Hypertension is highly prevalent in the adult population in the United States, especially among persons older than 60 years of age, and affects approximately 1 billion adults worldwide.1,2
Among persons 50 years of age or older, isolated systolic hypertension is the most common form of hypertension,3,4 and systolic blood pressure becomes more important than diastolic blood pressure as an independent risk predictor for coronary events, stroke, heart failure, and end-stage renal disease (ESRD).5-13 The Global Burden of Disease Study identified elevated blood pressure as the leading risk factor, among 67 studied, for death and disability-adjusted life-years lost during 2010.14
Clinical trials have shown that treatment of hypertension reduces the risk of cardiovascular disease outcomes, including incident stroke (by 35 to 40%), myocardial infarction (by 15 to 25%), and heart failure (by up to 64%).5,15,16 However, the target for systolic blood-pressure lowering is uncertain. Observational studies have shown a progressive increase in cardiovascular risk as systolic blood pressure rises above 115 mm Hg,10 but the available evidence from randomized, controlled trials in the general population of patients with hypertension only documents the benefit of treatment to achieve a systolic blood-pressure target of less than 150 mm Hg, with limited data concerning lower blood-pressure targets.11,17-21 In a trial involving patients with type 2 diabetes mellitus, the rate of major cardiovascular events was similar with a systolic blood-pressure target of less than 120 mm Hg and the commonly recommended target of less than 140 mm Hg, though the rate of stroke was lower with the target of less than 120 mm Hg.22 A recent trial involving patients who had had a stroke compared treatment to lower systolic blood pressure to less than 130 mm Hg with treatment to lower it to less than 150 mm Hg and showed no significant benefit of the lower target with respect to the overall risk of another stroke but a significant benefit with respect to the risk of hemorrhagic stroke.23
The hypothesis that a lower systolic blood-pressure goal (e.g., <120 mm Hg) would reduce clinical events more than a standard goal was designated by a National Heart, Lung, and Blood Institute (NHLBI) expert panel in 2007 as the most important hypothesis to test regarding the prevention of hypertension-related complications among patients without diabetes.24 The current article describes the primary results of the Systolic Blood Pressure Intervention Trial (SPRINT), which compared the benefit of treatment of systolic blood pressure to a target of less than 120 mm Hg with treatment to a target of less than 140 mm Hg.
METHODS
Study Design and Oversight
SPRINT was a randomized, controlled, open-label trial that was conducted at 102 clinical sites (organized into 5 clinical center networks) in the United States, including Puerto Rico (see the Supplementary Appendix, available with the full text of this article at NEJM.org). A trial coordinating center served as a data and biostatistical core center and supervised the central laboratory, the electrocardiography reading center, the magnetic resonance imaging reading center, and the drug-distribution center. The rationale and protocol for the trial are publicly available,25,26 and the protocol is available at NEJM.org.
SPRINT was sponsored by the NHLBI, with cosponsorship by the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Neurological Disorders and Stroke, and the National Institute on Aging. An independent data and safety monitoring board monitored unblinded trial results and safety events. The study was approved by the institutional review board at each participating study site. The steering committee designed the study, gathered the data (in collaboration with investigators at the clinics and other study units), made the decision to submit the manuscript for publication, and vouches for the fidelity of the study to the protocol. The writing committee wrote the manuscript and vouches for the completeness and accuracy of the data and analysis. The coordinating center was responsible for analyzing the data. Scientists at the National Institutes of Health participated in the design of the study and as a group had one vote on the steering committee of the trial.
Study Population
Participants were required to meet all the following criteria: an age of at least 50 years, a systolic blood pressure of 130 to 180 mm Hg (see the Supplementary Appendix), and an increased risk of cardiovascular events. Increased cardiovascular risk was defined by one or more of the following: clinical or subclinical cardiovascular disease other than stroke; chronic kidney disease, excluding polycystic kidney disease, with an estimated glomerular filtration rate (eGFR) of 20 to less than 60 ml per minute per 1.73 m2 of body-surface area, calculated with the use of the four-variable Modification of Diet in Renal Disease equation; a 10-year risk of cardiovascular disease of 15% or greater on the basis of the Framingham risk score; or an age of 75 years or older. Patients with diabetes mellitus or prior stroke were excluded. Detailed inclusion and exclusion criteria are listed in the Supplementary Appendix. All participants provided written informed consent.
