Self-management of hypertension is effective, but most studies have included few patients at high risk for cardiovascular (CV) disease. This primary care U.K. study involved 555 hypertensive patients (blood pressure [BP], >130/80 mm Hg) who had diabetes, coronary disease, cerebrovascular disease, or kidney disease (glomerular filtration rate, 30–59 mL/minute/1.73 m2). Patients with dementia, postural hypotension, or terminal illnesses and those who took >3 antihypertensive medications or were pregnant were excluded.
Patients were randomized to a self-management and self-monitoring protocol or to usual care. Intervention patients were trained during two or three sessions to take their BPs and to follow a predetermined plan in making decisions in response to various readings. For example:
- A patient with any reading of >181 mm Hg systolic or >101 mm Hg diastolic was prompted to make an appointment with a study physician or nurse within 48 hours.
- A patient who recorded >4 readings in a single week of 121 to 180 mm Hg systolic or 76 to 100 diastolic in 2 consecutive months was referred to an algorithm for medication changes that had been negotiated previously with his or her primary care physician.
At baseline, mean BP was 143/80 mm Hg. Target BP was 120/70 mm Hg. At 12 months, intervention patients' mean BP was significantly lower than that of usual-care patients (128/74 vs. 139/76 mm Hg). Researchers noted no differences in adverse events between the groups.
COMMENT
Self-monitoring and self-management of hypertension is done commonly in some Western countries but not in the U.S. Many barriers arise from clinical caution, healthcare system dysfunction, and inadequate reimbursement (to both patients and clinicians); however, this study shows that, in the right system and with the proper training and follow-up, a supervised home-based program of hypertension management can effectively lower BP, even in high-risk patients. However, the clinically important objective of this strategy — lower morbidity and mortality — remains to be demonstrated.
JAMA. 2014;312(8):799-808. doi:10.1001/jama.2014.10057.
Abstract
IMPORTANCE:
Self-monitoring of blood pressure with self-titration of antihypertensives (self-management) results in lower blood pressure in patients with hypertension, but there are no data about patients in high-risk groups.
OBJECTIVE:
To determine the effect of self-monitoring with self-titration of antihypertensive medication compared with usual care on systolic blood pressure among patients with cardiovascular disease, diabetes, or chronic kidney disease.
DESIGN, SETTING, AND PATIENTS:
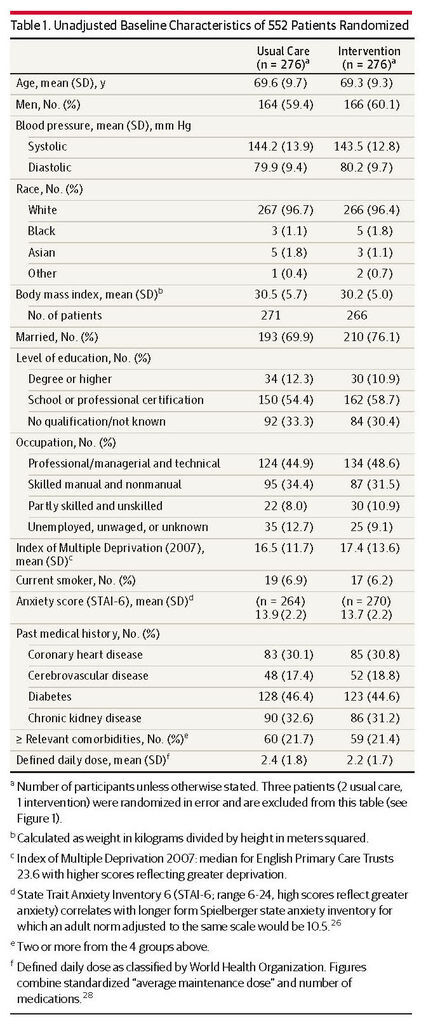
A primary care, unblinded, randomized clinical trial involving 552 patients who were aged at least 35 years with a history of stroke, coronary heart disease, diabetes, or chronic kidney disease and with baseline blood pressure of at least 130/80 mm Hg being treated at 59 UK primary care practices was conducted between March 2011 and January 2013.
