
Lars Grimm, MD, MHS Contributor Information
Skin rashes caused by bacterial, viral, or fungal etiologies are very common presenting complaints to primary care clinics, emergency departments, and dermatologists. Although many presenting symptoms overlap, discrete identifiable factors for each disease can help aid in diagnosis and treatment. For example, herpes zoster (shingles) is a dermal and neurologic disorder caused by reactivation of the varicella-zoster virus. Although radiation, trauma, medications, stress, or other infections have been proposed as triggers, no specific etiology has been clearly established. Zoster typically manifests with a prodrome of pain or anesthesia along a dermatomal distribution. Erythema, regional lymphadenopathy, and grouped herpetiform vesicles (shown) then develop. The cutaneous findings are typically unilateral and do not cross the midline.
Image courtesy of Wikipedia Commons.
In herpes zoster, vesicles are initially clear (shown), but then may become cloudy, rupture, crust, and involute. For some individuals, the pain does not resolve and may persist for years—a condition referred to as postherpetic neuralgia. Antiviral agents given early in the disease course may shorten the recovery period and decrease the chance of postherpetic neuralgia. A vaccine is available and is recommended by the Centers for Disease Control and Prevention for all individuals over the age of 60 years.
See if you can correctly diagnose the following rashes. This otherwise healthy 10-year-old girl was brought to her pediatrician for evaluation of patchy hair loss, which began as a red papule on the scalp over 2 weeks ago. On physical examination, the area is slightly pruritic and nontender. A solitary posterior cervical lymph node is noted. What is the most likely etiology of this skin lesion?
Image courtesy of Wikipedia Commons.
Answer: Tinea capitis
This boy has tinea capitis caused by an infection with the fungus Microsporum canis. Tinea capitis is considered to be a form of superficial mycosis or dermatophytosis and is the most common pediatric dermatophyte infection worldwide. Diagnosis depends on examination and culture of hair and skin scrapings.
A 9-year-old boy presented with the skin rash shown, accompanied by a low-grade fever and intense pruritus. What is the name of the virus and resultant rash? How is this virus transmitted?
Image courtesy of Wikipedia Commons.
Answer: Chickenpox, caused by the varicella zoster virus, which is highly contagious and acquired via inhalation of airborne respiratory droplets or direct vesicle contact.
This skin manifestation occurs mostly in children younger than 10 years. The viremia invades the capillary endothelial cells and epidermis producing inter- and intracellular edema, resulting in vesicle formation. The clear vesicles are surrounded by an erythematous halo (shown). Lesions will subsequently develop a central umbilication and crusting. On exam, vesicles in all stages of development are typically present. The disease typically resolves spontaneously, but adults may have significant morbidity and are often given antiviral medications.
Image courtesy of Wikipedia Commons.
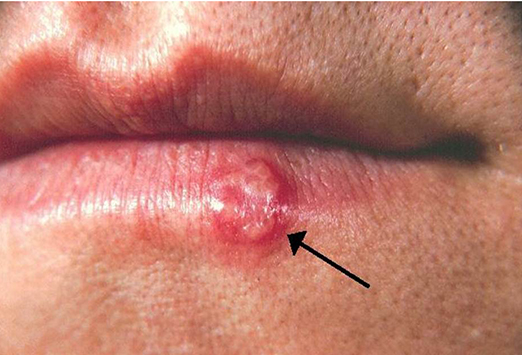
Herpes simplex viruses are DNA viruses that cause acute skin infections that present as grouped vesicles on an erythematous base (shown). Infection occurs from transmission of body fluids onto a mucous membrane or open skin from an actively shedding individual to a susceptible person. Most infections are self-limited but antiviral therapy, such as acyclovir, will shorten the course of symptoms and may help to prevent dissemination and transmission.
Image courtesy of Wikipedia Commons.
This patient presented with lesions appearing as firm, smooth, umbilicated papules, generally 2-6 mm in diameter. What is the cause of this skin manifestation?
Answer: Molluscum contagiosum
Molluscum contagiosum is a cutaneous infection caused by a large DNA poxvirus. Papules may be either clustered or widely distributed (shown). Lesions can be variable in color ranging from flesh, white, translucent, or yellow; range in number from one to several hundred; and may persist for several years. Transmission occurs via direct skin contact or by sharing towels, sports equipment, or benches. Most patients are asymptomatic, but others report pruritus, tenderness, and pain. Diagnosis is typically made on clinical grounds. Although typically self-limited, therapy may be appropriate for lesions that do not resolve after several months to prevent autoinoculation. Treatment options are non-FDA approved and include topical applications (eg, cantharidin, tretinoin cream), systemic agents (eg, griseofulvin, cimetidine, methisazone), and photodynamic therapy. The overall prognosis is typically excellent.
