| Rivadeneira DE, Steele SR, Ternent C, Chalasani S, Buie WD, Rafferty JL, Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of hemorrhoids (revised 2010). Dis Colon Rectum 2011 Sep;54(9):1059-64. [56 references] PubMed |
This is the current release of the guideline.
This guideline updates a previous version: Cataldo P, Ellis CN, Gregorcyk S, Hyman N, Buie WD, Church J, Cohen J, Fleshner P, Kilkenny J 3rd, Ko C, Levien D, Nelson R, Newstead G, Orsay C, Perry WB, Rakinic J, Shellito P, Strong S, Ternent C, Tjandra J, Whiteford M. Practice parameters for the management of hemorrhoids (revised). Dis Colon Rectum 2005 Feb;48(2):189-94. [41 references]
Scope
Hemorrhoids
Evaluation
Management
Treatment
Family Practice
Gastroenterology
Internal Medicine
Health Care Providers
Nurses
Patients
Physician Assistants
Physicians
To provide practice parameters on the evaluation and management of hemorrhoids
Patients with hemorrhoids
Evaluation
- Patient and family history
- Physical examination
- Endoscopic evaluation (colonoscopy, proctoscopy, barium enema with flexible sigmoidoscopy)
Treatment
- Dietary management (i.e., adequate fluid and fiber intake)
- Office treatmentTreatment of thrombosed external hemorrhoids (excision)
- Hemorrhoid banding
- Sclerotherapy
- Infrared coagulation
- Surgical hemorrhoidectomy
- Doppler-guided hemorrhoidectomy
- Stapled hemorrhoidopexy (not effective for large external hemorrhoids)
- Excision (open or closed hemorrhoidectomy)
- Recurrence rate
- Relief of symptoms
- Complications of treatments
Methodology
Hand-searches of Published Literature (Secondary Sources)
Searches of Electronic Databases
A literature search of MEDLINE, PubMed, and the Cochrane Database of Collected Reviews was performed through April 2010. Key word combinations included hemorrhoid, internal and external hemorrhoids, hemorrhoid disease, thrombosed hemorrhoid, rubber band ligation, hemorrhoidopexy, hemorrhoidectomy, PPH, Milligan-Morgan, Ferguson, Doppler guided, and stapled hemorrhoidopexy. Directed searches of the embedded references from the primary articles were also performed in selected circumstances.
Not stated
See the "Rating Scheme for the Strength of the Recommendations" field, below.
Systematic Review
Not stated
These guidelines are built on the last set of the American Society of Colon and Rectal Surgeons (ASCRS) Practice Parameters for the management of hemorrhoids published in 2005. The final grade of recommendation and level of evidence was determined using the Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) system (see the "Rating Scheme for the Strength of Recommendations" field).
The Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) System–Grading Recommendationsa
| Description | Benefit versus Risk and Burdens | Methodologic Quality of Supporting Evidence | Implications | |
|---|---|---|---|---|
| 1A | Strong recommendation, high-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | RCTs without important limitations or overwhelming evidence from observational studies | Strong recommendation, can apply to most patients in most circumstances without reservation |
| 1B | Strong recommendation, moderate-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | RCTs with important limitations (inconsistent results, methodologic flaws, indirect, or imprecise) or exceptionally strong evidence from observational studies | Strong recommendation, can apply to most patients in most circumstances without reservation |
| 1C | Strong recommendation, low- or very-low-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | Observational studies or case series | Strong recommendation but may change when higher quality evidence becomes available |
| 2A | Weak recommendation, high-quality evidence | Benefits closely balanced with risks and burdens | RCTs without important limitations or overwhelming evidence from observational studies | Weak recommendation, best action may differ depending on circumstances or patients' or societal values |
| 2B | Weak recommendations, moderate-quality evidence | Benefits closely balanced with risks and burdens | RCTs with important limitations (inconsistent results, methodologic flaws, indirect, or imprecise) or exceptionally strong evidence from observational studies | Weak recommendation, best action may differ depending on circumstances or patients' or societal values |
| 2C | Weak recommendation, low- or very-low-quality evidence | Uncertainty in the estimates of benefits, risks and burden; benefits, risk and burden may be closely balanced | Observational studies or case series | Very weak recommendations; other alternatives may be equally reasonable |
RCT = randomized controlled trial
aAdapted from Guyatt G, Gutermen D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians Task Force. Chest. 2006;129:174 –181.
