Associations of Dietary Cholesterol or Egg Consumption With Incident Cardiovascular Disease and Mortality
JAMA.
Key Points
Question Is consuming dietary cholesterol or eggs associated with incident cardiovascular disease (CVD) and all-cause mortality?
Findings Among 29 615 adults pooled from 6 prospective cohort studies in the United States with a median follow-up of 17.5 years, each additional 300 mg of dietary cholesterol consumed per day was significantly associated with higher risk of incident CVD (adjusted hazard ratio [HR], 1.17; adjusted absolute risk difference [ARD], 3.24%) and all-cause mortality (adjusted HR, 1.18; adjusted ARD, 4.43%), and each additional half an egg consumed per day was significantly associated with higher risk of incident CVD (adjusted HR, 1.06; adjusted ARD, 1.11%) and all-cause mortality (adjusted HR, 1.08; adjusted ARD, 1.93%).
Meaning Among US adults, higher consumption of dietary cholesterol or eggs was significantly associated with higher risk of incident CVD and all-cause mortality in a dose-response manner.
Importance Cholesterol is a common nutrient in the human diet and eggs are a major source of dietary cholesterol. Whether dietary cholesterol or egg consumption is associated with cardiovascular disease (CVD) and mortality remains controversial.
Objective To determine the associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality.
Design, Setting, and Participants Individual participant data were pooled from 6 prospective US cohorts using data collected between March 25, 1985, and August 31, 2016. Self-reported diet data were harmonized using a standardized protocol.
Exposures Dietary cholesterol (mg/day) or egg consumption (number/day).
Main Outcomes and Measures Hazard ratio (HR) and absolute risk difference (ARD) over the entire follow-up for incident CVD (composite of fatal and nonfatal coronary heart disease, stroke, heart failure, and other CVD deaths) and all-cause mortality, adjusting for demographic, socioeconomic, and behavioral factors.
Results This analysis included 29 615 participants (mean [SD] age, 51.6 [13.5] years at baseline) of whom 13 299 (44.9%) were men and 9204 (31.1%) were black. During a median follow-up of 17.5 years (interquartile range, 13.0-21.7; maximum, 31.3), there were 5400 incident CVD events and 6132 all-cause deaths. The associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality were monotonic (all P values for nonlinear terms, .19-.83). Each additional 300 mg of dietary cholesterol consumed per day was significantly associated with higher risk of incident CVD (adjusted HR, 1.17 [95% CI, 1.09-1.26]; adjusted ARD, 3.24% [95% CI, 1.39%-5.08%]) and all-cause mortality (adjusted HR, 1.18 [95% CI, 1.10-1.26]; adjusted ARD, 4.43% [95% CI, 2.51%-6.36%]). Each additional half an egg consumed per day was significantly associated with higher risk of incident CVD (adjusted HR, 1.06 [95% CI, 1.03-1.10]; adjusted ARD, 1.11% [95% CI, 0.32%-1.89%]) and all-cause mortality (adjusted HR, 1.08 [95% CI, 1.04-1.11]; adjusted ARD, 1.93% [95% CI, 1.10%-2.76%]). The associations between egg consumption and incident CVD (adjusted HR, 0.99 [95% CI, 0.93-1.05]; adjusted ARD, −0.47% [95% CI, −1.83% to 0.88%]) and all-cause mortality (adjusted HR, 1.03 [95% CI, 0.97-1.09]; adjusted ARD, 0.71% [95% CI, −0.85% to 2.28%]) were no longer significant after adjusting for dietary cholesterol consumption.
Conclusions and Relevance Among US adults, higher consumption of dietary cholesterol or eggs was significantly associated with higher risk of incident CVD and all-cause mortality in a dose-response manner. These results should be considered in the development of dietary guidelines and updates.
The associations between dietary cholesterol consumption and cardiovascular disease (CVD) and mortality remain controversial despite decades of research.1 The debate has intensified recently due to the inclusion of 2 seemingly contradictory statements in the 2015-2020 Dietary Guidelines for Americans2,3: (1) “Cholesterol is not a nutrient of concern for overconsumption”; and (2) “Individuals should eat as little dietary cholesterol as possible while consuming a healthy eating pattern.” The most recent meta-analysis of prospective cohort studies could not draw meaningful conclusions about the association between dietary cholesterol consumption and CVD, primarily due to sparse data, between-study heterogeneity, and lack of methodologic rigor of the reviewed studies.1
Cholesterol, saturated fat, and animal protein often coexist in foods.2 The interaction and independence between dietary cholesterol and these nutrients in relation to CVD and mortality remain uncertain. Further, it is unclear whether eating an overall high-quality diet attenuates the associations of dietary cholesterol consumption with CVD and mortality or if the food source of cholesterol (eg, eggs, red meat, poultry, fish, and dairy products) is important. Eggs, specially the yolk, are a major source of dietary cholesterol; a large egg (≈50 g) contains approximately 186 mg of cholesterol.4 Reported associations of egg consumption with CVD and mortality have been inconsistent overall and by subtypes of these events.5-10
Individual participant data were pooled from 6 cohorts from the Lifetime Risk Pooling Project to address the aforementioned gaps.11 The primary objective was to determine the associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality.