Randomization and Interventions
Eligible participants were assigned to a systolic blood-pressure target of either less than 140 mm Hg (the standard-treatment group) or less than 120 mm Hg (the intensive-treatment group). Randomization was stratified according to clinical site. Participants and study personnel were aware of the study-group assignments, but outcome adjudicators were not.
After the participants underwent randomization, their baseline antihypertensive regimens were adjusted on the basis of the study-group assignment. The treatment algorithms were similar to those used in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial.22 These algorithms and our formulary are listed in Figures S1 and S2 and Table S1 in the Supplementary Appendix. All major classes of antihypertensive agents were included in the formulary and were provided at no cost to the participants. SPRINT investigators could also prescribe other antihypertensive medications (not provided by the study). The protocol encouraged, but did not mandate, the use of drug classes with the strongest evidence for reduction in cardiovascular outcomes, including thiazide-type diuretics (encouraged as the first-line agent), loop diuretics (for participants with advanced chronic kidney disease), and beta-adrenergic blockers (for those with coronary artery disease).5,27 Chlorthalidone was encouraged as the primary thiazide-type diuretic, and amlodipine as the preferred calcium-channel blocker.28,29 Azilsartan and azilsartan combined with chlorthalidone were donated by Takeda Pharmaceuticals International and Arbor Pharmaceuticals; neither company had any other role in the study.
Participants were seen monthly for the first 3 months and every 3 months thereafter. Medications for participants in the intensive-treatment group were adjusted on a monthly basis to target a systolic blood pressure of less than 120 mm Hg. For participants in the standard-treatment group, medications were adjusted to target a systolic blood pressure of 135 to 139 mm Hg, and the dose was reduced if systolic blood pressure was less than 130 mm Hg on a single visit or less than 135 mm Hg on two consecutive visits. Dose adjustment was based on a mean of three blood-pressure measurements at an office visit while the patient was seated and after 5 minutes of quiet rest; the measurements were made with the use of an automated measurement system (Model 907, Omron Healthcare). Lifestyle modification was encouraged as part of the management strategy. Retention in the study and adherence to treatment were monitored prospectively and routinely throughout the trial.26
Study Measurements
Demographic data were collected at baseline. Clinical and laboratory data were obtained at baseline and every 3 months thereafter. A structured interview was used in both groups every 3 months to obtain self-reported cardiovascular disease outcomes. Although the interviewers were aware of the study-group assignments, they used the same format for interviews in the two groups to minimize ascertainment bias. Medical records and electrocardiograms were obtained for documentation of events. Whenever clinical-site staff became aware of a death, a standard protocol was used to obtain information on the event.
Serious adverse events were defined as events that were fatal or life-threatening, that resulted in clinically significant or persistent disability, that required or prolonged a hospitalization, or that were judged by the investigator to represent a clinically significant hazard or harm to the participant that might require medical or surgical intervention to prevent one of the other events listed above.30,31 A short list of monitored conditions were reported as adverse events if they were evaluated in an emergency department: hypotension, syncope, injurious falls, electrolyte abnormalities, and bradycardia. We also monitored occurrences of acute kidney injury or acute renal failure if they were noted on admission or occurred during a hospitalization and were reported in the hospital discharge summary as a primary or main secondary diagnosis. The Medical Dictionary for Regulatory Activities was used to classify the safety events. Coding was performed at the coordinating center, and up to three codes were assigned to each safety event. The relationship of serious adverse events to the intervention was assessed by the trial safety officer and reviewed monthly by the safety committee.
Study Outcomes
Definitions of study outcomes are outlined in the Supplementary Appendix. A committee whose members were unaware of the study-group assignments adjudicated the clinical outcomes specified in the protocol. The primary hypothesis was that treatment to reach a systolic blood-pressure target of less than 120 mm Hg, as compared with a target of less than 140 mm Hg, would result in a lower rate of the composite outcome of myocardial infarction, acute coronary syndrome not resulting in myocardial infarction, stroke, acute decompensated heart failure, or death from cardiovascular causes. Secondary outcomes included the individual components of the primary composite outcome, death from any cause, and the composite of the primary outcome or death from any cause.