A formal cost analysis was not performed and published cost analyses were not reviewed.
Not applicable
Recommendations
The levels of evidence and the grades of recommendations (1A-2C) are defined at the end of the "Major Recommendations" field.
Recommendations
- The evaluation of patients with hemorrhoids should include a directed history and physical examination. Grade of Recommendation: Strong recommendation based on low-quality evidence 1C.
The diagnosis of hemorrhoids is almost always a clinical one. The initial assessment should include a thorough targeted history and physical examination, with focus on the extent, severity, and duration of symptoms, such as bleeding, prolapse, issues of hygiene and pain, and fiber and fluid intake, as well. In addition, a careful review of bowel habits including frequency, consistency, and ease of evacuation should be performed. All patients with rectal bleeding require a detailed family history with particular emphasis on intestinal disease. The presence of malignant conditions should be evaluated to assess for sporadic or hereditary colon and rectal cancer, and thus for the need for extended colonic evaluation.
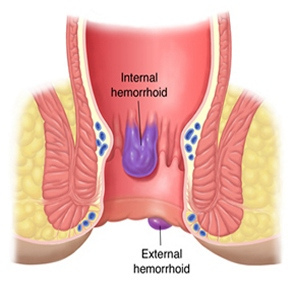
The physical examination should typically include visual inspection of the anus, digital examination, and anoscopy and/or proctoscopy looking for evidence of thrombosis or concomitant anorectal pathology, such as fissure, fistula, abscess, or evidence of Crohn's disease. Internal hemorrhoids, located above the dentate line, can be assigned a grade based on the definitions in the table below, which will help to guide therapy. Laboratory evaluation is not typically required.
Table: Classification of Internal Hemorrhoids
Grade Physical Findings I Prominent hemorrhoidal vessels, no prolapse II Prolapse with Valsalva and spontaneous reduction III Prolapse with Valsalva requires manual reduction IV Chronically prolapsed manual reduction ineffective
- Complete endoscopic evaluation of the colon is indicated in select patients with hemorrhoids and rectal bleeding. Grade of Recommendation: Strong recommendation based on moderate-quality evidence 1B.
Although commonly associated with hemorrhoids, complaints of rectal bleeding may be a symptom of other disease processes, such as colorectal cancer, inflammatory bowel disease, other colitides, diverticular disease, and angiodysplasia. A thorough personal history, a detailed family history, and a physical examination, which may include proctoscopy and/or flexible sigmoidoscopy, will identify high-risk patients requiring more extensive evaluation. Those who fulfill the select criteria should have a full colonic evaluation with colonoscopy. Patients unable to undergo colonoscopic evaluation may be considered for flexible sigmoidoscopy combined with barium enema or other diagnostic modalities per consensus guidelines.
- Dietary modification consisting of adequate fluid and fiber intake is the primary first-line nonoperative therapy for patients with symptomatic hemorrhoid disease. Strong recommendation based on moderate quality evidence 1B.
Constipation and altered bowel habits can play a significant role in many patients with symptomatic hemorrhoids. Whereas more aggressive office-based or operative treatment is usually required for advanced hemorrhoidal disease (grades III to IV or those with significant external components), increased fiber and fluid intake has been shown to improve symptoms of mild to moderate prolapse and bleeding. Patients should also be counseled as to maintaining proper bowel habits, such as the avoidance of straining and limiting prolonged time on the commode, because this has been associated with higher rates of symptomatic hemorrhoids.
- Most patients with grade I, II, and III hemorrhoid disease in whom medical treatment fails may be effectively treated with office-based procedures, such as banding, sclerotherapy, and infrared coagulation. Hemorrhoid banding is typically the most effective option. Grade of Recommendation: Strong recommendation based on moderate-quality evidence 1B.