INTERVENTIONS:
Self-monitoring of blood pressure combined with an individualized self-titration algorithm. During the study period, the office visit blood pressure measurement target was 130/80 mm Hg and the home measurement target was 120/75 mm Hg. Control patients received usual care consisting of seeing their health care clinician for routine blood pressure measurement and adjustment of medication if necessary.
MAIN OUTCOMES AND MEASURES:
The primary outcome was the difference in systolic blood pressure between intervention and control groups at the 12-month office visit.
RESULTS:
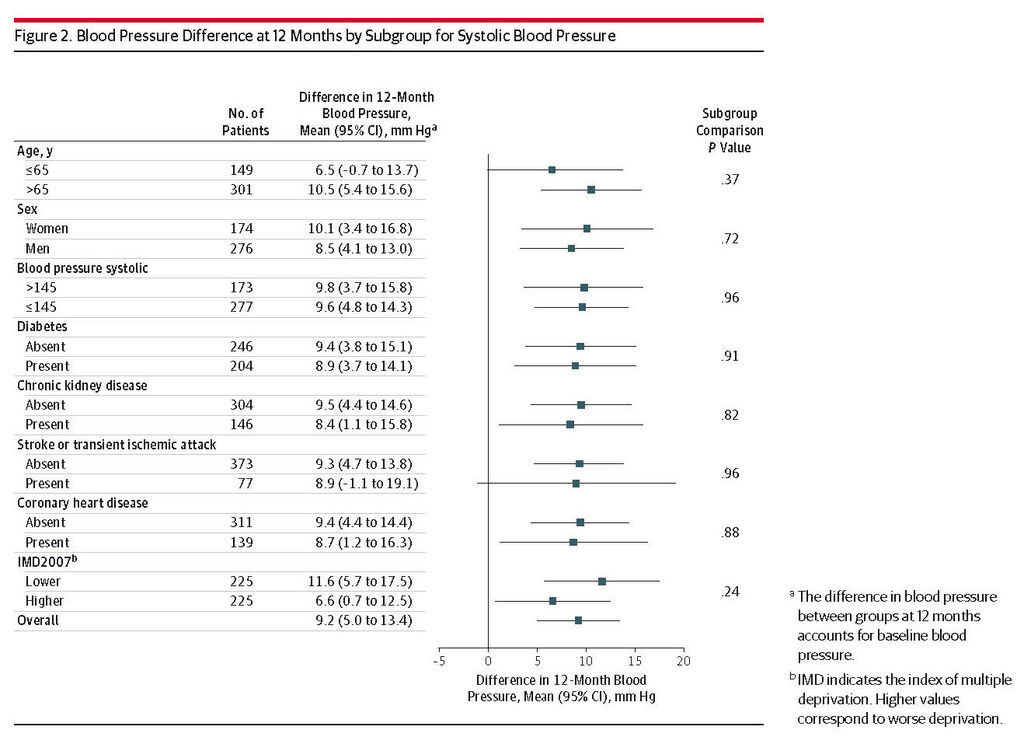
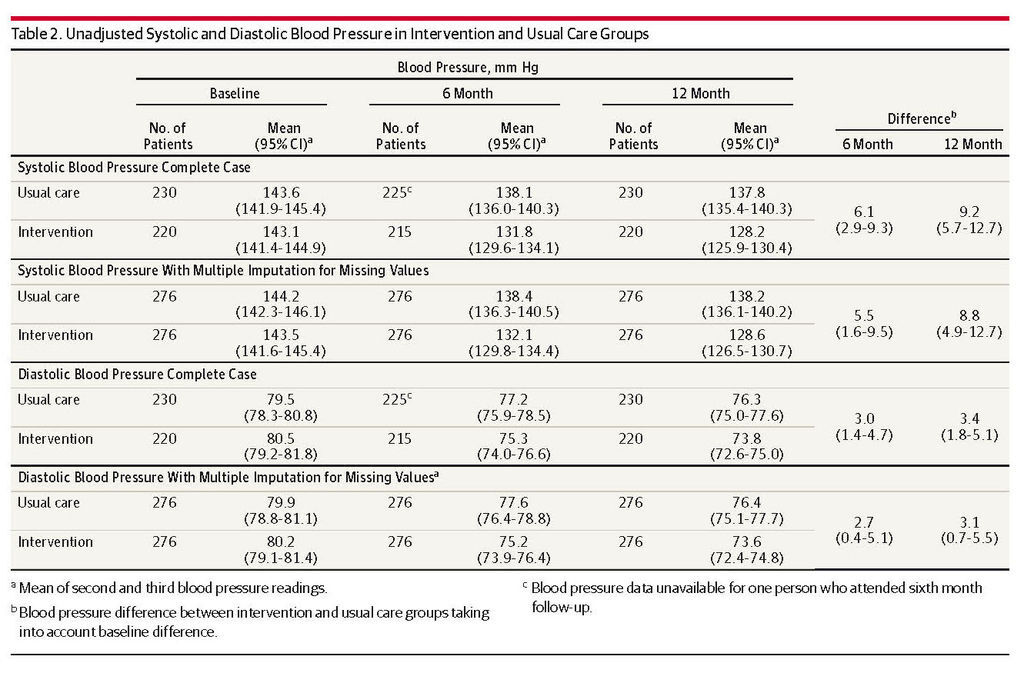