This study was approved by the institutional review board at Northwestern University. Written informed consent was obtained from all participants for initial data collection in each original cohort. For this analysis of deidentified data, specific consent was not required.
The Lifetime Risk Pooling Project included 20 community-based prospective cohorts of US participants primarily for the study of long-term risks and development patterns of CVD over the life course in adults.11 Six cohorts that each assessed usual dietary intake and had information on key study variables (see following Methods subsections) were included in this analysis. The cohorts were the Atherosclerosis Risk in Communities (ARIC) Study,12 Coronary Artery Risk Development in Young Adults (CARDIA) Study,13 Framingham Heart Study (FHS),14 Framingham Offspring Study (FOS),15 Jackson Heart Study (JHS),16 and the Multi-Ethnic Study of Atherosclerosis (MESA).17 Participants were excluded if they had CVD at baseline, self-reported energy intake less than 500 kcal per day or greater than 6000 kcal per day, or had missing data for any of the study variables.
Using a standardized protocol and data dictionary, diet data were harmonized cohort by cohort. Briefly, consumption frequencies were converted into estimated number per day using the middle value (eg, 3-4 times per week = 0.5 times per day). One serving unit was standardized across cohorts. Food groups were constructed using the same definitions. Ingredients in mixed dishes were considered and the appropriate portions were determined for each cohort. The first available diet data collection visit was defined as baseline ranging between 1985 in CARDIA and 2005 in JHS. Only baseline measures were included for this study. Additional details are provided in the eAppendix in the Supplement.
The primary outcomes were incident CVD and all-cause mortality. Incident CVD was a composite end point of fatal and nonfatal coronary heart disease (0), stroke, heart failure, and CVD death from other causes. Secondary outcomes were CHD, stroke, heart failure, CVD mortality, and non-CVD mortality. The included cohorts used similar ascertainment and adjudication criteria for CVD and mortality events. Vital status was known for 98% of the participants. The adjudication criteria included International Classification of Diseases codes (versions 8, 9, or 10); diagnostic procedures; and review of medical records, autopsy data, or both. Methods for adjudication have been described in ARIC,12 CARDIA,18 FHS,19FOS,19 JHS,20 and MESA,17 as well as in the Lifetime Risk Pooling Project.11,21-23 The most recent follow-up ended on August 31, 2016.
Standardized questionnaires and laboratory protocols were used to collect information on the following variables: age, sex, race/ethnicity, education, lifestyle factors (including smoking, alcohol intake, and physical activity), body mass index (BMI, calculated as weight in kilograms divided by height in meters squared), blood pressure, lipid profile, medication use, and medical conditions. These details have been described elsewhere for each cohort.11-17 The earliest baseline date was March 25, 1985. Race/ethnicity was self-reported and dichotomized as black and nonblack for subgroup analysis (race/ethnicity breakdown of participants: white [62.1%], black [31.1%], Hispanic [4.4%], Chinese [2.4%]).
Cohort-stratified cause-specific hazard models were used to determine the associations of dietary cholesterol or egg consumption with incident CVD, CVD subtypes, and cause-specific mortality. Cause-specific hazard models take into consideration competing risks by removing individuals who develop a competing event from the risk set; this technique has been recommended for studying the etiology of an association in the presence of competing risks.24,25 Cohort-stratified standard proportional hazard models were used for analyzing all-cause mortality outcome. Proportional hazards assumption was tested using the Kolmogorov-type supremum test.26 There was no evidence of violation of the proportionality assumption (P value > .05) except for the association between egg consumption and mortality, which was corrected by conducting cohort- and sex-stratified analyses. Models were sequentially adjusted for age, sex, race/ethnicity (white, black, Hispanic, Chinese), education (<high school, high school, some college or more) (model 1); plus total energy, smoking status (current, former, never), smoking pack-years (0, 0.1-4.9, 5.0-9.9, 10-19.9, 20-29.9, 30-39.9, ≥40), cohort-specific physical activity z score, alcohol intake (gram), use of hormone therapy (y/n) (model 2); plus BMI, diabetes status (y/n), systolic blood pressure, use of antihypertensive medications (y/n), high-density lipoprotein (0) cholesterol, non-HDL cholesterol, and use of lipid-lowering medications (y/n) (model 3). Model 2 was the primary model because model 3 risk factors may be in the causal pathway. To increase the applicability of the study results to the contemporary US population, the interpretation was based on consuming each additional 300 mg of dietary cholesterol per day or half an egg per day (equivalent to consumption of 1 egg 3-4 times per week or total consumption of 3-4 eggs per week) because mean dietary cholesterol consumption in the United States was 293 mg per day27 and mean egg consumption was 25.5 g per day28 based on data from recent National Health and Nutrition Examination Survey. One large egg weighs approximately 50 g.4 Estimates were also provided based on other units: each 50-mg per day dietary cholesterol increment up to 600 mg per day and each 1-egg per week increment up to 2 eggs per day. To test for statistically significant departure from a linear association, polynomial terms were added to model 2. If model fit was significantly improved, exposures were converted into 5-category variables. Otherwise, dietary exposures were included as single linear terms on each exposure’s original measurement scale. The distributions of dietary cholesterol or egg consumption were winsorized at the 0.5 and 99.5 percentiles before modeling.
