[Excerpts]
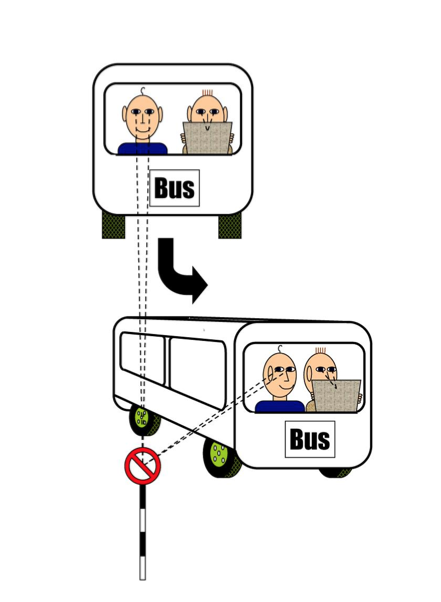
Visual-vestibular conflict. As the bus turns, the passenger on the left has a fixed external visual reference and has no visual-vestibular conflict. The passenger on the right, who is reading the paper, experiences a conflict because the visual input is still but the vestibular system is sensing motion (modified from Bronstein and Lempert)
Summary points
- Motion sickness is a common and potentially disabling problem, thought to be due to sensory conflict or "mismatch" involving the vestibular system
- Management using behavioural methods such as habituation can be effective and has few adverse effects, but can be unpleasant and time consuming
- Hyoscine is an effective preventive medication for which oral preparations and transdermal patches are established in clinical practice, and emerging evidence suggests that hyoscine nasal spray is effective in preventing motion sickness
- Evidence to support the use of other drugs, taking into account the trade off between efficacy and adverse effects, is weaker.
- Management of motion sickness with traditional remedies such as ginger and acupressure bands has not been shown to be effective.
- Motion sickness is a syndrome of nausea and vomiting, pallor, sweating, headache, dizziness, malaise, increased salivation, apathy, drowsiness, belching, hyperventilation, and stomach awareness. Symptoms can be provoked by externally imposed motion, or implied self motion from a moving visual field, such as in a cinema. The condition has been recognised from the early days of sea travel and the word for sickness, "nausea," derives from the Greek word nu alpha nu sigmaf, meaning "ship."
- Travel by car, train, or other transport is part of everyday life for most people, and motion sickness is a common problem. Estimating its prevalence is complex because reported symptoms depend on variables such as previous avoidance and exposure, as well as presumed inherent susceptibility. Some estimates are presented in table 1. Motion sickness may have an important effect on occupational activity for some people, such as airline pilots, those in the armed forces, and emergency services staff. General practitioners may frequently encounter patients who report difficulties in work or daily life related to motion sickness, or those seeking advice about prevention before a forthcoming journey. We review the management of patients with motion sickness for the generalist. This article is based on evidence obtained largely from controlled studies in patients and in healthy volunteers.
HOW CAN MOTION SICKNESS BE TREATED?
BEHAVIOURAL COUNTER MEASURES
Simple behavioural counter measures can be effective treatments for patients who experience motion sickness. A within person comparison showed that sickness was reduced when a stable visual reference point, such as the horizon, was provided, minimising visual-vestibular conflict during sea travel. Forward visibility is particularly helpful in coach or bus travel. Alternatively, laboratory based observations showed that lying supine, where practical, reduces symptoms of motion sickness and is preferable to an upright seated posture. Controlled studies have shown that deliberate restriction of head movements is helpful, as is avoidance of tasks that enhance visual-vestibular conflict, such as reading when travelling.
Prospective controlled studies have shown that repeated exposure to the nauseogenic stimulus (habituation) is an effective treatment for motion sickness. Habituation programmes pioneered by the military are effective but time consuming. For maximum efficacy, the exposure to the stimuli needs to be frequent and graded. The exposure is initially gentle, and is then increased by gradual increments to maximise acceptability and speed up recovery between sessions, and to avoid the undesirable effect of sensitisation to the stimulus. Habituation is specific to a particular stimulus: tolerance to car travel may have no effect on susceptibility to seasickness.