The goals of all office-based procedures are three-fold: to decrease vascularity, reduce redundant tissue, and increase hemorrhoidal fixation to the rectal wall to minimize prolapse. These procedures are all relatively well tolerated, causing minimal pain and discomfort. However, patients should understand they all have a variable recurrence rate and may require repeated applications.
Rubber Band Ligation. Rubber band ligation is a commonly used and effective way of treating symptomatic internal hemorrhoids. Banding is commonly performed with either a suction apparatus or a forceps ligator. Both methods are acceptable, because, in general, banding is very well tolerated.
A careful and detailed history should be specifically obtained from the patient in regard to the presence of coagulation disorders, either intrinsic, such as those with thrombocytopenia, or acquired, as seen with antiplatelet therapy (Plavix), or anticoagulated with warfarin (Coumadin) or heparin products. In general, the performance of a banding procedure is contraindicated in this group because the exceedingly high incidence of postprocedure bleeding.
Sclerotherapy. Sclerotherapy involves injection of 3 to 5 mL of a sclerosant into the apex of an internal hemorrhoid. This relatively simple procedure may be used for small, bleeding internal hemorrhoids. Unfortunately, longer follow-up intervals often demonstrate a relatively higher rate of symptomatic recurrence. This approach may be particularly appealing in those with bleeding tendencies, such as the patient receiving antiplatelet or anticoagulation therapy.
Infrared Coagulation. Infrared coagulation involves the direct application of infrared waves that results in protein necrosis within the hemorrhoid. This is most commonly used for grade I and II hemorrhoids.
Complications. Patients should be counseled regarding the rare but devastating complications of perianal sepsis and urinary retention and fever with all office-based hemorrhoid procedures.
- Most patients with thrombosed external hemorrhoids benefit from surgical excision within 72 hours of the onset of symptoms. Grade of Recommendation: Strong recommendation based on low-quality evidence 1C.
Most excisions can be safely performed in the office setting, although extensive large thrombosed hemorrhoids and those extending into the anal canal may require a more formal surgical approach in the operating room. One should avoid lancing techniques with simple incision and drainage, because they tend to result in higher rates of reaccumulation and may worsen symptoms with further expansion of the thrombosis.
- Surgical hemorrhoidectomy should be reserved for patients who are refractory to office procedures, who are unable to tolerate office procedures, who have large external hemorrhoids, or who have combined internal and external hemorrhoids with significant prolapse (grades III to IV). Grade of Recommendation: Strong recommendation based on moderate-quality evidence 1B.
Surgical Excision. Surgical excision of hemorrhoids remains a very effective approach. In general, it should be reserved for patients for whom office-based procedures fail or who cannot tolerate these procedures, grade III or IV hemorrhoids, or patients with substantial external skin tags.
Either open or closed hemorrhoidectomy can be performed with a variety of surgical devices including surgical scalpel, scissors, monopolar cauterization, bipolar energy, and ultrasonic devices. In general, there appears to be no definitive advantage of one over the other. As such, individual patient factors and preferences need to be carefully weighed and considered before a decision for operative therapy.
Hemorrhoidopexy. Stapled hemorrhoidopexy uses a circular stapling device that resects internal hemorrhoids and fixes the remaining tissues in place. Although effective for internal prolapsing disease, it may not adequately address external hemorrhoids. In general, the stapled procedure is not effective for large external or thrombosed hemorrhoids, although limited data have demonstrated some success.
Doppler-Guided Hemorrhoidectomy. Doppler-guided/assisted hemorrhoidal ligation is a procedure that uses an anoscope fashioned with a Doppler probe for identification of each hemorrhoid arterial blood supply that is subsequently ligated. A potential benefit is the lack of tissue excised and possibly less pain. Currently, larger studies including variations of the Doppler technique and comparisons with other methods with longer follow-up intervals are required before definitive recommendations on this method.