To evaluate the associations of dietary cholesterol consumption with incident CVD and all-cause mortality, nutrients correlated with dietary cholesterol (saturated fat, unsaturated fat, trans fat, animal protein, fiber, and sodium) were adjusted individually or in combination, in addition to model 2 covariates. To determine if certain cholesterol-containing foods were major determinants for the associations, eggs, processed meat, unprocessed red meat, fish, poultry, and total dairy products were adjusted individually or in combination. For the associations of egg consumption with incident CVD and all-cause mortality, dietary cholesterol consumption was further adjusted.
To further evaluate whether consuming dietary cholesterol or eggs within different dietary patterns altered the associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality, major food groups were adjusted in addition to model 2 covariates, either individually or incorporated into 3 scores: the alternate Healthy Eating Index 2010 (aHEI-2010) score,29 alternate Mediterranean diet score,30 and Dietary Approaches to Stop Hypertension score.31 Cholesterol-containing foods such as meat and fish were removed from calculating these scores. All aforementioned analyses were performed for incident CVD overall, as well as separately by event-type (CHD, stroke, heart failure), and for all-cause mortality, CVD mortality, and non-CVD mortality.
Subgroup analyses were performed for incident CVD and all-cause mortality outcomes by the following variables: age (<65, ≥65 years), sex (men, women), race/ethnicity (black, non-black), smoking status (never, former, current), weight status (normal/underweight [BMI <25], overweight [BMI ≥25-<30], obese [BMI ≥30]), diabetes (y/n; defined as having fasting glucose ≥126 mg/dL or HbA1c ≥6.5% or taking glucose-lowering medications), hypertension (y/n; defined as ≥140/90 mm Hg or taking antihypertensive medications), hyperlipidemia (y/n; defined as having total cholesterol ≥240 mg/dL or taking lipid-lowering medications), low lipids (y/n; defined as not taking lipid-lowering medications and having low-density lipoprotein [0] cholesterol <70 mg/dL or non-HDL cholesterol <100 mg/dL), higher-quality diet (y/n; defined as consuming a diet with aHEI-2010 score in the highest quartile [≥51.5; score range, 0-100]), high–saturated fat diet (y/n; defined as percent of energy consumed from saturated fat in the highest quartile [≥ 13.8%]), and low–saturated fat diet (y/n; defined as percent of energy consumed from saturated fat <7%). The joint test was used to obtain a Pvalue for interaction for examining statistical significance of the difference between subgroups.32
An absolute risk difference (ARD) was calculated for each hazard ratio (HR) derived from the previously described models. Specifically, we used the mean of the included covariates and calculated the difference in absolute risk at the maximum follow-up time given each additional 300 mg dietary cholesterol consumed per day or 0.5 egg consumed per day. Three R packages were used: riskRegression,33 survival,34 and pec.35 The bootstrap method was applied to derive 95% CIs for ARD based on 100 bootstrap samples.
Six sensitivity analyses were conducted for primary outcomes: (1) events ascertained during the first 2 and 5 years of follow-up were excluded; (2) participants were arbitrarily censored at 10- and 20-year follow-up; (3) multiple imputation by chained equations was applied to impute missing data for study variables36 and events were censored at loss to follow-up; (4) any 1 of the 6 cohorts was dropped out of the analyses; (5) cohort-specific quintiles or convenient categorical cutoffs for dietary cholesterol or egg consumption were used; and (6) subdistribution hazard models were used instead of cause-specific hazard models.24,25 A 2-tailed P value of less than .05 was used to determine the statistical significance. Because of the potential for type I error due to multiple comparisons, findings for analyses of secondary outcomes should be interpreted as exploratory. All analyses were performed using SAS version 9.4 and R version 3.5.2.
This study included 29 615 participants with 524 376 person-years of follow-up data (Table).
