Knowledge, Attitudes and Education of Pharmacists Regarding Pharmacogenetic Testing
Abstract and Introduction
Abstract
Aim: Pharmacists are positioned to provide medication counseling and drug information to patients. This study assessed the knowledge, attitudes and education of over 700 pharmacists concerning pharmacogenetics and pharmacogenetic testing.
Methods: A multiquestion, online survey was developed to assess healthcare provider knowledge, attitudes and education concerning pharmacogenetic testing.
Results: More than 90% of pharmacists were interested in learning more about pharmacogenetics and testing, with those with less than 10 years of experience were more likely to want web-based continuing education programs. The pharmacists were unlikely to have had formalized education regarding pharmacogenetics, were very likely to rate their knowledge accurately, and were more likely to have a positive attitude about pharmacogenetics if they had received education regarding pharmacogenetics.
Conclusion: Most pharmacists were interested in learning more about pharmacogenetic testing.
Introduction
Pharmacists know that one dose does not always fit all. Just as pharmacokinetics helps to find the right dose of gentamicin or vancomycin for a patient, pharmacogenetics is the study of how heritable traits affect an individual's response to a medication. Pharmacogenetic testing utilizes the results of genetic tests to guide a patient's drug therapy, much like renal function and drug levels guide pharmacokinetic dosing of selected drugs.
With adverse drug reactions costing hundreds of thousands of US dollars and drugs causing the desired effect in only a subset of those prescribed the drug, any and all scientific advances that decrease the toxicity or improve the efficacy of prescribed medications is beneficial.[1–3] Pharmacists, as the chemists of the healthcare team and the drug therapy experts, are poised to take the lead in providing patients and prescribers with the information essential to optimizing pharmacotherapy for treatment and control of diseases and conditions. Pharmacogenetics can be a powerful tool to aid in refining a drug dose or prioritizing one drug over another for a patient. In fact the US FDA requires inclusion of pharmacogenetic information in over 100 drug labels, approximately 10% of all drug labels up to 2005.[4] Of the drugs reviewed by a major pharmacy benefits manager (PBM; n = 36.1 million patients), approximately 25% of the patients filled prescriptions for drugs with a mention of pharmacogenetics in the drug label.[4] Astoundingly, pharmacists may see one in four patients fill prescriptions for drugs that have human genomic information in the drug label.
Warfarin is one drug with pharmacogenetic information included in the drug label. Warfarin is metabolized by the polymorphic CYP2C9 enzyme, among other drug-metabolizing enzymes, and targets VKORC1 for drug action. The warfarin drug label states that CYP2C9 and VKORC1 genotype can assist in selecting a starting dose of warfarin and provides a table with a range of doses for each combination of genotype information.[101] The dosing recommendations based on genotype were added to the drug label for warfarin after studies found that genetic differences in CYP2C9 and VKORC1 affect the dose of warfarin required to achieve the desired therapeutic effect, generally an international normalized ratio of 2–3, or to avoid untoward effects such as bleeding.[5,6]Ultimately an algorithm that integrates clinical dosing criteria and pharmacogenetics data was established and tested.[7] The pharmacogenetically enhanced algorithm performed better than the clinical algorithm in selecting the therapeutic dose.[7]
Few studies exist that evaluate the knowledge of pharmacists related to pharmacogenetics. In one study by Kadafour et al., healthcare professionals providing anticoagulation services were surveyed regarding warfarin pharmacogenetic testing. The majority of respondents were pharmacists (63.9%) providing anticoagulation services for more than 5 years (62.2%). However, over 80% (80.1%) did not have pharmacogenetic testing available at their practice site. From the five questions assessing knowledge of pharmacogenetic testing associated with warfarin anticoagulation, on average respondents scored 2 out of 5. Respondents with testing available at their practice site scored significantly higher with a score of 3 out of 5 (p = 0.03 by Wilcoxon-rank sum test).[8]
In terms of attitudes regarding pharmacogenetics among pharmacists and other healthcare professionals, our current understanding is very limited. This is unfortunate given that there are likely to be ethical, legal and social implications of the routine use of pharmacogenetics. These include concerns regarding privacy, confidentiality, informed consent, cost, equity of access to treatments that may be more expensive, genetic testing in minors, duty to warn of potential risk for adverse drug reactions, and inappropriate marketing of race-based medications.[9,10] Moreover, the implementation of pharmacogenetics in clinical practice is highly dependent upon acceptance of pharmacogenetics among pharmacists and other healthcare professionals.