We also assessed renal outcomes, using a different definition for patients with chronic kidney disease (eGFR <60 ml per minute per 1.73 m2) at baseline and those without it. The renal outcome in participants with chronic kidney disease at baseline was a composite of a decrease in the eGFR of 50% or more (confirmed by a subsequent laboratory test) or the development of ESRD requiring long-term dialysis or kidney transplantation. In participants without chronic kidney disease at baseline, the renal outcome was defined by a decrease in the eGFR of 30% or more to a value of less than 60 ml per minute per 1.73 m2. Incident albuminuria, defined for all study participants by a doubling of the ratio of urinary albumin (in milligrams) to creatinine (in grams) from less than 10 at baseline to greater than 10 during follow-up, was also a prespecified renal outcome.
Prespecified subgroups of interest for all outcomes were defined according to status with respect to cardiovascular disease at baseline (yes vs. no), status with respect to chronic kidney disease at baseline (yes vs. no), sex, race (black vs. nonblack), age (<75 vs. ≥75 years), and baseline systolic blood pressure in three levels (≤132 mm Hg, >132 to <145 mm Hg, and ≥145 mm Hg). We also planned a comparison of the effects of systolic blood-pressure targets on incident dementia, changes in cognitive function, and cerebral small-vessel ischemic disease; these results are not presented here.
Statistical Analysis
We planned a 2-year recruitment period, with a maximum follow-up of 6 years, and anticipated a loss to follow-up of 2% per year. With an enrollment target of 9250 participants, we estimated that the trial would have 88.7% power to detect a 20% effect with respect to the primary outcome, assuming an event rate of 2.2% per year in the standard-treatment group.
Our primary analysis compared the time to the first occurrence of a primary outcome event between the two study groups with the use of the intention-to-treat approach for all randomly assigned participants; for this analysis, we used Cox proportional-hazards regression with two-sided tests at the 5% level of significance, with stratification according to clinic. Follow-up time was censored on the date of last event ascertainment. Interactions between treatment effect and prespecified subgroups were assessed with a likelihood-ratio test for the interaction with the use of Hommel-adjusted P values.32 Interim analyses were performed for each meeting of the data and safety monitoring board, with group-sequential stopping boundaries defined with the use of the Lan–DeMets method with an O’Brien–Fleming–type spending function.33 The Fine–Gray model for the competing risk of death was used as a sensitivity analysis.34
RESULTS
Study Participants
A total of 9361 participants were enrolled between November 2010 and March 2013 (Figure 1
FIGURE 1Eligibility, Randomization, and Follow-up.). Descriptive baseline statistics are presented in Table 1
 TABLE 1Baseline Characteristics of the Study Participants.. On August 20, 2015, the NHLBI director accepted a recommendation from the data and safety monitoring board of the trial to inform the investigators and participants of the cardiovascular-outcome results after analyses of the primary outcome exceeded the monitoring boundary at two consecutive time points (Fig. S3 in the Supplementary Appendix), thus initiating the process to end the blood-pressure intervention early. The median follow-up on August 20, 2015, was 3.26 years of the planned average of 5 years.
TABLE 1Baseline Characteristics of the Study Participants.. On August 20, 2015, the NHLBI director accepted a recommendation from the data and safety monitoring board of the trial to inform the investigators and participants of the cardiovascular-outcome results after analyses of the primary outcome exceeded the monitoring boundary at two consecutive time points (Fig. S3 in the Supplementary Appendix), thus initiating the process to end the blood-pressure intervention early. The median follow-up on August 20, 2015, was 3.26 years of the planned average of 5 years.
Blood Pressure
The two treatment strategies resulted in a rapid and sustained between-group difference in systolic blood pressure (Figure 2
FIGURE 2Systolic Blood Pressure in the Two Treatment Groups over the Course of the Trial.). At 1 year, the mean systolic blood pressure was 121.4 mm Hg in the intensive-treatment group and 136.2 mm Hg in the standard-treatment group, for an average difference of 14.8 mm Hg. The mean diastolic blood pressure at 1 year was 68.7 mm Hg in the intensive-treatment group and 76.3 mm Hg in the standard-treatment group (Fig. S4 in the Supplementary Appendix). Throughout the 3.26 years of follow-up, the mean systolic blood pressure was 121.5 mm Hg in the intensive-treatment group and 134.6 mm Hg in the standard-treatment group, and the mean number of blood-pressure medications was 2.8 and 1.8, respectively. The relative distribution of antihypertensive medication classes used was similar in the two groups, though the use of each class was greater in the intensive-treatment group (Table S2 in the Supplementary Appendix).