Mean (SD) age was 51.6 (13.5) years at baseline, 9204 (31.1%) were black, 13 299 (44.9%) were men. The 6 cohorts differed considerably in terms of sample size, age, sex, race/ethnicity, education level, BMI, and behavioral and clinical CVD risk factors, as well as incident CVD and all-cause mortality rates. Overall median dietary cholesterol consumption was 241 mg per day (interquartile range [IQR], 164-350) and the overall mean (SD) was 285 (184) mg per day. Overall median egg consumption was 0.14 per day (IQR, 0.07-0.43) and the overall mean (SD) was 0.34 (0.46) per day. Participants’ characteristics, according to 5 levels of dietary cholesterol or egg consumption are shown in eTables 1 and 2 in the Supplement. The unadjusted incidence per 1000 person-years was 10.9 (95% CI, 10.6-11.2) for incident CVD and 11.7 (95% CI, 11.4-12.0) for all-cause mortality (eTable3 in the Supplement). The energy-adjusted Pearson correlations between dietary cholesterol or egg consumption and a range of dietary factors are shown in eTable 4 in the Supplement.
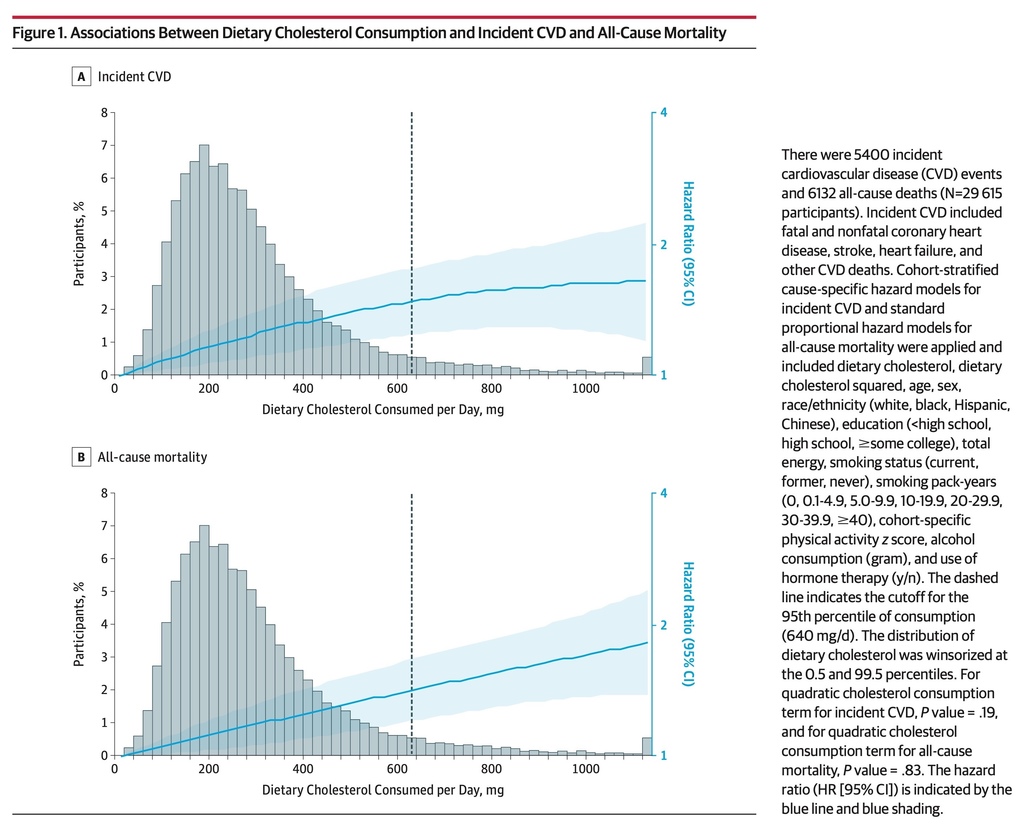
During a median follow-up of 17.5 years (IQR, 13.0-21.7; maximum 31.3), there were a total of 5400 incident CVD events (2088 fatal and nonfatal CHD events, 1302 fatal and nonfatal stroke events, 1897 fatal and nonfatal heart failure events, and 113 other CVD deaths) and 6132 all-cause deaths. The associations between dietary cholesterol consumption and incident CVD and all-cause mortality were monotonic (P value >.1 for quadratic cholesterol term; Figure 1).