One of the few existing studies concerning attitudes about pharmacogenetics is a study by Rogausch and colleagues.[11] Findings from this study suggest that attitudes and concerns regarding pharmacogenetics often differ between patients and physicians. They found that while patients were primarily concerned with privacy issues and adverse treatment by employers or insurance companies, physicians were concerned that employers or insurance companies might pressure patients into pharmacogenetic testing and patients might be disadvantaged if test results indicated a need for higher doses of a drug. In the study by Kadafour and colleagues, over 35% of the participants agreed that warfarin pharmacogenetic testing will help to more accurately determine initial warfarin dose, 32% agreed that warfarin pharmacogenetic testing will help achieve therapeutic international normalized ratio more quickly and 26% agreed that warfarin pharmacogenetic testing will decrease the incidence of bleeding adverse events.[8] An increasing number of drugs have a response that is linked to genetic differences in drug metabolizing enzymes, drug transporters or drug targets. Pharmacists are positioned in communities and in health systems where they may be presented with a patient prescribed a medication that requires at least an understanding of pharmacogenetic principles to address the relationships between genetics and metabolizing enzymes, transporters or drug targets.
Certainly, the call to action by the International Society of Pharmacogenomics that was reported in a paper by Gurwitz et al. in 2005 highlighted the need for pharmacogenomics education for medical, pharmaceutical and other health professionals schools.[12] From the studies on pharmacy education, Latif et al. found that 78% of 41 schools provided pharmacogenomics education, however, only 39% of the doctor of pharmacy programs included this education.[13] By 2010, Murphy et al. found that 92% of schools provided educational content on pharmacogenomics, with 89% providing content within the clinical degree program or doctor of pharmacy program.[14]
The purpose of this article is to share select findings from a larger study concerning knowledge and attitudes regarding pharmacogenetic testing among healthcare professionals. For this article, the focus is limited to the responses of pharmacists from North Carolina, USA.
Methods
With the increase in evidence supporting the use of pharmacogenetics in clinical practice, a panel of experts from the University of North Carolina (UNC; NC, USA) Center for Genomics and Society and the UNC Institute for Pharmacogenomics and Individualized Therapy (IPIT), created a survey that addressed not only knowledge of pharmacogenetics, but also attitudes regarding pharmacogenetic testing. The survey was evaluated by an interdisciplinary group of nurses, physicians and pharmacists with expertise in pharmacogenetic testing and pilot-tested with five clinicians prior to the beginning of data collection. The survey included: six background information questions, two questions designed to assess overall perceptions of understanding regarding genetics and pharmacogenetics, ten basic knowledge questions (five about genetics and five about pharmacogenetics), eight questions concerning attitudes about pharmacogenetic testing (four about pharmacogenetic testing in general and four focusing on pharmacogenetic testing to guide warfarin therapy), four questions for clinicians with prescriptive privileges, and two questions developed to assess interest in future educational offerings regarding pharmacogenetic testing.
The Institutional Review Board at the UNC at Chapel Hill determined that the Institutional Review Board approval was not required because responses to the survey were anonymous. An email invitation to participate with a link to an online survey through the survey engine, Survey Monkey, was distributed to 9516 pharmacists licensed in the state of North Carolina, USA, via the NC Board of Pharmacy distribution list in February of 2009.[102]
Statistical Analysis
Descriptive statistics were generated for all respondents as a group, including frequencies for categorical variables and means for continuous variables. Knowledge scores (i.e., total correct out of the five genetics questions, out of the five pharmacogenetics questions, and out of all ten questions) were compared across selected categorical respondent characteristics using one-way analysis of variance tests. When associated F tests were significant, post hoc analyses were conducted using Duncan's multiple range test to identify respondent groups with different mean knowledge. All statistical analyses were performed using SAS software system version 9.2. In all circumstances p-values of less than 0.05 were used to define significance.
Results
Seven hundred and thirty seven pharmacists began the survey yielding an overall response rate of 7.7%, with 728 completing the majority of the questions. In addition to being a pharmacist, one respondent was also a physician, another was a medical student and two were registered nurses.