Clinical Outcomes
A primary outcome event was confirmed in 562 participants — 243 (1.65% per year) in the intensive-treatment group and 319 (2.19% per year) in the standard-treatment group (hazard ratio with intensive treatment, 0.75; 95% confidence interval [CI], 0.64 to 0.89; P<0.001) (Table 2
TABLE 2Primary and Secondary Outcomes and Renal Outcomes.). Separation in the primary outcome between the groups was apparent at 1 year (Figure 3A
FIGURE 3Primary Outcome and Death from Any Cause.). The between-group differences were consistent across the components of the primary outcome and other prespecified secondary outcomes (Table 2).
A total of 365 deaths occurred — 155 in the intensive-treatment group and 210 in the standard-treatment group (hazard ratio, 0.73; 95% CI, 0.60 to 0.90; P=0.003). Separation in mortality between the groups became apparent at approximately 2 years (Figure 3B). Causes of death are provided in Table S3 in the Supplementary Appendix. The relative risk of death from cardiovascular causes was 43% lower with the intensive intervention than with the standard treatment (P=0.005) (Table 2).
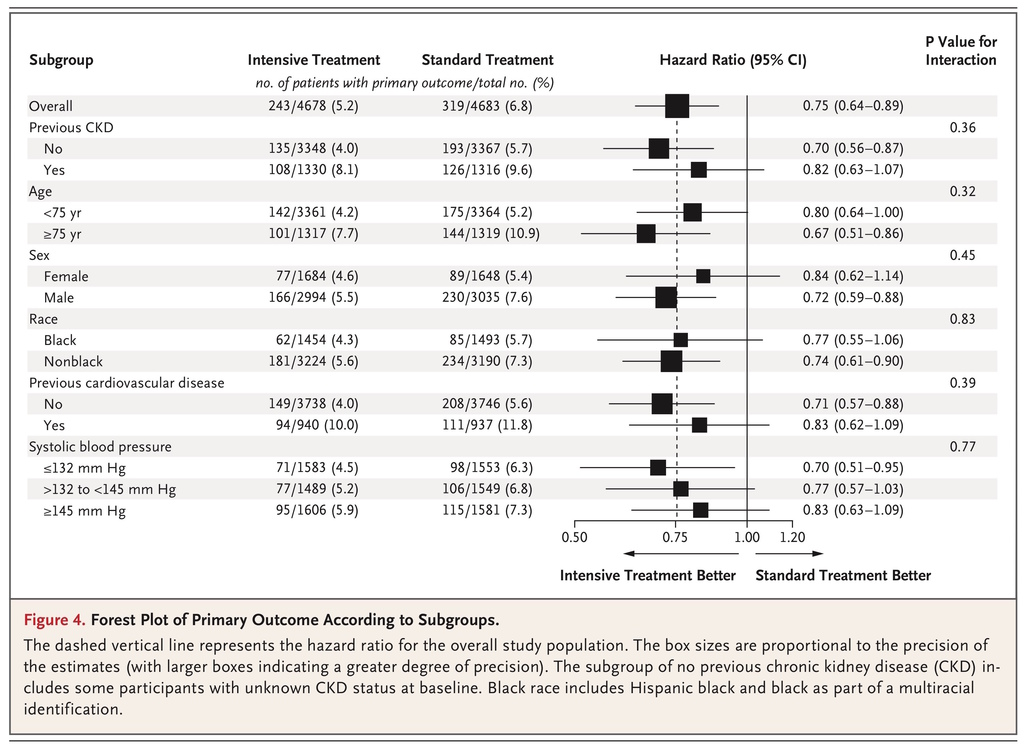
The numbers needed to treat to prevent a primary outcome event, death from any cause, and death from cardiovascular causes during the median 3.26 years of the trial were 61, 90, and 172, respectively. The effects of the intervention on the rate of the primary outcome and on the rate of death from any cause were consistent across the prespecified subgroups (Figure 4
FIGURE 4Forest Plot of Primary Outcome According to Subgroups., and Fig. S5 in the Supplementary Appendix). There were no significant interactions between treatment and subgroup with respect to the primary outcome or death from any cause. When death was treated as a competing risk in a Fine–Gray model, the results with respect to the primary outcome were virtually unchanged (hazard ratio, 0.76; 95% CI, 0.64 to 0.89).