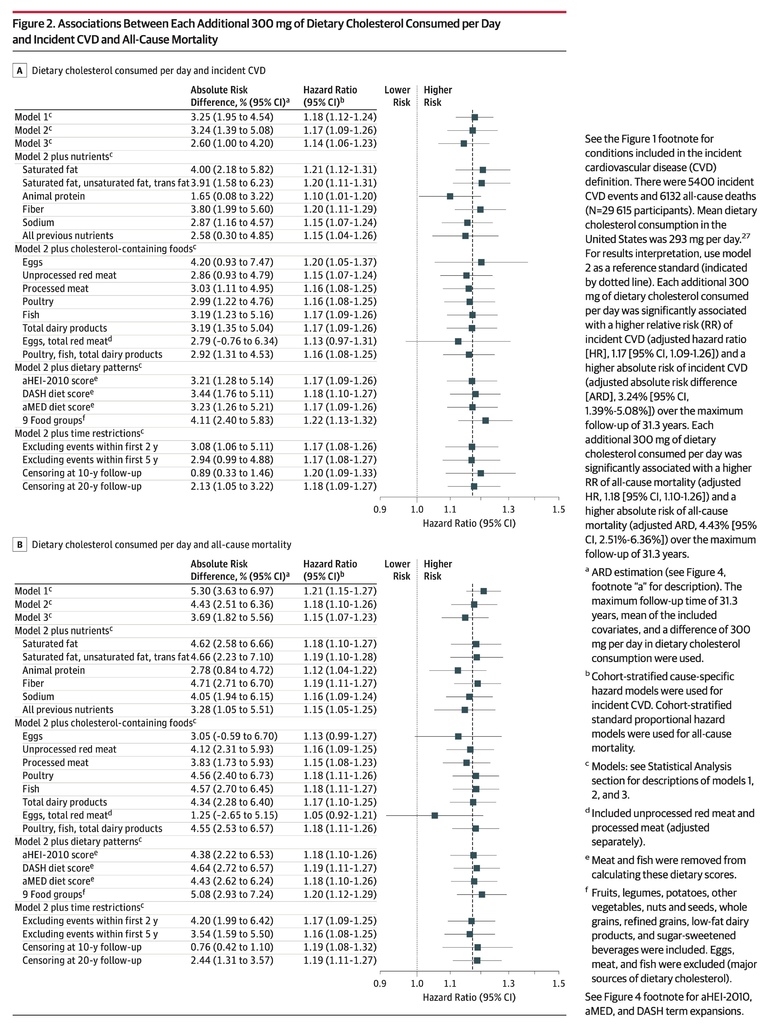
Based on model 2, each additional 300 mg of dietary cholesterol consumed per day was significantly associated with higher risk of incident CVD (adjusted HR, 1.17 [95% CI, 1.09-1.26]; adjusted ARD, 3.24% [95% CI, 1.39%-5.08%]; Figure 2A) and all-cause mortality (adjusted HR, 1.18 [95% CI, 1.10-1.26]; adjusted ARD, 4.43% [95% CI, 2.51%-6.36%]; Figure 2B).
These associations remained significant after further adjusting for CVD risk factors (eg, BMI, diabetes, blood pressure, and serum lipids), dietary fats, animal protein, fiber, sodium, cholesterol-containing foods, or dietary patterns with 2 exceptions: (1) the associations between dietary cholesterol consumption and incident CVD (adjusted HR, 1.13 [95% CI, 0.97-1.31]; adjusted ARD, 2.79% [95% CI, −0.76% to 6.34%]) and all-cause mortality (adjusted HR, 1.05 [95% CI, 0.92-1.21]; adjusted ARD, 1.25% [95% CI, −2.65% to 5.15%]) were no longer significant after adjusting for consumption of eggs, unprocessed red meat, and processed meat; and (2) the association between dietary cholesterol consumption and all-cause mortality was no longer significant after adjusting for egg consumption (adjusted HR, 1.13 [95% CI, 0.99-1.27]; adjusted ARD, 3.05% [95% CI, −0.59% to 6.70%]).
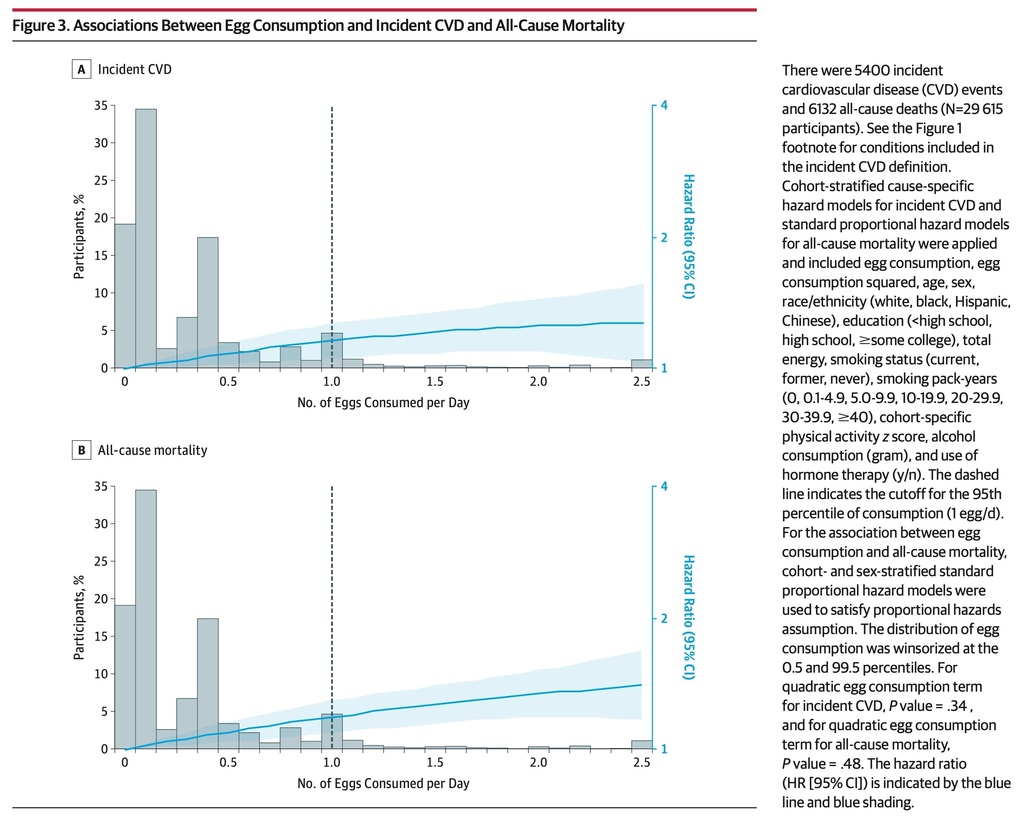
The associations between egg consumption and incident CVD and all-cause mortality were monotonic (P value > .3 for quadratic egg term; Figure 3).
