急性外耳炎,又名游泳耳,指的在耳膜以外到耳殼之間發炎。 門診常看到病人抱怨,耳朵痛、外耳道腫脹或造成聽力障礙,甚至嘴巴一張開就會疼痛的情形。
好發於濕熱的夏季,因為游泳後(或挖耳不當),如產生下列症狀時,如:耳朵發癢、被異物塞住的感覺、轉動頭部或拉耳朵時耳朵感到疼痛或聲音聽不清楚時,便可能得到外耳炎。
Question
Why is swimmer's ear so common in the summer months, and how should it be managed in primary care?
Response from Judith S. Lynch, MS, MA, APRN-BC
Assistant Clinical Professor, Yale School of Nursing, Milford, Connecticut; Advanced Practice Nurse Practitioner, Naugatuck Valley ENT Associates, Waterbury, Connecticut
Swimmer's Ear -- Acute Otitis Externa
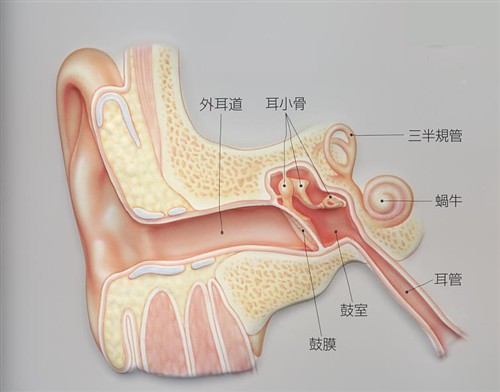
Swimmer's ear, or acute otitis externa (AOE), is an inflammation or infection of the external auditory canal that may or may not include the auricle.[1] It is a common health problem that is seen more frequently in hot weather, particularly in emergency departments during summer vacations.
AOE affects swimmers (hence the name) because their ears are frequently exposed to water. This creates a warm and moist environment, allowing microorganisms to thrive. Individuals with allergic conditions (eczema, allergic rhinitis, asthma) also have a significantly higher risk for this condition developing.[1]
Other risk factors include:
- Absence of cerumen with development of dry skin in the ear canal;
- High humidity and increased temperature;
- Local trauma, especially from the use of cotton-tipped swabs;
- Wearing hearing aids and headphones;
- Presence of exostosis (bony prominences in the canal from exposure to cold water -- often found in surfers);
- Narrow, curved, or tortuous auditory canals, allowing retained moisture; and
- Ear piercings.
Incidence and Prevalence of AOE
A study published in the May 20, 2011, Morbidity and Mortality Weekly Report[2] stated that AOE adds substantially to healthcare costs and to the number of annual provider visits. Findings included:
- One in 123 Americans consulted a provider for swimmer's ear in 2007;
- From 2003-2007, children ages 5-14 years had the highest annual visits for swimmer's ear;
- More than 50% of these visits were by adults 20 years and older;
- Cases peak during summer months;
- 2.4 million heathcare visits for swimmer's ear per year cost half a billion dollars, not including time lost from work and school activities; and
- AOE has no gender or racial predilection.[3]
Classification of AOE
- Acute diffuse OE: the most common form, often seen in swimmers;
- Acute localized OE (furunculosis): associated with an infected hair follicle;
- Chronic OE: an acute infection lasting longer than 6 weeks;
- Eczematous OE: arises from atopic dermatitis, psoriasis, and other dermatologic conditions; and
- Necrotizing "malignant" OE: extends into deeper tissue adjacent to the auditory canal; occurs in immunocompromised adult patients (those with diabetes, AIDS); may result in cellulitis or osteomyelitis.
Pathophysiology of AOE
The presence of cerumen is a healthy defense for the external auditory canal. It is generally acidic (pH 4-5). Cerumen inhibits bacterial or fungal growth and its waxy nature also protects the underlying epithelium from maceration or skin breakdown.
Many individuals have a preoccupation with cerumen, often using various instruments to remove it (flushing syringes, pencils, paper clips, cotton-tipped swabs, etc). This leads to irritation and drying of the canal and skin breakdown and allows an entry point for bacteria or fungi.
AOE develops in swimmers because of excessive water exposure. This reduces cerumen, leading to canal dryness and pruritis. If individuals then insert objects as described above, it results in inflammation and infection.
The most common organisms involved in AOE are:
- Pseudomonas aeruginosa (50%)
- Staphylococcus aureus (23%)
- Anaerobes and gram-negative organisms (12.5%)
- Fungi: Otomycosis is an infection caused by Aspergillus species (80%-90% of the time). Otomycosis is easily identified by long white filaments of hyphae growing from the canal surface. These filaments are often surrounded by black strands.[3]
Signs and Symptoms of AOE
AOE is an extremely painful condition. It typically has a rapid onset with the following symptoms:
- Pruritis and/or otalgia;
- Fullness with/without hearing loss;
- Otorrhea (clear and odorless);
- Tenderness of pinna and/or tragus, especially when pressure is applied to the area;
- Diffuse canal edema/erythema; and
- Regional lymphadenopathy.