This patient presented with cutaneous lesions on the hands, feet, and buttocks. The 2-to 10-mm erythematous macules developed a central, gray, oval vesicle. The lesions are elliptical with the long axis parallel to skin lines. What is the cause of these skin lesions?
Image courtesy of Wikimedia Commons.
Answer: Hand-foot-and-mouth disease
Hand-foot-and-mouth disease is a viral illness with oral and distal extremity lesions. It is most commonly caused by a coxsackievirus infection. Infections are highly contagious leading to epidemics from direct contact with nasal and oral secretions or fecal material. Incubation typically averages 3-6 days. The oral lesions are typically 2-3 mm vesicles on an erythematous base. Care is typically supportive with antipyretics and anesthetics for symptomatic relief on a case by case basis.
Image courtesy of Wikimedia Commons.
This patient presented with an illness that has three distinct phases with a very mild prodrome. In the first phase (2-4 days), bright red erythema appears over the cheeks in a classic slapped-cheek appearance with sparing of the nasal, periorbital, and perioral regions (shown). In the second phase (1-4 days), an erythematous macular-to-morbilliform eruption occurs predominately on the extensor surfaces of the extremities. In the final stage (several days to weeks), the eruption fades, leaving behind a reticulated lacy pattern. What is the cause of this viral illness?
Image courtesy of Wikimedia Commons.
Answer: Erythema infectiosum
Erythema infectiosum, or fifth disease, is a common childhood exanthem caused by human parvovirus B19. Transmission is via aerosolized respiratory droplets with an incubation period of 4-14 days. The disease is typically self-limited and resolves without complications or sequelae in children, while adults may suffer significant morbidity. Some patients may develop arthralgia or pruritus, which can be treated with oral analgesics, antihistamines, or topical antipruritic lotions on a case-by-case basis.
Image courtesy of Wikimedia Commons.
This patient presented with complaints of a solitary, salmon-colored macule that enlarged over several days to become a patch with fine scales and a well-demarcated border. Over the next several weeks, a generalized xanthem developed with bilateral, symmetric macules, 0.5-1.5 cm in diameter, oriented along cleavage lines, with mild to moderate pruritus. What is the cause of this pruritic dermatologic manifestation?
Image courtesy of Wikimedia Commons.
Answer: Pityriasis rosea
Pityriasis rosea is a benign papulosquamous disease. It begins as a solitary macule that is 2-10 cm in diameter, termed a herald patch. The generalized xanthem typically lasts for 6 weeks. The exact etiologic organism is not known, but immunologic data suggests a viral etiology. Like many viral xanthems, the incidence increases in the fall and spring. Treatment is largely symptomatic for relief of pruritus with topical steroids, oral antihistamines, oatmeal baths, and topical menthol-phenol lotions. Oral steroids are not recommended. Rashes typically resolve within 12 weeks. Image courtesy of Wikimedia Commons.
This skin infection is generally limited to the epidermis and expands in a centrifugal pattern. Transmission is via direct skin-to-skin contact. Patients may be asymptomatic or complain of a pruritic or burning sensation. The lesion appears as an erythematous, scaly plaque that may enlarge rapidly (shown). Scales, crust, papules, vesicles, or bullae may develop along the advancing border. What is the cause of this skin manifestation?
Answer: Tinea
Tinea is a superficial dermatophyte infection characterized by inflammatory or noninflammatory lesions on the glabrous skin. Classification is based on the region of infection: pedis for feet, corporis for body, capitis for head, and cruris for groin. It may be caused by one of three dermatophytes: Trichophyton (most common), Microsporum, and Epidermophyton. The dermatophytes preferentially inhabit warm, moist environments. Diagnosis may be made with a KOH preparation from a skin scraping.
Image courtesy of Wikimedia Commons.
Treatment for tinea (shown) includes topical therapy with either an azole or allylamine, which is typically sufficient. Systemic therapy with an azole, griseofulvin, or terbinafine may be required for individuals with extensive skin infection, immunosuppression, resistance to topical therapies, or for tinea capitis.
Image courtesy of Wikipedia Commons.
Intertrigo (shown) is an inflammatory condition of skin folds, most commonly from candidal infection. Heat, moisture, maceration, friction, and lack of air circulation all provide ideal conditions for infection. It is most common in people who are diabetic or obese. Intertrigo is typically chronic in nature with patients reporting itching, burning, and stinging of infected areas. Erythema, weeping, maceration, crusting, fissuring, pustules, or vesicles may all be present depending on the duration of inflammation.
