-2648 (2007).
- 46. Eberhard DA, Johnson BE, Amler LC et al. Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J. Clin. Oncol. 23,5900-5909 (2005).
- 47. Moore MJ, Goldstein D, Hamm J et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a Phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 25,1960-1966 (2007).
Trial of the addition of erlotinib to gemcitabine that led to registration of erlotinib despite modest results. - 48. Xiong HQ, Rosenberg A, LoBuglio A et al. Cetuximab, a monoclonal antibody targeting the epidermal growth factor receptor, in combination with gemcitabine for advanced pancreatic cancer: a multicenter Phase II trial. J. Clin. Oncol. 22,2610-2616 (2004).
- 49. Philip P, Benedetti J, Fenoglio-Preiser C et al. Phase III study of gemcitabine [G] plus cetuximab [C] versus gemcitabine in patients [pts] with locally advanced or metastatic pancreatic adenocarcinoma [PC]: SWOG S0205 study. J. Clin. Oncol. 25(Suppl.),LBA4509 (2007).
- 50. Itakura J, Ishiwata T, Shen B et al. Concomitant over-expression of vascular endothelial growth factor and its receptors in pancreatic cancer. Int. J. Cancer 85,27-34 (2000).
- 51. Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science307,58-62 (2005).
- 52. Kindler HL, Friberg G, Singh DA et al. Phase II trial of bevacizumab plus gemcitabine in patients with advanced pancreatic cancer. J. Clin. Oncol. 23,8033-8040 (2005).
- 53. Kindler H, Niedzwiecki D, Hollis D et al. A double-blind, placebo-controlled, randomized Phase III trial of gemcitabine (G) plus bevacizumab (B) versus gemcitabine plus placebo (P) in patients (pts) with advanced pancreatic cancer (PC): a preliminary analysis of Cancer and Leukemia Group B (CALGB). J. Clin. Oncol. 25(Suppl.),A4508 (2007).
- 54. Vervenne W, Bennouna J, Humblet Y et al. A randomized, double-blind, placebo (P) controlled, multicenter Phase III trial to evaluate the efficacy and safety of adding bevacizumab (B) to erlotinib (E) and gemcitabine (G) in patients (pts) with metastatic pancreatic cancer. J. Clin. Oncol. 26(Suppl.) A4507 (2008).
- 55. Spano JP, Chodkiewicz C, Maurel J et al. Efficacy of gemcitabine plus axitinib compared with gemcitabine alone in patients with advanced pancreatic cancer: an open-label randomised phase II study. Lancet 371,2101-2108 (2008).
- 56. Kuo T, Cabebe EC, Koong A et al. An update of a Phase I/II study of the VEGF receptor tyrosine kinase inhibitor vatalanib and gemcitabine in patients with advanced pancreatic cancer. J. Clin. Oncol. 26(Suppl.) A15571 (2008).
- 57. Wallace JA, Locker G, Nattam S et al. Sorafenib (S) plus gemcitabine (G) for advanced pancreatic cancer (PC): a Phase II trial of the University of Chicago Phase II Consortium J. Clin. Oncol.25(Suppl.),A4608 (2007).
Website
101. Study of gemcitabine plus AG-013736 versus gemcitabine for advanced pancreatic cancer http://clinicaltrials.gov/ct2/show/NCT00471146
Authors and Disclosures
Andrew Weickhardt and Michael Michael, Peter MacCallum Cancer Centre, Melbourne, Australia
Financial & Competing Interests Disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Correspondence: Michael Michael, Peter MacCallum Cancer Centre, Melbourne, Australia. michael.michael@petermac.org
Expert Rev Clin Pharmacol. 2009;2(2):173-180. © 2009 Expert Reviews Ltd.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 