If untreated, pruritis, otalgia, and erythema become more pronounced. Often, mucopurulent drainage with decreased or muffled hearing is present. Symptoms can progress to severe pain radiating into the face, neck, or mastoid area. Complete ear blockage from edema, erythema of the auricle, fever, and mastoid tenderness are possible. This may progress to necrotizing OE requiring hospitalization.[4]
Physical Examination of AOE
Testing for preauricular and mastoid tenderness should be done, and a complete otologic examination is essential. However, it is important to gently use the otoscope in the presence of edema and erythema because this will cause excessive pain. Although it is necessary to visualize the tympanic membrane, it is easier to treat the patient's pain first and recheck the area in 48-72 hours to rule out otitis media. Check for lymphadenopathy. Nodes on the affected side will often be enlarged and tender.
Treatment of AOE
The goal of treatment is to relieve the patient's pain while treating the underlying infection as quickly as possible. The use of oral antibiotics is no longer necessary in the treatment of AOE unless the patient is immunocompromised or has an overt otitis media. Topical treatments are effective in 87% to 97% of cases and include:
- Dexamethasone 0.1%/ciprofloxacin 0.3% is a combination of steroid and fluoroquinolone inhibits bacterial DNA syntheses and consequently growth. It also reduces canal edema and relieves pain. The dose is 4-5 drops into the affected ear, twice daily, for 7 days. A longer course may be used with severe cases. Fungal infections may occur with prolonged use.
- Ciprofloxacin otic is the same combination as above without the addition of a steroid. This may be used with mild cases of AOE where edema is not profound. Both compounds may be used safely in patients with perforated tympanic membranes and carry no warnings for ototoxicity. Dose and duration of use are the same as above.[5]
- Neomycin, polymixin B, hydrocortisone has a broad-spectrum bactericidal effect, may be painful to the ear canal, and rarely results in a Neosporin® hypersensitivity. It must not be used if there is a suspicion of a perforated tympanic membrane.
- Fungal infections may be treated with acetic acid solutions or with a topical antifungal agent (1% clotrimazole 3-5 drops twice daily). The course of therapy is usually 10-14 days.
Supportive measures in the management of AOE include the following:
- No swimming! Swimming is not allowed until the infection is completely cleared, usually 10 days to 2 weeks.
- Analgesics: The short-term use of narcotic pain-relief agents is justified. Prescribe pain relief for 48-72 hours for moderate to severe cases. At the 72-hour recheck visit, switch to an anti-inflammatory agent or acetaminophen.
- Water protection: The affected ear must be kept dry during showers, shampoos, etc. This can be accomplished by gently placing a small cotton ball in the ear and applying petroleum jelly to the cotton ball.
- Warm compresses to the area for 10-15 minutes 3 times daily will alleviate discomfort.
- A soft diet is helpful to minimize pain with jaw movement.
- Do not use hearing aids, earplugs, or headphones until the infection clears.
Complications Requiring Consultation or Referral
- Temporary hearing loss: If this does not resolve, refer the patient for audiometric evaluation.
- Chronic OE lasting longer than 6 weeks.
- Cellulitis requiring an oral antibiotic (usually a fluoroquinolone).
- Necrotizing OE with bone and cartilage damage requiring referral and hospitalization
- Sepsis into the brain or nerves: This is rare but life-threatening.
Follow-up
For moderate to severe cases, recheck the patient in 48-72 hours, especially if the tympanic membrane was not visualized during the initial visit. If the patient is not experiencing immediate relief, consultation with an ear-nose-throat specialist is helpful. A wick can be placed in the ear to help deliver topical medication more effectively.
Additional follow-up a week later is advisable for visualizing the affected ear and continued symptom relief. Debris may be gently removed only if the canal has no erythema or edema. Hearing should be restored as edema resolves.
Prevention of AOE
AOE: More Than a Nuisance
AOE is often described as a "nuisance" but only by those who have never experienced its pain. Rapid diagnosis and treatment are necessary to prevent escalating infection and to treat severe discomfort. Prevention measures are essential to keep this common health problem from becoming a greater burden to the healthcare system.
References
- Holten KB, Gick J. Management of the patient with otitis externa. J Fam Pract. 2001;50:353-360. Abstract
- Doheny K. Swimmer's ear costs US half a billion yearly. WebMD Health. May 19, 2011. Available at: http://www.medscape.com/viewarticle/743492 Accessed June 18, 2011.
- Garry JP. Otitis externa. Medscape: Drugs, Diseases, and Procedures. 2010. Available at: http://emedicine.medscape.com/article/84923-overview Accessed June 18, 2011.
- Mayo Clinic. Swimmer's ear. Mayo Clinic Reprints. 2011. Available at: http://www.mayoclinic.com/health/swimmersear/DS00473/DSECTION=symptoms Accessed June 18, 2011.
- Lee S. Otitis externa in emergency medicine medication: otic antibiotics. Medscape: Drugs, Diseases, and Procedures. 2010. Available at: http://emedicine.medscape.com/article/763918-medication#4 Accessed June 24, 2011.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 