Based on model 2, each additional half an egg consumed per day was significantly associated with higher risk of incident CVD (adjusted HR, 1.06 [95% CI, 1.03-1.10]; adjusted ARD, 1.11% [95% CI, 0.32%-1.89%]; Figure 4A) and all-cause mortality (adjusted HR, 1.08 [95% CI, 1.04-1.11]; adjusted ARD, 1.93% [95% CI, 1.10%-2.76%]; Figure 4B).
These associations remained significant after accounting for CVD risk factors, dietary fats, animal protein, fiber, sodium, or dietary patterns. However, the associations between egg consumption and incident CVD (adjusted HR, 0.99 [95% CI, 0.93-1.05]; adjusted ARD, −0.47% [95% CI, −1.83% to 0.88%]) and all-cause mortality (adjusted HR, 1.03 [95% CI, 0.97-1.09]; adjusted ARD, 0.71% [95% CI, −0.85% to 2.28%]) were no longer significant after adjusting for dietary cholesterol consumption.
The adjusted HRs (95% CIs), calculated using other increment units for dietary cholesterol or egg consumption based on model 2, are shown in eTable 5 and eTable 6 in the Supplement.
The association between dietary cholesterol consumption (per 300 mg/day) and incident CVD was stronger in participants with BMI lower than 25 (adjusted HR, 1.25 [95% CI, 1.12-1.39]) than in overweight participants (BMI ≥25 to <30; adjusted HR, 1.05 [95% CI, 0.95-1.16]) or obese participants (BMI ≥30; adjusted HR, 1.14 [95% CI, 1.03-1.26]) (P value for interaction, .03) (Figure 5) and stronger in participants without low lipid levels (adjusted HR, 1.19 [95% CI, 1.11-1.28]) than in participants with low lipid levels (adjusted HR, 0.96 [95% CI, 0.78-1.19]) (P value for interaction, .04).
The association between dietary cholesterol consumption and all-cause mortality was stronger in women (adjusted HR, 1.28 [95% CI, 1.17-1.41]) than in men (adjusted HR, 1.14 [95% CI, 1.06-1.22]) (P value for interaction, .02) (Figure 6) and stronger in participants who consumed a high–saturated fat diet (adjusted HR, 1.24 [95% CI, 1.13-1.36]) than in participants who did not (adjusted HR, 1.12 [95% CI, 1.04-1.21]) (P value for interaction, .046).
The association between egg consumption (per half an egg/day) and incident CVD was stronger in women (adjusted HR, 1.13 [95% CI, 1.07-1.20]) than in men (adjusted HR, 1.03 [95% CI, 0.99-1.08]) (P value for interaction, .009; Figure 7) and stronger in participants without low lipid levels (adjusted HR, 1.07 [95% CI, 1.04-1.11]) than in participants with low lipid levels (adjusted HR, 0.93 [95% CI, 0.81-1.07]) (P value for interaction, .04).
The association between egg consumption and all-cause mortality was stronger in women (adjusted HR, 1.16 [95% CI, 1.10-1.23]) than in men (adjusted HR, 1.04 [95% CI, 1.01-1.08]) (P value for interaction, .001) (Figure 8) and stronger in participants without low lipid levels (adjusted HR, 1.09 [95% CI, 1.05-1.12] than in participants with low lipid levels (adjusted HR, 0.95 [95% CI, 0.86-1.05]) (P value for interaction, .007).
The associations of dietary cholesterol or egg consumption with CVD subtypes and cause-specific mortality were monotonic (P value for quadratic terms >0.1).