Education
More than half of respondents achieved a doctor of pharmacy degree (51.8%), while 40.6% obtained a Bachelor of Science degree in pharmacy and 1.7% held an additional doctorate. Approximately 10% of the respondents were faculty members or educators. The respondents well represented pharmacists with varying years of experience: 19.3% out of 727 respondents practicing less than 5 years and 22.4% practicing more than 30 years (Figure 1). A total of 47.0% of the pharmacists did not have any genetics education. However, 26.1% of respondents took an undergraduate genetics course and 14.2% declared receiving genetics education via a continuing education course (Table 1).
Table 1. Types of prior genetics education† (n = 728).
| Type of genetics education | Respondents (%) |
|---|---|
| No genetics education | 47.0 |
| Undergraduate genetics course | 26.1 |
| Continuing education course | 14.2 |
| Seminar or workshop | 8.7 |
| Grand rounds | 6.5 |
| Other | 9.6 |
†More than one response allowed.

Knowledge
The survey contained five questions to assess knowledge of general genetics and five questions to assess the knowledge of general pharmacogenetics (Box 1). In assessing level of education as an influencing factor on knowledge, respondents with a PharmD had a significantly higher mean score on the total ten questions and the five genetics and five pharmacogenetics questions separately compared with respondents without an advanced degree or with a masters (all three p-values <0.001). Self-identified educators and those with prescribing privileges had higher scores on the ten knowledge assessment questions (p-values 0.003 and 0.029, respectively). Educators scored higher overall on the genetics and pharmacogenetics questions separately (p-values 0.022 and 0.002, respectively). However, the respondents with prescribing privileges scored higher on pharmacogenetics questions (p = 0.008) but not on the five genetics questions (p = 0.237).
New graduates with fewer than 5 years since matriculation scored statistically significantly higher on all ten questions and the five genetics and pharmacogenetics questions than the respondents out of school for 5 years or more (all p-values <0.001). Distant graduates out of school for 30 years or more scored significantly lower than all other respondents for all three assessments (all p-values <0.001) (Figure 2).

Figure 2.
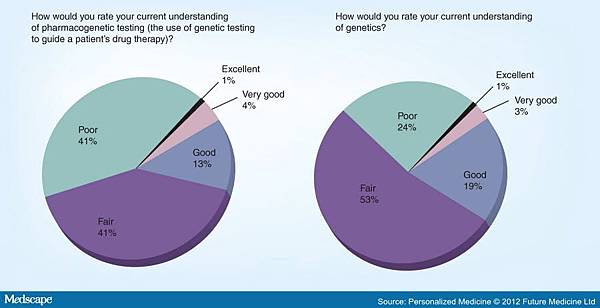
Figure 3.Pharmacist understanding.
Attitudes
Table 2 contains the eight questions related to attitudes regarding pharmacogenetic testing. There were five possible responses for each question ranging from 1: not likely to 5: very likely for questions 1, 3, 5, and 7, 1=not concerned to 5: very concerned for questions 2 and 4 and 1: not comfortable to 5: very comfortable for questions 6 and 8. The response to questions 2 and 4 were reverse coded so that larger values for all eight questions corresponded to more positive attitudes. A total positive attitude score was then computed as the average of the eight attitude questions. Cronbach's α for this attitude scale was acceptable at 0.71. PharmD and BSc in pharmacy degree recipients did not significantly differ in mean total positive attitude score or in mean values for each of the eight attitude questions. Similarly, when comparing pharmacists with prescribing privileges versus those without prescribing privileges, the mean positive attitude score and mean values for the eight questions did not differ significantly. Respondents serving as educators were not significantly different than noneducators in mean total positive attitude score but were significantly more comfortable having genetic information incorporated into the determination of their patient's initial warfarin dose (question 6). Mean total positive attitude increased with self-reported level of knowledge of genetics. For questions 2, 5, 6 and 8, the mean values for the individual questions increased with increased with self-reported knowledge. The mean total positive attitude score also increased with self-reported level of knowledge of pharmacogenetic testing. Similarly, for questions 1 and 5–8, the mean score increased with self-reported knowledge.