A prospective controlled study of healthy volunteers has shown that coping strategies such as controlled regular breathing or listening to music are more effective than placebo in reducing nausea. However the effect size was small, with provocative stimuli tolerated for around 10% longer. A small but well designed prospective placebo controlled study showed no benefit of acupressure bands over control, although a small trial showed Korean hand pressure to be more effective than sham pressure in reducing subjective nausea for emergency patients transported in ambulances.
Motion sickness is increasingly reported in the context of virtual environments, with head mounted or large field of view displays, when it is known as cybersickness or visually induced motion sickness. These devices are potentially useful tools for various research, health, training, and leisure activities. Cybersickness can be treated with habituation.
ANTIEMETIC DRUGS
Most drugs in common use for motion sickness have been used for more than 30 years. Some of these drugs have been examined in small but well designed studies. However, most data have been obtained in studies involving healthy adults, usually men. Data on the effectiveness of these drugs for treating motion sickness in women and children are scarce, although these groups are generally more susceptible than men. Many of the drugs cause drowsiness and other adverse effects. Also, evidence suggests that some (for example, hyoscine) may delay habituation either directly or indirectly via sedative effects. Consider drug treatment carefully in patients who could benefit from using habituation methods to overcome motion sickness, and discuss this disadvantage of using drugs with them before embarking on treatment. Some drugs in common use are shown in table 2.
Common anti-motion sickness drugs (adapted from Benson, 2002)
========================
DRUG: Hyoscine OTC
ROUTE: Oral
ADULT DOSE: 0.3-0.6 mg
TIME TO ONSET:30 min
DURATION OF ACTION (H):4
-------------------------------
DRUG: Hyoscine
ROUTE: Injection
ADULT DOSE: 0.1-0.2 mg
TIME TO ONSET:15 min
DURATION OF ACTION (H):4
-------------------------------
DRUG:Hyoscine
ROUTE: Transdermal patch
ADULT DOSE:
TIME TO ONSET: 6–8 h
DURATION OF ACTION (H): 72
-------------------------------
DRUG: Promethazine OTC
ROUTE: Oral
ADULT DOSE: 25-50 mg
TIME TO ONSET: 2 h
DURATION OF ACTION (H): 15
-------------------------------
DRUG: Promethazine
ROUTE: Injection
ADULT DOSE: 25 mg
TIME TO ONSET: 15 min
DURATION OF ACTION (H): 15
-------------------------------
DRUG: Promethazine
ROUTE: Suppository
ADULT DOSE: 25 mg
TIME TO ONSET: 1 h
DURATION OF ACTION (H): 15
-------------------------------
DRUG: Dimenhydrinate
ROUTE: Oral
ADULT DOSE: 50-100 mg
TIME TO ONSET: 2 h
DURATION OF ACTION (H): 8
-------------------------------
DRUG: Dimenhydrinate
ROUTE: Injection
ADULT DOSE: 50 mg
TIME TO ONSET: 15 min
DURATION OF ACTION (H): 8
-------------------------------
DRUG: Cyclizine
ROUTE:Oral
ADULT DOSE: 50 mg
TIME TO ONSET:2 h
DURATION OF ACTION (H): 6
-------------------------------
DRUG: Cyclizine
ROUTE:Injection
ADULT DOSE: 50 mg
TIME TO ONSET:15 min
DURATION OF ACTION (H): 6
-------------------------------
DRUG:Meclizine
ROUTE: Oral
ADULT DOSE: 25-50 mg
TIME TO ONSET: 2 h
DURATION OF ACTION (H): 8
-------------------------------
DRUG: Buclizine
ROUTE: Oral
ADULT DOSE: 50 mg
TIME TO ONSET: 1 h
DURATION OF ACTION (H): 6
-------------------------------
DRUG: Cinnarizine OTC
ROUTE: Oral
ADULT DOSE: 15-30 mg
TIME TO ONSET: 4 h
DURATION OF ACTION (H): 8
========================
OTC=over the counter
Gastric stasis occurs with motion sickness before the vomiting phase, so non-oral routes of administration, such as transdermal patches, are advantageous. Medication is most effective when taken before exposure rather than after the onset of symptoms. Drugs are useful in situations where habituation is impractical, such as solitary or infrequent journeys.
Antimuscarinics
Hyoscine (scopolamine) is available as tablets or liquid for oral ingestion, intravenous and subcutaneous injection, and transdermal patches. Its potential adverse effects include drowsiness, blurred vision, dry mouth, and dizziness, which reflect its muscarinic anticholinergic properties. However, many studies have reported that it is safe and well tolerated.