Among participants who had chronic kidney disease at baseline, no significant between-group difference in the composite outcome of a decrease in the eGFR of 50% or more or the development of ESRD was noted, though the number of events was small (Table 2). Among participants who did not have chronic kidney disease at baseline, the incidence of the outcome defined by a decrease in the eGFR of 30% or more to a value of less than 60 ml per minute per 1.73 m2 was higher in the intensive-treatment group than in the standard-treatment group (1.21% per year vs. 0.35% per year; hazard ratio, 3.49; 95% CI, 2.44 to 5.10; P<0.001).
Serious Adverse Events
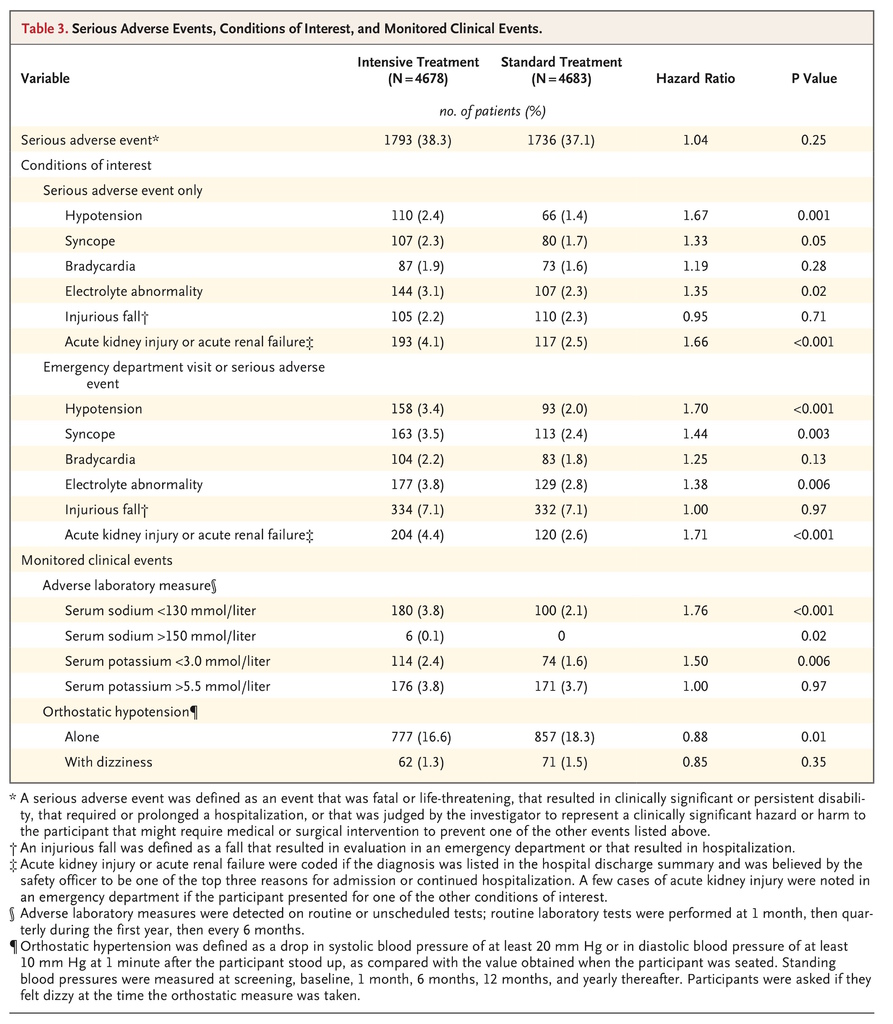
Serious adverse events occurred in 1793 participants in the intensive-treatment group (38.3%) and in 1736 participants in the standard-treatment group (37.1%) (hazard ratio with intensive treatment, 1.04; P=0.25) (Table 3
TABLE 3Serious Adverse Events, Conditions of Interest, and Monitored Clinical Events., and Table S4 in the Supplementary Appendix). Serious adverse events of hypotension, syncope, electrolyte abnormalities, and acute kidney injury or acute renal failure, but not injurious falls or bradycardia, occurred more frequently in the intensive-treatment group than in the standard-treatment group. Orthostatic hypotension as assessed during a clinic visit was significantly less common in the intensive-treatment group. A total of 220 participants in the intensive-treatment group (4.7%) and 118 participants in the standard-treatment group (2.5%) had serious adverse events that were classified as possibly or definitely related to the intervention (hazard ratio, 1.88; P<0.001) (Table S5 in the Supplementary Appendix). The magnitude and pattern of differences in adverse events according to treatment assignment among participants 75 years of age or older were similar to those in the overall cohort (Table S6 in the Supplementary Appendix).