Educational Offerings
Ninety percent (90.5%) of respondents are interested in learning more about pharmacogenetic testing (see Figure 4 for the breakdown on types of educational offerings of interest). A total of 88.0% of pharmacists with a PharmD degree and 81.5% of BSc graduates want to receive education on pharmacogenetic testing. As a group, educators want education on pharmacogenetic testing more than noneducators (93.2 vs 84.6%; p = 0.05). Unlike level of education and serving as an educator, pharmacists with and without prescribing privileges do not differ in percentage wanting education on pharmacogenetic testing.
Table 2. Questions on attitudes about phamacogentic testing.
| Question number | Mean value and standard deviation | Question assessing attitude regarding pharmacogenetic testing |
|---|---|---|
| 1 | Mean: 3.5; standard deviation: 1.0 | In your opinion, how likely is it that pharmacogenetic testing will help to decrease the number of adverse drug reactions? |
| 2 | Mean: 3.0; standard deviation: 1.3 | How concerned are you that unauthorized persons may gain access to the results of a patient's pharmacogenetic testing? |
| 3 | Mean: 2.4; standard deviation: 1.2 | In your opinion, how likely is it that pharmacogenetic testing will help to decrease the cost of developing new drugs? |
| 4 | Mean: 2.6; standard deviation: 1.3 | How concerned are you that pharmacogenetic testing may result in discrimination by employers and/or insurance companies? |
| 5 | Mean: 3.5; standard deviation: 1.0 | In your opinion, how likely is it that pharmacogenetic testing will help to decrease the time it takes to find the optimal dose of warfarin for patients? |
| 6 | Mean: 3.7; standard deviation: 1.0 | How comfortable would you be having genetic information incorporated into the determination of your patient's initial warfarin dose? |
| 7 | Mean: 3.5; standard deviation: 1.0 | In your opinion, how likely is it that pharmacogenetic testing will help to decrease the adverse reactions experienced by patients on warfarin? |
| 8 | Mean: 3.9; standard deviation: 1.1 | If you were the patient being started on warfarin, how comfortable would you be having genetic information incorporated into the determination of your initial dose of warfarin? |
Contains the eight questions related to attitudes about pharmacogenetic testing. There were five possible responses for each question ranging from 1: not likely to 5: very likely for questions 1, 3, 5 and 7; 1: not concerned to 5: very concerned for questions 2 and 4; and 1: not comfortable to 5: very comfortable for questions 6 and 8. The response to questions 2 and 4 were reverse coded so that larger values for all eight questions corresponded to more positive attitudes. A total positive attitude score was then computed as the average of the eight attitude questions. Cronbach's a for this attitude scale was acceptable at 0.71. Within the table individual mean scores for each question are reported, along with standard deviation.

Figure 4.
AHEC: Area health education center; CE: Continuing education; CME: Continuing medical education.
When evaluating the interest in pharmacogenetic testing by years of practice, the 5–10 years since graduation group had the highest overall percentage of respondents interested at 92.9% versus the group with the fewest interested in education, the more than 30 years since graduation group, with 77.3% (p = 0.008). The pharmacists that identified having taken a continuing education genetics course in the past were more likely to want an educational session on pharmacogenetic testing (94.2 vs 83.4%; p = 0.005) as were those who had taken an undergraduate course in the past (92.1 vs 82,3%; p = 0.001). Pharmacists who had not had any prior genetics education were significantly less likely to want an educational session on pharmacogenetic testing (80.6 vs 89.8%).
When reviewing the types of pharmacogenetics education that respondents want, the PharmDs prefer web-based continuing medical education more than BSc graduates (58.3 vs 42.5%; p < 0.001). The preference for web-based continuing medical education also significantly decreased with increased years in practice (61.4% for 0–4 years, 64.3% for 5–10 years, 51.6% with 10–19 years, 46.4% for 20–29 years and 38.7% for 30 or more years; p < 0.001).
Discussion
Pharmacists have long been thought of as the medication experts in the healthcare field. It has become evident over the past decade that pharmacogenetics is evolving into an essential tool to ensure optimal medication use in a growing number of medications and disease states. Therefore, it is imperative that pharmacists are prepared to use pharmacogenetic information to appropriately individualize medication therapy for patients now and in the future. The pharmacist serves many roles in the implementation of pharmacogenetics in the healthcare setting.[15] These include serving as a clinician who ensures that all proper information is incorporated into medication decisions, including pharmacogenetics. Pharmacists also serve as educators for patients and healthcare professionals alike to raise awareness of pharmacogenetics principles and clinical utilization strategies. Finally, pharmacists are in the optimal role to investigate and advance the science of pharmacogenetics through pilot and comparative–effectiveness research.
