BMJ 2013;346:f3719
[EXCERPTS]
A 67 year old woman presents with recent onset of “palpitations,” lethargy, and shortness of breath, usually related to exercise. She experiences a fluttering in her chest and has hypertension and type 2 diabetes.
What you should cover
Atrial fibrillation is the commonest cardiac arrhythmia, increasing in frequency with age. It causes various symptoms including palpitations, lethargy, shortness of breath, and chest pain and increases the risk of stroke sixfold. It can be intermittent (paroxysmal) or continuous (persistent (>7 days to 1 year), longstanding persistent (>1 year), or permanent). Controlling symptoms is important, but reducing stroke risk is paramount.
Consider:
- Are the palpitations caused by atrial fibrillation?
- Do you need to refer the patient to hospital?
- Treatment to control the heart rate and improve symptoms.
- Stroke risk and stroke prevention strategies.
- Patient anxiety over symptoms and taking oral anticoagulants.
What you should do
Initial assessment
- Check the apical heart beat for the irregularly irregular rhythm of atrial fibrillation.
- Record ventricular rate, blood pressure, and heart sounds. Haemodynamically unstable patients require urgent admission.
- Ask about chest pain and shortness of breath.
- Ask about vascular events such as stroke, transient ischaemic attack, and peripheral emboli.
- Exclude and document other potential causes of symptoms: anaemia, myocardial infarction, pneumonia, and pulmonary embolus.
- Identify predisposing factors for atrial fibrillation and correct treatable causes.
Stroke risk assessment
- Annual risk of stroke can be calculated with CHADS2. Low risk patients who do not require any prophylaxis can be identified with the CHA2DS2-VASc index.
- Calculate the CHADS2 score from the presence of risk factors (table 1) then identify the annual stroke risk from the resultant score (table 2).
- Recommendations for treatment depend on the patient’s CHADS2 score (table 2).
- The risk of bleeding with oral anticoagulants (HAS-BLED) is increased by certain modifiable conditions (table 3): a score of ≥3 does not preclude anticoagulation but indicates greater caution in starting treatment and more regular review.
Table 1: CHADS2 and CHA2DS2-VASc scores for calculating annual risk of stroke
Table 2: Annual stroke risks calculated with CHADS2 and CHA2DS2-VASc scores, and associated treatment recommendations
*Number needed to treat with warfarin for 1 year to prevent 1 stroke.
Note: Aspirin is recognised by Quality and Outcomes Framework and NICE guidelines but is no longer a recommended treatment for thromboprophylaxis in patients with atrial fibrillation.
Table 3: HAS-BLED scoring system to identify patients at increased risk of haemorrhage and to identify modifiable risk factors
ALT=serum alanine aminotransferase. AST=serum aspartate aminotransferase. NSAID=non-steroidal anti-inflammatory drug. INR=international normalised ratio.
Investigations
- Confirm the diagnosis by 12 lead electrocardiography and to exclude abnormalities such as a short PR interval.
- Consider 24 hour electrocardiography, or event or loop recording, if paroxysmal atrial fibrillation is suspected.
- Blood tests (full blood count, urea and electrolytes test, liver function tests, thyroid function tests, clotting screen, fasting blood sugar (or HbA1c), and cholesterol levels).
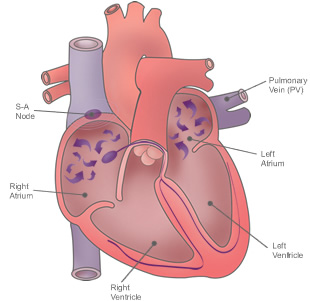
- Echocardiography is useful to assess left ventricular function or a suspected valvular defect.
Management
When to refer to cardiologist (or cardiac rhythm management specialist if available)
- Urgently if the patient has new onset atrial fibrillation (<48 hours) or there is haemodynamic instability.
- When the patient has paroxysmal atrial fibrillation for consideration of preventive medication.
- When there is difficulty achieving adequate rate control.
- If there is coexistent heart disease such as coronary or valvular heart disease.
- For consideration of cardioversion if:
- Symptoms remain despite adequate rate control
- Relatively young age (no definitive guideline but generally <60 years old)
- Atrial fibrillation related heart failure
- Atrial fibrillation secondary to a corrected cause.
Rate control
- Start immediately.
- Initially aim for lenient rate control with a resting apical heart rate <100-110 beats/min, but more stringent control may be required if symptoms remain (resting apical rate 80 beats/min).
- Start bisoprolol 2.5 mg (1.25 mg in elderly patients) and titrate upwards in increments of 1.25 mg every 1-2 weeks until target heart rate is achieved or until maximum tolerated dose (not more than 10 mg daily). ß blockers are contraindicated in acute heart failure, severe obstructive airways disease, asthma, and severe peripheral arterial disease. Symptoms of hypoglycaemia may be masked in diabetic patients.
- If ß blockers are not tolerated or contraindicated, alternatives include diltiazem (slow release, starting at 90 mg twice daily, increasing to 120 mg twice daily if heart rate remains uncontrolled) and verapamil (starting at 40 mg three times daily, titrating upwards in increments of 40 mg every 1-2 weeks and converting to a long acting preparation once heart rate is controlled). Both must be avoided in patients with impaired left ventricular function or already taking ß blockers.
- Digoxin is an alternative for elderly sedentary patients (>80 years old). Start at 62.5 µg daily and titrate upwards in increments of 62.5 µg every 1-2 weeks; the usual maintenance dose is 62.5-250 µg daily. Check urea and electrolytes before starting, after a dose change, and then annually. Monitor digoxin level at least 1 week after a dose change; subsequently only if toxicity is suspected.
Stroke risk reduction
- Start as soon as possible after diagnosis.
- Aspirin is no longer considered an appropriate treatment despite being a Quality and Outcomes Framework target.
- Low risk patients (see table 2) require no treatment.
- Higher risk patients are recommended oral anticoagulants, which can be started in primary care.
- Falls and risk of falls are not contraindications to oral anticoagulants, but investigation of falls is important before starting treatment.
- Warfarin within the target international normalised ratio (2.0-3.0) reduces stroke risk by 68% across all age ranges.
- Newer agents (dabigatran, rivaroxaban, and apixaban) are at least as effective as warfarin and do not require blood monitoring. Compared with warfarin, they reduce the risk of intracranial haemorrhage by nearly 50%, but slightly increase the risk of gastrointestinal haemorrhage. The effects of warfarin can be reversed with administration of vitamin K, but there is no known antidote to the newer agents if bleeding occurs.
- These newer agents are recommended by the National Institute for Health and Care Excellence (NICE) for patients with non-valvular atrial fibrillation and at least one other risk factor—such as congestive heart failure, hypertension, age ≥75 years, diabetes, or prior stroke or transient ischaemic attack
- Dabigatran dose: 150 mg twice a day, reduced to 110 mg twice a day in patients >80 years old
- Rivaroxaban dose: 20 mg with evening meal, reduced to 15 mg if creatinine clearance is 15-50 mL/min
- Apixaban dose: 5 mg twice a day, reduced to 2.5 mg twice a day if creatinine clearance is 15-30 mL/min, patient is >80 years old, creatinine concentration is >133 µmol, or body weight is <60 kg.
[Free full-text BMJ article with tables and references]





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 