Dietary cholesterol (per 300 mg/day; adjusted HR, 1.10 [95% CI, 0.98-1.23]) or egg consumption (per half an egg/day; adjusted HR, 1.05 [95% CI, 0.99-1.11]) was not significantly associated with CHD in model 2 (eFigure 1 and eFigure 6 in the Supplement). Dietary cholesterol consumption was significantly associated with stroke (adjusted HR, 1.26 [95% CI, 1.09-1.46]; eFigure 2 in the Supplement). This association was no longer significant after adjusting for egg consumption alone (adjusted HR, 1.19 [95% CI, 0.91-1.57]) or consumption of eggs, unprocessed red meat, and processed meat together (adjusted HR, 1.02 [95% CI, 0.75-1.38]). Dietary cholesterol consumption was significantly associated with heart failure (adjusted HR, 1.14 [95% CI, 1.05-1.24]; eFigure 3 in the Supplement). This association was no longer significant after adjusting for CVD risk factors (adjusted HR, 1.11 [95% CI, 0.98-1.27]) or animal protein consumption (adjusted HR, 1.06 [95% CI, 0.91-1.23]). Egg consumption was significantly associated with stroke (adjusted HR, 1.11 [95% CI, 1.03-1.18]; eFigure 7 in the Supplement), but not heart failure (adjusted HR, 1.06 [95% CI, 0.996-1.12]; eFigure 8 in the Supplement). The association between egg consumption and stroke was no longer significant after adjusting for dietary cholesterol consumption (adjusted HR, 1.03 [95% CI, 0.91-1.17]).
Dietary cholesterol consumption was significantly associated with CVD mortality (adjusted HR, 1.22 [95% CI, 1.07-1.39]; eFigure 4 in the Supplement). This association was no longer significant after adjusting for animal protein consumption (adjusted HR, 1.07 [95% CI, 0.91-1.25]), egg consumption (adjusted HR, 1.23 [95% CI, 0.95-1.59]), or consumption of eggs, unprocessed red meat, and processed meat (adjusted HR, 1.13 [95% CI, 0.85-1.50]). Dietary cholesterol consumption was significantly associated with non-CVD mortality (adjusted HR, 1.16 [95% CI, 1.08-1.26]; eFigure 5 in the Supplement). This association was no longer significant after adjusting for egg consumption (adjusted HR, 1.10 [95% CI, 0.95-1.26]) or consumption of eggs, unprocessed red meat, and processed meat (adjusted HR, 1.03 [95% CI, 0.88-1.21]). Egg consumption was significantly associated with CVD mortality (adjusted HR, 1.08 [95% CI, 1.01-1.15]; eFigure 9 in the Supplement) and non-CVD mortality (adjusted HR, 1.08 [95% CI, 1.04-1.11]; eFigure 10 in the Supplement), but these associations were no longer significant after adjusting for dietary cholesterol consumption for CVD mortality (adjusted HR, 0.99 [95% CI, 0.88-1.12]) and non-CVD mortality (adjusted HR, 1.04 [95% CI, 0.97-1.11]), as well as adjusting for animal protein consumption for CVD mortality (adjusted HR, 1.05 [95% CI, 0.99-1.12])
Excluding events within the first 2 and 5 years or censoring participants at 10- and 20-year follow-up did not materially alter the significant associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality (Figure 2; Figure 4). Compared with the included participants (N = 29 615), participants who were excluded (n = 4882) were older (54.4 vs 51.6 years), more likely to be black (42.5% vs 31.1%), and less likely to have an education of some college or more (43.6% vs 54.7%) (eTable 7 in the Supplement). The adjusted HRs (95% CIs) were similar between complete case analyses and multiple imputation-based analyses (eTable 8 in the Supplement). Dropping any 1 of the 6 cohorts did not considerably alter the significant associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality (eTable 9 in the Supplement). These significant associations were similar when the exposure variables were divided into quintiles or by other convenient cutoffs (eTables 10-13 in the Supplement). The adjusted HRs (95% CIs) obtained from subdistribution hazard models were similar to those obtained from cause-specific hazard models (eTable 14 in the Supplement).
Among 29 615 adults pooled from 6 prospective cohort studies in the United States with a median follow-up of 17.5 years, higher consumption of dietary cholesterol or eggs was significantly associated with higher risk of incident CVD and all-cause mortality, in a dose-response manner.