Definitions:
The Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) System–Grading Recommendationsa
| Description | Benefit versus Risk and Burdens | Methodologic Quality of Supporting Evidence | Implications | |
|---|---|---|---|---|
| 1A | Strong recommendation, high-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | RCTs without important limitations or overwhelming evidence from observational studies | Strong recommendation, can apply to most patients in most circumstances without reservation |
| 1B | Strong recommendation, moderate-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | RCTs with important limitations (inconsistent results, methodologic flaws, indirect, or imprecise) or exceptionally strong evidence from observational studies | Strong recommendation, can apply to most patients in most circumstances without reservation |
| 1C | Strong recommendation, low- or very-low-quality evidence | Benefits clearly outweigh risk and burdens or vice versa | Observational studies or case series | Strong recommendation but may change when higher quality evidence becomes available |
| 2A | Weak recommendation, high-quality evidence | Benefits closely balanced with risks and burdens | RCTs without important limitations or overwhelming evidence from observational studies | Weak recommendation, best action may differ depending on circumstances or patients' or societal values |
| 2B | Weak recommendations, moderate-quality evidence | Benefits closely balanced with risks and burdens | RCTs with important limitations (inconsistent results, methodologic flaws, indirect, or imprecise) or exceptionally strong evidence from observational studies | Weak recommendation, best action may differ depending on circumstances or patients' or societal values |
| 2C | Weak recommendation, low- or very-low-quality evidence | Uncertainty in the estimates of benefits, risks and burden; benefits, risk and burden may be closely balanced | Observational studies or case series | Very weak recommendations; other alternatives may be equally reasonable |
RCT = randomized controlled trial
aAdapted from Guyatt G, Gutermen D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians Task Force. Chest. 2006;129:174 –181.
None provided
Evidence Supporting the Recommendations
The type of supporting evidence is identified and graded for each recommendation (see the "Major Recommendations" field).
Benefits/Harms of Implementing the Guideline Recommendations
Appropriate evaluation and management of patients with hemorrhoids
- The most common complications of rubber band ligation are postband anorectal pain, rectal bleeding, thrombosed external hemorrhoids, and vasovagal symptoms, which have been reported in <1% to 3% of patients.
- Complications of sclerotherapy are uncommon; the most frequent one is minor discomfort or bleeding with injection. Rare, serious complications have resulted from erroneous injection site placement or systemic effects of the solution itself, including the creation of rectourethral fistulas, rectal perforations, and necrotizing fasciitis. These compilations have been described in isolation or in conjunction with the simultaneous application of rubber bands.
- Previous reports on infrared coagulation have demonstrated high rates of recurrence, especially with grades III and IV.
- Overall, the incidence of major complications is rare; yet, one must remember that perianal sepsis has been described as a life-threatening complication with all office-based procedures. The onset of urinary retention and fever immediately after an office-based procedure may be the initial sign of perianal sepsis and mandates emergent patient evaluation. As such, patients should be counseled regarding these rare but devastating complications.
- Hemorrhoidectomy is associated with increased pain and the highest complication rate.
- A Cochrane review of 6 randomized trials with 628 patients all having follow-up greater than one year demonstrated no significant differences between stapled hemorrhoidopexy and conventional hemorrhoidectomy in terms of pain, pruritus, and urgency, with higher long-term recurrences following the stapled technique. Although stapled hemorrhoidopexy is associated with several unique complications (i.e., rectovaginal fistula, staple line bleeding), overall complication rates are similar to conventional excisional hemorrhoidectomy.
- A recent systematic review of Doppler-guided hemorrhoidectomy including 17 series with 1996 patients reported an overall recurrence rate of 9% for prolapse, 8% for bleeding, and 5% for pain at defecation. For those with a minimum of 1-year follow-up, the recurrence rate was 11% for prolapse, 10% for bleeding, and 9% for pain at defecation. The authors found recurrences were higher for grade IV hemorrhoids and recommended this for use in grade II and III disease.
Contraindications
A careful and detailed history should be specifically obtained from the patient in regard to the presence of coagulation disorders, either intrinsic, such as those with thrombocytopenia, or acquired, as seen with antiplatelet therapy (Plavix), or anticoagulated with warfarin (Coumadin) or heparin products. In general, the performance of a banding procedure is contraindicated in this group because the exceedingly high incidence of postprocedure bleeding.
Qualifying Statements
- These guidelines are inclusive, and not prescriptive. Their purpose is to provide information on which decisions can be made, rather than dictate a specific form of treatment.