Patches are applied to the mastoid area 6-8 hours before exposure. Patch users should wash their hands thoroughly both before and after touching the patch, since hyoscine can be spread to the eyes by hand, which can cause blurred vision and pupil dilatation. Patches should never be cut into pieces, as this interferes with the drug release mechanism. One small randomised, crossover, double blind study in healthy young men reported on double dose hyoscine patch therapy as a potential treatment for those in whom a single patch is ineffective, and concluded that two patches were safe and well tolerated in this group. Faster onset of action may be obtained through administration as a nasal spray. A small randomised, placebo controlled, double blind crossover trial using experimentally induced motion sickness in young adults showed the nasal preparation to be effective, with no significant decrease in alertness. A Cochrane systematic review concluded that hyoscine is more effective
than placebo in treating the symptoms of motion sickness, but that its effectiveness compared with other treatments for the condition is unclear. Selective M3 or M5 muscarinic receptor antagonists may also be effective against motion sickness.
Antihistamines
Antihistamines-including cinnarizine, meclozine, dimenhydrinate, cyclizine, chlorphenamine, and promethazine-are the other main group of drugs frequently used to treat motion sickness. These are available as prescribed and over the counter preparations. Cinnarizine at a dose of 50 mg was more effective than placebo at reducing symptoms in a double blind placebo controlled study, although 25 mg was not. According to a small placebo controlled study of healthy young men, promethazine is effective given as a 50 mg intramuscular injection, but at the cost of considerable sedative effects. Dimenhydrinate was found to be no more effective than placebo in another study of susceptible individuals. Cetirizine and fexofenadine are ineffective, probably owing to a lack of central nervous system effects.
Central nervous system stimulants
Sympathomimetics such as dextroamphetamine have been documented to have efficacy in the prevention of motion sickness, either alone or in combination with other drugs, but their usefulness is limited by the potential for abuse and legal problems. Amphetamine has been discontinued as an anti-motion sickness treatment, apart from some limited use in special circumstances for the military. Modafinil, an alternative central nervous system stimulant, was recently evaluated as a potential treatment for motion sickness, but was not found to be effective alone in a double blind, placebo controlled study.
Ondansetron
Individuals with a history of motion sickness are at higher risk for postoperative and chemotherapy induced nausea and vomiting. Because 5-HT3 receptor antagonists such as ondansetron have revolutionised the management of nausea and vomiting, experts hoped they would be efficacious in the management of motion sickness. However, initial results of placebo controlled studies have not shown ondansetron to be effective among small groups of healthy volunteers or larger groups of people with a history of high susceptibility to motion sickness.
NON DRUG REMEDIES
Ginger is a popular traditional remedy for nausea. One small trial suggested that ginger was better than placebo in treating motion sickness but another has shown it to be ineffective compared with hyoscine. Supplemental oxygen may reduce motion sickness in patients being transported by ambulance, but does not alleviate the problem in individuals who are otherwise healthy. This apparent paradox is perhaps explained by the suggestion that supplemental oxygen may work by ameliorating internal states that sensitise for motion sickness.
COMBINATION TREATMENTS
Combinations of agents have also been selected with the aim of increasing efficacy and others to increase tolerability. One small study examined the combination of chlorpheniramine with ephedrine to combat the drowsiness which is so frequently a problem in managing motion sickness. A modest reduction in drowsiness was reported. In another study of the prevention of air sickness, the combination of promethazine with caffeine was more effective than placebo, meclizine, or hyoscine and had fewer adverse effects. Although no longer available for legal reasons, combinations of hyoscine or promethazine with amphetamine are highly effective.
OTHER DRUGS
5-HT receptor agonists
Given the well known connections between migraine and motion sickness, and the revolution in migraine management that has taken place thanks to the advent of 5-HT 1B/1D receptor agonists (triptans), experts hoped that these drugs might be useful in motion sickness, both in migraineurs and in non-migraineurs. Rizatriptan has been evaluated for efficacy in motion sickness in migraineurs in a double blind randomised placebo controlled study. Although the majority of participants with complete data reported a reduction in symptoms, the effect was small and not repeatable.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 