A survey on attitudes towards pharmacogenetics was recently reported for the US public.[16] This survey was conducted by telephone to over 2000 randomly identified participants throughout the US. The study achieved a 42% response rate and demonstrated a high rate of interest in pharmacogenetic testing, which could predict side effects, guide dosing, or assist with medication selection. Most were not willing to undergo testing, though, if there was a risk that their information could be shared without their permission. To date, there has been no formal analysis of practicing pharmacists' knowledge and attitudes of pharmacogenetics information. Our report is the first such survey that examines not only the pharmacists' perceived knowledge but attempts to measure actual knowledge through several questions related to pertinent genetic and pharmacogenetic information. We also explored attitudes towards pharmacogenetic information being used in clinical practice as well as thoughts on how pharmacists could best obtain further pharmacogenetics education.
Not surprisingly, over half of practicing pharmacists have received some formal training in genetics. Approximately a half of those who did respond as having formal genetics education, had genetics as part of their undergraduate curriculum, which presumably did not contain any content on pharmacogenetics. It was not until 2007, that the American Council on Pharmacy Accreditation set pharmacogenetics as a required component of the pharmacy curriculum.[103] The majority of participants in this survey have been in practice for over 10 years so the likelihood of receiving pharmacogenetics as part of the pharmacy curriculum is unlikely. Providing continuing education opportunities in pharmacogenetics has been a major focus of many colleges of pharmacy as well as many national pharmacy organizations. Only 14% of respondents had received any pharmacogenetics training through continuing education programs.
With a lack in formalized education in pharmacogenetics, it is not surprising that the majority of respondents reported their understanding of pharmacogenetics as fair or poor (83%). Only 17% of respondents rated their understanding of pharmacogenetics as excellent, very good or good. Those participants who rated their knowledge as either excellent or very good were associated with the highest mean scores on knowledge assessment, which helps validate this perception as being accurate. One encouraging statistic was that those with less than 10 years of practice experience demonstrated the highest scores on pharmacogenetic knowledge assessment, which may represent the increased focus of pharmacogenetics in the pharmacy curricula across the nation, as well as the increased amount of information on pharmacogenetics over the past decade. Of note, this group of practitioners with less than 10 years of experience also had the highest level of interest in further pharmacogenetics education.
In a similar survey of pharmacists that practice at three sites for the Mayo Clinic (in Arizona [AZ, USA], Florida [FL, USA] and Minnesota [MN, USA]), the authors conclude that pharmacists are interested to know about pharmacogenetics, feel pharmacogenetics contributes to the practice of pharmacy, but they feel ill-prepared to act on the results of pharmacogenetic tests. The survey responses suggest that practicing pharmacists need additional educational offerings to teach them about the application of pharmacogenetics.[17]
There are several limitations of our survey that may have impacted the type and validity of the results. First, the sample size is relatively small compared with the number of pharmacists practicing in the state of NC and throughout the USA. This is evidenced and compounded by our low response rate of 7.7%. With nearly 10,000 pharmacists with an active NC license, our survey population may not be reflective of the average pharmacist licensed in NC nor the USA.
Future Perspective
With new graduates matriculating from schools of pharmacy in the USA, the pharmacogenetics knowledge is changing. The accrediting body for schools of pharmacy, the American Council on Pharmaceutical Education, encourages systematic integration of pharmacogenetics into the education of doctor of pharmacy students alongside other specific drug information.[103] From 2005 to 2010, the schools of pharmacy surveyed improved in the education of pharmacogenetics provided to doctor of pharmacy students (from 39% in 2005 to 89% in 2010).[13,14] The level of didactic, and hopefully experiential education that incorporates principles of pharmacogenetics is likely to grow exponentially. There is a need for all pharmacists to feel comfortable interpreting medication related information that considers pharmacogenetic testing and be adept at relaying that information at the point of patient care.
References
- Phillips KA, Veenstra DL, Oren E, Lee JK, Sadee W. Potential role of pharmacogenomics in reducing adverse drug reactions: a systematic review. JAMA 286(18), 2270–2279 (2001).