DISCUSSION
SPRINT showed that among adults with hypertension but without diabetes, lowering systolic blood pressure to a target goal of less than 120 mm Hg, as compared with the standard goal of less than 140 mm Hg, resulted in significantly lower rates of fatal and nonfatal cardiovascular events and death from any cause. Trial participants assigned to the lower systolic blood-pressure target (intensive-treatment group), as compared with those assigned to the higher target (standard-treatment group), had a 25% lower relative risk of the primary outcome; in addition, the intensive-treatment group had lower rates of several other important outcomes, including heart failure (38% lower relative risk), death from cardiovascular causes (43% lower relative risk), and death from any cause (27% lower relative risk). During the follow-up period of the trial (median, 3.26 years), the number needed to treat with a strategy of intensive blood-pressure control to prevent one primary outcome event was 61, and the number needed to treat to prevent one death from any cause was 90. These benefits with respect to both the primary outcome and death were consistent across all prespecified subgroups, including participants 75 years of age or older.
Owing in part to a lower-than-expected decline in the eGFR and to the early termination of the trial, the number of renal events was small. Among participants who had chronic kidney disease at baseline, the number of participants with a decrease in the eGFR of 50% or more or reaching ESRD over the course of the trial did not differ significantly between the two intervention groups. Among participants who did not have chronic kidney disease at baseline, a decrease in the eGFR of 30% or more to a value of less than 60 ml per minute per 1.73 m2 occurred more frequently in the intensive-treatment group than in the standard-treatment group (1.21% per year vs. 0.35% per year). Among all participants, acute kidney injury or acute renal failure occurred more frequently in the intensive-treatment group than in the standard-treatment group (Table 3, and Table S5 in the Supplementary Appendix). The differences in adverse renal outcomes may be related to a reversible intrarenal hemodynamic effect of the greater reduction in blood pressure and greater use of diuretics, angiotensin-converting–enzyme inhibitors, and angiotensin-receptor blockers in the intensive-treatment group.35,36 With the currently available data, there is no evidence of substantial permanent kidney injury associated with the lower systolic blood-pressure goal; however, the possibility of a long-term adverse renal outcome cannot be excluded. These observations and hypotheses need to be explored further in analyses that incorporate more clinical outcomes and longer follow-up.
The results of SPRINT add substantially to the evidence of benefits of lowering systolic blood pressure, especially in older patients with hypertension. Trials such as the Systolic Hypertension in the Elderly Program trial,17 the Systolic Hypertension in Europe trial,11 and the Hypertension in the Very Elderly Trial18 showed the benefits of lowering systolic blood pressure below 150 mm Hg. However, trials evaluating systolic blood-pressure levels lower than those studied in these trials have been either underpowered19-21 or performed without specific systolic blood-pressure targets.37 A major component of the controversy regarding the selection of the systolic blood-pressure goal in this population has resulted from inadequate data on the risks versus benefits of systolic blood-pressure targets below 150 mm Hg.11,17-21,37 SPRINT now provides evidence of benefits for an even lower systolic blood-pressure target than that currently recommended in most patients with hypertension.