A recent meta-analysis did not report a conclusive association between dietary cholesterol consumption and CVD, primarily due to the heterogeneity of the available studies and sparse data.1 As a major source of dietary cholesterol, egg consumption has been differentially associated with CHD, stroke, heart failure, and mortality. Recent meta-analyses showed that frequent egg consumption (generally ≥1 per day), as compared with infrequent consumption (generally <1 per week or never), was associated with significantly higher risk of heart failure,10 significantly lower risk of stroke,6,8 or no significant association with stroke or stroke mortality,5,7 and higher risk of all-cause mortality (pooled HR 1.09, 95% CI [0.997-1.20]).8 No significant association with CHD was reported.5-8 Another meta-analysis, which analyzed all CVD subtypes together, reported a significant positive dose-response association between egg consumption and CVD.9 As highlighted by these meta-analyses,1,5-10 residual confounding was a potential reason for inconsistent results. For example, egg consumption was commonly correlated with unhealthy behaviors such as low physical activity, current smoking, and unhealthy dietary patterns.38 Also, cholesterol-containing foods are usually rich in saturated fat and animal protein.2 Failure to consider these factors and others could lead to differential conclusions. In contrast, the current study included comprehensive assessment of these factors. Also, the current study had longer follow-up than the majority of the previous studies and may have provided more power to detect associations.1,5-10
The current study found that the significant associations of dietary cholesterol consumption with incident CVD and all-cause mortality were independent of fat amount and quality of the diet. These findings are consistent with the evidence that a reduction of dietary cholesterol intake, in addition to isocaloric replacement of saturated fat by unsaturated fat, was significantly associated with reduced total cholesterol (primarily LDL cholesterol) concentration.39 Further, the significant association between egg consumption and incident CVD was fully accounted for by the cholesterol content in eggs, which also largely explained the significant association between egg consumption and all-cause mortality, offering additional support for the significant associations of dietary cholesterol consumption with incident CVD and all-cause mortality. Although the significant associations of dietary cholesterol consumption with incident CVD and all-cause mortality were no longer significant after accounting for egg, unprocessed red meat, and processed meat consumption, it remains unclear if cholesterol from these foods is more harmful than other cholesterol-containing foods. Statistically, the remaining variation in dietary cholesterol consumption from other foods may not be sufficient to materially modify the associations. Egg consumption contributed 25% to the total dietary cholesterol consumption and meat consumption contributed 42%.27 Mechanistically, eggs and processed or unprocessed red meat are rich in other nutrients such as choline, iron, carnitine, and added sodium (for processed meat) that have been implicated in CVD risk via different pathways. Further, the significant associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality were similar between participants who consumed a higher-quality diet and those who did not, suggesting that people may need to minimize dietary cholesterol and egg yolk intake when consuming a healthier eating pattern, as recommended by the Institute of Medicine.40
The magnitudes of the significant associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality were modest but consistent across event subtypes including stroke, heart failure (except for egg consumption: adjusted HR 1.06, 95% CI [0.996-1.12]), CVD mortality, and non-CVD mortality, as well as for subgroups according to age, race/ethnicity, smoking status, CVD risk factors (ie, diabetes, hypertension, and hyperlipidemia), and diet quality. The nonsignificant association for CHD was consistent with the literature.5-8 US mean dietary cholesterol consumption of approximately 290 mg per day is higher than the global average of 228 mg per day,41 and was relatively stable from 2001-2002 to 2013-2014.27 Egg consumption has been relatively low in the United States, but overall per capita egg consumption increased by 11% from 23.0 g per day in 2001-2002 to 25.5 g per day in 2011-2012.28 The recommendations for dietary cholesterol and egg consumption from the 2015-2020 Dietary Guidelines, if carried forward in subsequent versions of Dietary Guidelines, might lead to further increases in egg and dietary cholesterol consumption in the United States, which could be harmful for prevention of CVD and premature death. Findings of the current study suggest that cholesterol from egg yolk may be harmful in the context of the current US diet, in which overnutrition and overweight/obesity are more common than malnutrition and underweight. This is consistent with the evidence that frequent egg consumption has been significantly associated with diabetes risk only in US studies.42
This study has several limitations. First, appropriate interpretation of the study findings requires consideration of measurement error for self-reported diet data. Further, this study relied on single measurement of egg and dietary cholesterol consumption. Exposure misclassification may be of concern, but results were similar when censoring participants at different time points. Second, all cohorts used different dietary assessment tools except 2 Framingham cohorts, which created heterogeneities for data analyses. This was addressed by the following: (1) implementing a rigorous methodology to harmonize diet data; (2) performing cohort-stratified analyses; and (3) conducting several sensitivity analyses. Third, residual confounding was likely, although a number of covariates were adjusted. Fourth, data were not available for investigating subtypes of CHD, stroke, and heart failure, as well as more detailed cause-specific mortality such as cancer mortality. Fifth, generalizing our results to non-US populations requires caution due to different nutrition and food environments and chronic disease epidemiology. Sixth, the study findings are observational and cannot establish causality.
Among US adults, higher consumption of dietary cholesterol or eggs was significantly associated with higher risk of incident CVD and all-cause mortality in a dose-response manner. These results should be considered in the development of dietary guidelines and updates.












 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 