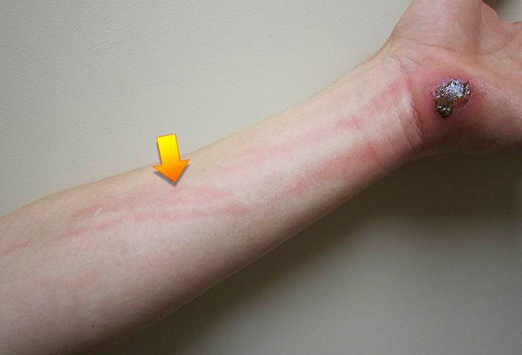
Cellulitis (shown) is a nonnecrotizing infection of the dermis and hypodermis. The most common organisms involved are Streptococcus pyogenes and Staphylococcus aureus. Small breaks in the skin allow for organisms to gain entrance to the dermis and multiply. In rare cases, hematogenous or metastatic seeding may occur. Patients typically report fevers, chills, pain, swelling, tenderness, erythema, and warmth. The borders of cellulitis are typically not elevated or sharply demarcated.
Lymphangitis (streaking-arrow) or regional lymphadenopathy may develop. Mild cases may be treated in an outpatient setting with oral antibiotics with activity against staphylococci and streptococci (eg, dicloxacillin, cephalexin, clindamycin, amoxicillin/clavulanate). Intravenous antibiotics are reserved for patients who are severely ill, with facial cellulitis, who are refractory to oral therapy, or who are immunosuppressed. There is a growing presence of community-acquired MRSA, requiring treatment with more potent antibiotics.
Image courtesy of Wikipedia Commons.
The infection shown typically occurs via skin breakage from excoriation or other skin diseases. It is characterized first by a red macule or papule 2-5 mm in size, which turns into a fragile vesicle that ruptures to become a honey-yellow crusted papule or plaque. An initial vesicle develops into a superficial flaccid bullae, 1 cm in size, with minimal surrounding erythema that eventually ruptures leaving behind a crusty scale (shown). Lesions are typically asymptomatic with occasional pain or pruritus. What is the cause of this dermatologic condition?
Image courtesy of Wikipedia Commons.
Answer: Impetigo
Impetigo is a gram-positive bacterial infection of the superficial layers of the epidermis. Impetigo may be bullous or non-bullous. The most common organisms identified are Staphylococcus aureus and group A beta-hemolytic streptococci. Infection typically occurs via skin breakage from excoriation or other skin diseases. Patients are either colonized in the anterior nares or organisms pass from one individual to another through direct hand contact. Treatment is typically with topical antibiotics, such as mupirocin.
The skin infection shown begins as a small erythematous patch that progresses to a fiery-red, indurated, tense, and shiny plaque. The margins are typically sharply demarcated. In severe infections, vesicles, bullae, petechiae, and frank necrosis may be found. What is this dermatologic manifestation called?
Image courtesy of Wikipedia Commons.
Answer: Erysipelas
Erysipelas is a superficial bacterial skin infection that extends into the cutaneous lymphatics. The most common bacteria responsible are streptococci. Infection occurs via inoculation into an area of local skin trauma. In severe infections, vesicles, bullae, petechiae, and frank necrosis may be found. Treatment for 10-20 days is recommended with penicillin (or a first-generation cephalosporin or macrolide in penicillin-allergic patients). Elevation and rest of the affected area may help reduce swelling. Saline wet dressing should be applied to ulcerated and necrotic lesions.
This dermatologic manifestation appeared as multiple small papules. Pustules on an erythematous base pierced by a central hair are found (shown). This patient had used a hot tub 2 days prior, wearing a bikini-style bathing suit. What is the name of this condition? What are the most common bacteria associated with this condition?
Answers: Folliculitis; Staphylococcus aureus
Folliculitis is inflammation within the wall and ostia of a hair follicle, creating a pustule. Many different causes have been identified, including infection, trauma, perspiration, and occlusion. The most common infectious organism is Staphylococcus aureus. However, gram-negative organisms are found in patients on chronic antibiotic therapy and Pseudomonas may be found in patients using hot tubs or wet suits. Folliculitis is typically self-limited and does not require treatment, but the use of antibacterial soaps is recommended for recurrent folliculitis.
Image courtesy of Wikipedia Commons.





























 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 