Comparisons between SPRINT and the ACCORD trial22 are inevitable, because the trials examined identical systolic blood-pressure targets (<120 mm Hg vs. <140 mm Hg). In contrast to the findings of SPRINT, the cardiovascular and mortality benefits observed in the ACCORD trial were not statistically significant and were of a lesser magnitude. Several important differences between these trials should be noted. The ACCORD trial enrolled participants with diabetes exclusively, whereas SPRINT excluded participants with diabetes; in addition, the sample size of the ACCORD trial was only half that of SPRINT (4733 vs. 9361). SPRINT enrolled an older cohort (mean age, 68 years, vs. 62 years in the ACCORD trial), with 28% of participants 75 years of age or older, and also included participants with chronic kidney disease. The ACCORD trial showed a (nonsignificant) 12% lower risk of its primary composite cardiovascular outcome, with a 95% confidence interval that included the possibility of a 27% lower risk, which is consistent with the cardiovascular benefit observed in SPRINT. The ACCORD trial also used a factorial design that included comparisons of standard and intensive glycemic and lipid treatment targets in the same trial. A secondary analysis of the ACCORD results showed that, as compared with the combined standard glycemia and blood-pressure treatments, intensive blood-pressure treatment alone reduced major cardiovascular outcomes by 26% without additional benefit from combining the two intensive treatments.38 Thus, the difference in results between the trials could be due to differences in study design, treatment interactions, or the play of chance. An inherent difference in the cardiovascular benefits of systolic blood-pressure lowering between the population with diabetes and the population without diabetes seems unlikely but cannot be ruled out.
In the Secondary Prevention of Small Subcortical Strokes trial (intensive systolic blood-pressure goal <130 mm Hg)23 and in the ACCORD trial (intensive systolic blood-pressure goal <120 mm Hg), the lower blood-pressure target was associated with a nonsignificant 19% lower incidence of stroke (P=0.08) and a significant 41% lower incidence of stroke, respectively, than the incidence with higher targets. The intensive-treatment group in SPRINT had a nonsignificant 11% lower incidence of stroke, though SPRINT also excluded persons with prevalent stroke or transient ischemic attack at baseline.
In SPRINT, significant between-group differences were noted in some adverse effects that were attributed to the intervention (Table S5 in the Supplementary Appendix). Orthostatic hypotension as assessed during a clinic visit (Table 3) was observed less frequently in the intensive-treatment group than in the standard-treatment group (P=0.01), but syncope was more common among participants in the intensive-treatment group than among those in the standard-treatment group (3.5% vs. 2.4%, P=0.003), as was hypotension (3.4% vs. 2.0%, P<0.001). There was no between-group difference in injurious falls (hazard ratio, 1.00; P=0.97). There was a higher rate of acute kidney injury or acute renal failure in the intensive-treatment group, as noted above. These adverse events need to be weighed against the benefits with respect to cardiovascular events and death that are associated with intensive control of systolic blood pressure.
The strengths of SPRINT include a large sample size, the diversity of the population (including a large proportion of patients 75 years of age or older), and its success in achieving the intended separation in systolic blood pressure between the two intervention groups throughout the trial. The lack of generalizability to populations not included in the study — such as persons with diabetes, those with prior stroke, and those younger than 50 years of age — is a limitation. It is also worth noting that we did not enroll older adults residing in nursing homes or assisted-living facilities. In addition, the effects of the lower blood pressure on the central nervous system and kidney cannot be reasonably interpreted until analysis of these end points has been completed.
The SPRINT results raise important practical issues. Hypertension control to a blood pressure of less than 140/90 mm Hg is achieved in only about 50% of the general population in the United States, which suggests that control to even that level is challenging.39 We excluded patients with more severe hypertension, and control of systolic blood pressure to less than 120 mm Hg required, on average, one additional antihypertensive drug. In addition, the median systolic blood pressure in the intensive-treatment group was just above 120 mm Hg, which indicates that more than half the participants had a systolic blood pressure above the 120 mm Hg target. These observations suggest that achieving a systolic blood-pressure goal of less than 120 mm Hg in the overall population of patients with hypertension would be more demanding and time-consuming for both providers and patients than achieving a goal of 140 mm Hg, and would necessitate increased medication costs and clinic visits.
In conclusion, targeting a systolic blood pressure of less than 120 mm Hg, as compared with less than 140 mm Hg, in patients at high risk for cardiovascular events but without diabetes resulted in lower rates of fatal and nonfatal major cardiovascular events and death from any cause. However, some adverse events occurred significantly more frequently with the lower target.









 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 