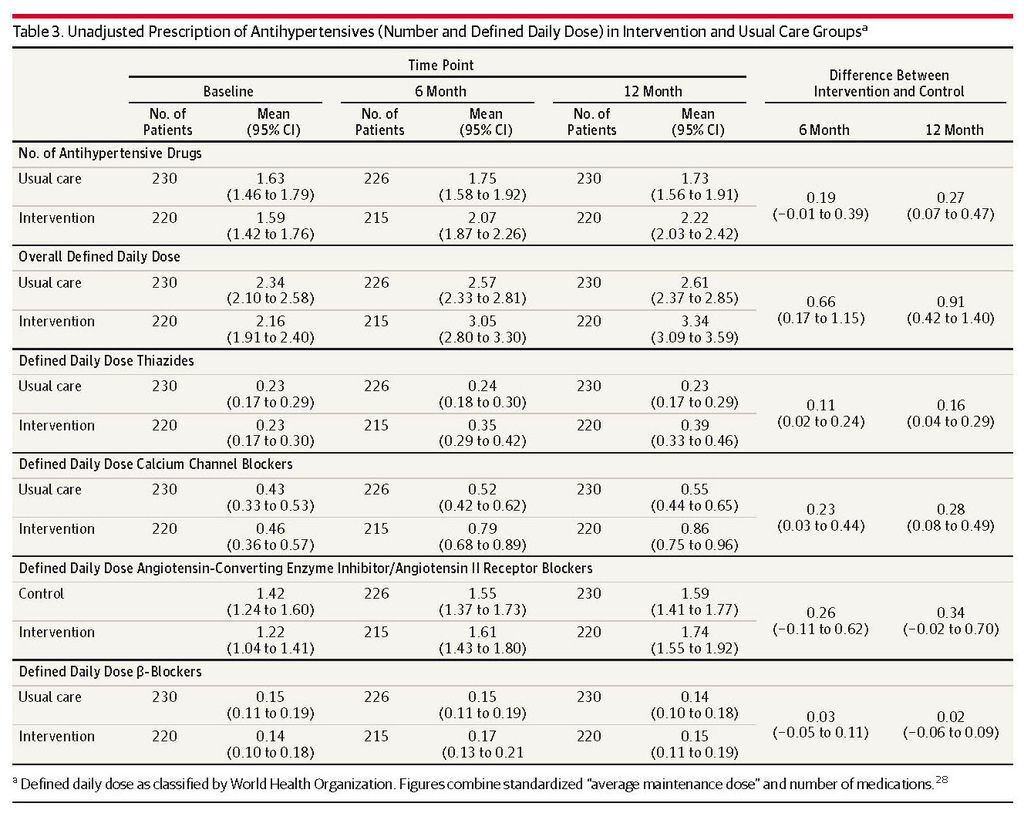
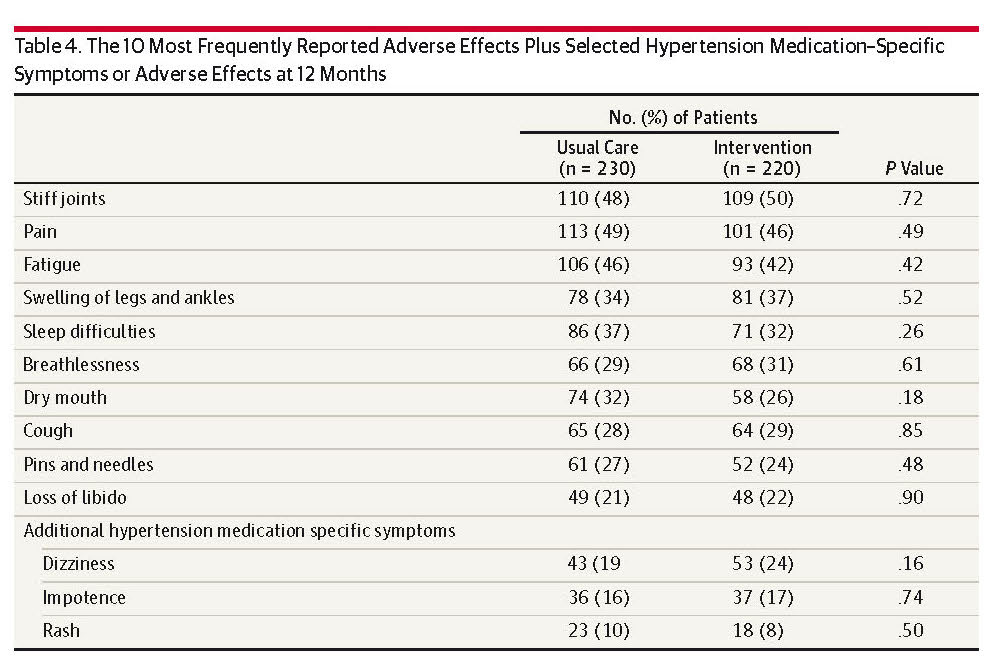
Primary outcome data were available from 450 patients (81%). The mean baseline blood pressure was 143.1/80.5 mm Hg in the intervention group and 143.6/79.5 mm Hg in the control group. After 12 months, the mean blood pressure had decreased to 128.2/73.8 mm Hg in the intervention group and to 137.8/76.3 mm Hg in the control group, a difference of 9.2 mm Hg (95% CI, 5.7-12.7) in systolic and 3.4 mm Hg (95% CI, 1.8-5.0) in diastolic blood pressure following correction for baseline blood pressure. Multiple imputation for missing values gave similar results: the mean baseline was 143.5/80.2 mm Hg in the intervention group vs 144.2/79.9 mm Hg in the control group, and at 12 months, the mean was 128.6/73.6 mm Hg in the intervention group vs 138.2/76.4 mm Hg in the control group, with a difference of 8.8 mm Hg (95% CI, 4.9-12.7) for systolic and 3.1 mm Hg (95% CI, 0.7-5.5) for diastolic blood pressure between groups. These results were comparable in all subgroups, without excessive adverse events.
CONCLUSIONS AND RELEVANCE:
Among patients with hypertension at high risk of cardiovascular disease, self-monitoring with self-titration of antihypertensive medication compared with usual care resulted in lower systolic blood pressure at 12 months.







 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 