Published - Written by Carla Rothaus
Are there any targeted therapies for keratinocyte carcinomas?
Basal-cell carcinoma and cutaneous squamous-cell carcinoma are the most common skin cancers worldwide. Although the term “nonmelanoma skin cancer” has traditionally been used to refer to all skin cancers except melanoma, “keratinocyte carcinoma” is becoming the preferred term for basal-cell carcinoma and cutaneous squamous-cell carcinoma because of the shared lineage with epidermal keratinocytes. The dramatic rise in the incidence of keratinocyte carcinoma is an important public health concern, with more than $1 billion in annual treatment expenditures. Read the latest review article here.
Clinical Pearls
Q: Is mortality equally low for basal-cell carcinoma and cutaneous squamous-cell carcinoma?
A: Although mortality from basal-cell carcinoma remains exceedingly low, the estimated annual number of deaths from cutaneous squamous-cell carcinoma in the United States was 2500 in one study and more than 8000 in another study. Mortality from cutaneous squamous-cell carcinoma is likely to be underreported and may approach mortality from melanoma, particularly in geographic areas with high exposure to ultraviolet (UV) radiation.
Q: How does immunosuppression affect the risk of keratocyte carcinoma?
A: UV radiation, particularly among fair-skinned persons, is the primary etiologic agent for keratinocyte carcinomas. Immunosuppression is another risk factor for the development of keratinocyte carcinoma, especially cutaneous squamous-cell carcinoma. Long-term immunosuppressive therapy in recipients of solid-organ transplants is associated with a risk of cutaneous squamous-cell carcinoma that is increased by a factor of 100, as compared with the risk in the general population, and is also associated with higher rates of metastasis and mortality.
Morning Report Questions
Q: How are high-risk keratinocyte carcinomas managed?
A: For low-risk basal-cell carcinoma and low-risk cutaneous squamous-cell carcinoma, standard excision or ablative treatment with electrodesiccation and curettage is generally recommended, which in experienced hands yields very high cure rates. High-risk basal-cell carcinoma and high-risk cutaneous squamous-cell carcinoma are best managed with surgical techniques that include complete peripheral and deep margin assessment, such as Mohs micrographic surgery, a procedure in which microscopic examination of excised tissue occurs during surgery and the extent of the excision can be defined precisely rather than approximated. Mohs surgery results in high cure rates and maximum tissue conservation, particularly in anatomically and cosmetically sensitive locations on the head and neck. A randomized, controlled trial with 10 years of follow-up confirmed the benefit of Mohs micrographic surgery for both primary and recurrent basal-cell carcinoma on the face. Adjuvant radiation therapy may be considered after margin-negative excision of high-risk basal-cell carcinoma or cutaneous squamous-cell carcinoma, but definitive indications are not well established. Primary radiation therapy may be considered for patients who are not candidates for surgery.
Q: Are there any targeted therapies for keratinocyte carcinomas?
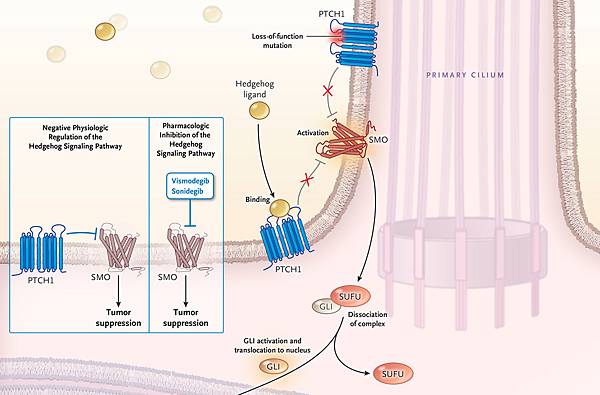
A: Identification of variants in the patched 1 gene (PTCH1) two decades ago as the causative mutant gene in patients with Gorlin’s syndrome (a rare autosomal dominant disorder characterized by multiple basal-cell carcinomas that develop at an early age) has been critical for an understanding of the molecular pathogenesis of basal-cell carcinoma and the development of targeted therapy. PTCH1, located on human chromosome 9q22, encodes a transmembrane protein that negatively regulates the hedgehog signaling pathway and functions as a classic tumor-suppressor gene. In Gorlin’s syndrome and the majority of sporadic basal-cell carcinomas, a loss-of-function mutation in PTCH1 leads to uninhibited activation of the hedgehog signaling pathway, resulting in tumor formation. Vismodegib, an antagonist of transmembrane protein smoothened homologue (SMO) that inhibits the hedgehog signaling pathway, was approved by the Food and Drug Administration in 2012 for the treatment of adults with locally advanced or metastatic basal-cell carcinoma who are not eligible for surgery and radiation therapy. A similar SMO inhibitor, sonidegib, was approved in 2015. Although attempts have been made to identify mutations that are predictive of cutaneous squamous-cell carcinomas with aggressive behavior or metastatic potential, current knowledge has not yet led to the development of targeted therapy, as it has for basal-cell carcinoma.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 