- Wysowski DK, Nourjah P, Swartz L. Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch. Intern. Med. 167(13), 1414–1419 (2007).
- Wysowski DK, Swartz L. Adverse drug event surveillance and drug withdrawals in the United States, 1969–2002: the importance of reporting suspected reactions. Arch. Intern. Med. 165(12), 1363–1369 (2005).
- Frueh FW, Amur S, Mummaneni P et al. Pharmacogenomic biomarker information in drug labels approved by the United States food and drug administration: prevalence of related drug use. Pharmacotherapy 28(8), 992–998 (2008).
•• First paper to highlight the relevance of pharmacogenetics information as it relates to commonly prescribed medications. - Lindh JD, Lundgren S, Holm L, Alfredsson L, Rane A. Several-fold increase in risk of overanticoagulation byCYP2C9 mutations. Clin. Pharmacol. Ther. 78(5), 540–550 (2005).
- Sanderson S, Emery J, Higgins J. CYP2C9 gene variants, drug dose, and bleeding risk in warfarin-treated patients: a HuGEnet systematic review and meta-analysis. Genet. Med. 7(2), 97–104 (2005).
- International Warfarin Pharmacogenetics Consortium, Klein TE, Altman RB et al. Estimation of the warfarin dose with clinical and pharmacogenetic data. N. Engl. J. Med. 360(8), 753–764 (2009).
•• First paper to compare a clinical dosing algorithm with a pharmacogenetically enhanced dosing algorithm for dosing warfarin in a derivation cohort and validation cohort. - Kadafour M, Haugh R, Posin M, Kayser SR, Shin J. Survey on warfarin pharmacogenetic testing among anticoagulation providers. Pharmacogenomics 10(11), 1853–1860 (2009).
- Corrigan OP. Pharmacogenetics, ethical issues: review of the Nuffield Council on Bioethics Report. J. Med. Ethics31(3), 144–148 (2005).
- Marx-Stolting L. Pharmacogenetics and ethical considerations: why care? Pharmacogenomics J. 7(5), 293–296 (2007).
- Rogausch A, Prause D, Schallenberg A, Brockmöller J, Himmel W. Patients' and physicians' perspectives on pharmacogenetic testing. Pharmacogenomics 7(1), 49–59 (2006).
- Gurwitz D, Lunshof JE, Dedoussis G et al. Pharmacogenomics education: International Society of Pharmacogenomics recommendations for medical, pharmaceutical, and health schools deans of education.Pharmacogenomics J. 5(4), 221–225 (2005).
- Latif DA. Pharmacogenetics and pharmacogenomics instruction in schools of pharmacy in the USA: is it adequate? Pharmacogenomics 6(4), 317–319 (2005).
•• Highlights the deficiency in pharmacy education with regard to pharmacogenetics, especially in the doctor of pharmacy program curricula. - Murphy JE, Green JS, Adams LA, Squire RB, Kuo GM, McKay A. Pharmacogenomics in the curricula of colleges and schools of pharmacy in the United States. Am. J. Pharm. Educ. 74(1), 7 (2010).
•• Follow-up survey that highlights the improvements in the doctor of pharmacy curricula since the 2005 survey by Latif et al..[13] - Brock TP, Valgus JM, Smith SR, Summers KM. Pharmacogenomics: implications and considerations for pharmacists. Pharmacogenomics 4(3), 321–330 (2003).
- Haga SB, O'Daniel JM, Tindall GM, Lipkus IR, Agans R. Survey of US public attitudes toward pharmacogenetic testing. Pharmacogenomics J. doi:10.1038/tpj.2011.1 (2011) (Epub ahead of print).
•• First paper to describe patient attitudes towards pharmacogenetic testing in a US population. - McCullough KB, Formea CM, Berg KD et al. Assessment of the pharmacogenomics educational needs of pharmacists. Am. J. Pharm. Educ. 75(3), 51 (2011).
Websites
101. Coumadin tablets. www.accessdata.fda.gov/drugsatfda_docs/label/2010/009218s108lbl.pdf
102. Survey Monkey. www.surveymonkey.com
103. Amercian College of Pharmaceutical Education. www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf
Papers of special note have been highlighted as:
•• of considerable interest






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 