- It should be recognized that these guidelines should not be deemed inclusive of all proper methods of care or exclusive of methods of care reasonably directed to obtaining the same results. The ultimate judgment regarding the propriety of any specific procedure must be made by the physician in light of all of the circumstances presented by the individual patient.
Implementation of the Guideline
An implementation strategy was not provided.
Institute of Medicine (IOM) National Healthcare Quality Report Categories
Patient-centeredness
Identifying Information and Availability
| Rivadeneira DE, Steele SR, Ternent C, Chalasani S, Buie WD, Rafferty JL, Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of hemorrhoids (revised 2010). Dis Colon Rectum 2011 Sep;54(9):1059-64. [56 references] PubMed |
Not applicable: The guideline was not adapted from another source.
American Society of Colon and Rectal Surgeons
Standards Practice Task Force of the American Society of Colon and Rectal Surgeons
Primary Authors: David E. Rivadeneira, M.D.; Scott R. Steele, M.D.; Charles Ternent, M.D.; Sridhar Chalasani, M.D.; W. Donald Buie, M.D.; Janice L. Rafferty, M.D.
Contributing Members of the American Society of Colon and Rectal Surgeons (ASCRS) Standards Committee: W. Donald Buie, M.D. (Chair); Janice Rafferty, M.D., Co-Chair/Council Representative; Farshid Araghizadeh, M.D.; Robin Boushey, M.D.; George Chang, M.D.; Daniel Feingold, M.D.; Phillip Fleshner, M.D.; Jill Genua, M.D.; Sharon Gregorcyk, M.D.; Kerry Hammond, M.D.; William Harb, M.D.; Samantha Hendren, M.D.; Daniel Herzig, M.D.; Andreas Kaiser, M.D.; David Larson, M.D.; Sang Lee, M.D.; James McCormick, D.O.; Genevieve Melton-Meaux, M.D.; Steven Mills, M.D.; John Monson, M.D.; Harvey Moore III, M.D.; W. Brian Perry, M.D.; P. Terry Phang, M.D.; David Rivadeneira, M.D.; Howard Ross, M.D.; Sharon Dykes, M.D.; Scott Steele, M.D.; Scott Strong, M.D.; Charles Ternent, M.D.; Madhulika Varma, M.D.; Martin Weiser, M.D.; Kirsten Wilkins, M.D.
Not stated
This is the current release of the guideline.
This guideline updates a previous version: Cataldo P, Ellis CN, Gregorcyk S, Hyman N, Buie WD, Church J, Cohen J, Fleshner P, Kilkenny J 3rd, Ko C, Levien D, Nelson R, Newstead G, Orsay C, Perry WB, Rakinic J, Shellito P, Strong S, Ternent C, Tjandra J, Whiteford M. Practice parameters for the management of hemorrhoids (revised). Dis Colon Rectum 2005 Feb;48(2):189-94. [41 references]
Electronic copies: Available in Portable Document Format (PDF) from the American Society of Colon and Rectal Surgeons Web site ![]() .
.
Print copies: Available from the ASCRS, 85 W. Algonquin Road, Suite 550, Arlington Heights, Illinois 60005.
None available
The following is available:
- Hemorrhoids: expanded version. 2012. Available from the American Society of Colon and Rectal Surgeons Web site
 .
.
Please note: This patient information is intended to provide health professionals with information to share with their patients to help them better understand their health and their diagnosed disorders. By providing access to this patient information, it is not the intention of NGC to provide specific medical advice for particular patients. Rather we urge patients and their representatives to review this material and then to consult with a licensed health professional for evaluation of treatment options suitable for them as well as for diagnosis and answers to their personal medical questions. This patient information has been derived and prepared from a guideline for health care professionals included on NGC by the authors or publishers of that original guideline. The patient information is not reviewed by NGC to establish whether or not it accurately reflects the original guideline's content.
This summary was completed by ECRI on February 15, 2000. The information was verified by the guideline developer on November 7, 2000. This summary was updated by ECRI on July 15, 2005. This NGC summary was updated on April 24, 2012.
This NGC summary is based on the original guideline, which is subject to the guideline developer's copyright restrictions.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 