學妹今天問我說他不太瞭解Thiazide用在尿崩症的機轉。
首先,要先瞭解何謂尿崩症:
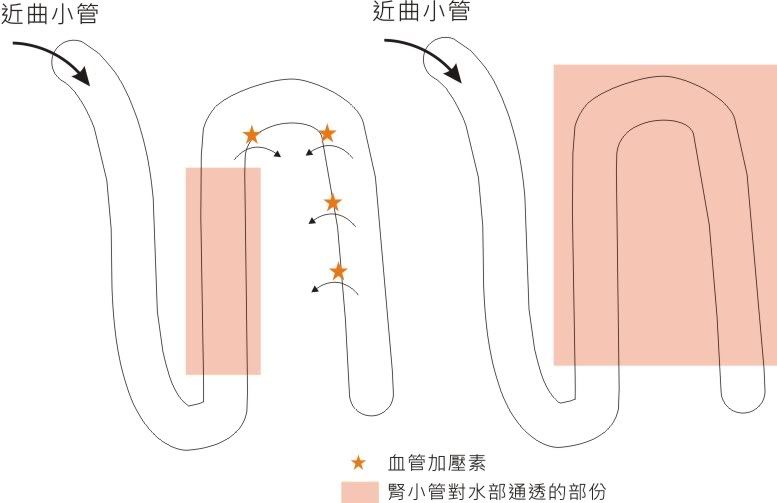
尿崩症(diabetes insipindus)是指血管加壓素(vasopressin,VP)又稱抗利尿激素(antidiuretic hormone,ADH) 分泌不足(又稱中樞性或垂體性尿崩症),或腎臟對血管加壓素反應缺陷(又稱腎性尿崩症)而引起的一症候群群,其特點是多尿、煩渴、低比重尿和低滲透壓尿。
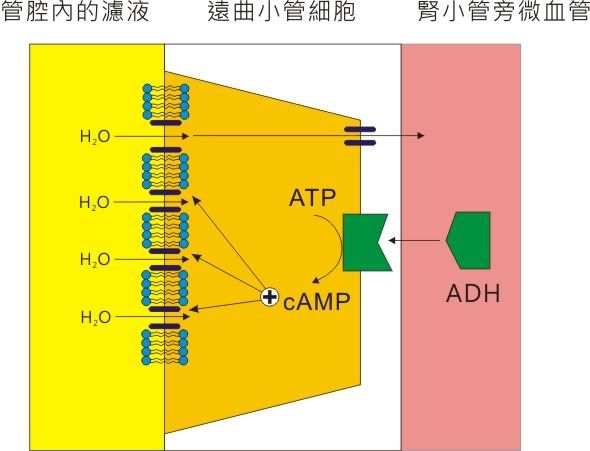
ADH的作用機轉是在遠曲小管內促使ATP轉換成cAMP,進而在膜上增加新的水通道使管腔膜對水的通透性增加。所以當血管加壓素消蝕或是無法和受體結合時,就會使管腔膜失去對水的通透性。
而對於腎性尿崩症來說:
腎性尿崩症的病因可由目前體內對水分平衡的生理調節去了解。血管加壓素(Arginine vasopressin(AVP)或稱抗利尿激素(ADH))是由下視丘的上視核及旁視核製造並且儲存於腦下垂體的後葉。AVP 的分泌最初是由血漿的滲透壓的改變來調節,但也可對於非滲透壓的刺激有所反應。這些非滲透壓的刺激一般不是跟全身血液體積的改變有關就是跟細胞外體液的分布有關。同時疼痛、情緒壓力、以及某些藥物(如尼古丁nicotine)也會影響AVP的分泌。
在腎臟方面,AVP與位於內髓質集尿細胞及拱廊細胞(arcade cell)表面的血管加壓素第二型受器 (又稱V2受器,vasopressin type-2(V2) receptors)結合 (拱廊是腎小管的一部份具高度分支且長的特性,其可連接許多深部及中皮層的腎元至皮質集尿管的源頭)。V2受器被結合的結果導致G蛋白產生而活化腺酸鹽環化酶 (adenlyate cyclase)而使細胞內ATP變成cAMP,cAMP經由一個大型的未知機轉,而其中一個機轉是活化蛋白激酶A(protein kinase A;PKA)以及磷酸化各種調控蛋白因而啟動細胞內包含許多水分子通道的小囊泡插入細胞膜的頂部;而使水分的滲透性大增,使水分可經由腎小管的內腔而滲透至較高張的髓質間隙。當AVP的刺激結束之後,水通道就會經由小囊泡的胞飲作用而自細胞膜的頂端移除。控制小囊泡由細胞膜頂端至細胞質的移動是藉由膜的來回穿梭機轉 (membrane shuttle mechanism)而成。
治療方式:腎性尿崩症被發現以來其治療方式就不是很確定。最重要的治療方式就是提供足量的液體補充尿液的流失量,第一類使用於腎性尿崩症患者相對較安全且在臨床上有效的藥物是thiazide類利尿劑。例如hydrocholrothiazide(HCTZ:2~4 mg/kg/24 hours)。當合併低鹽分的攝取時,可降低20~50%的尿量,這樣可以使某些病人的有足夠的體液維持恆定。
為何Thazide類利尿劑反而可以治療尿崩症?
先從Thiazide的機轉講起:
Thiazide主要作用在遠端腎小管前段,抑制Na+-Cl- co-transporter,阻斷Na+及Cl-的再吸收。同時又有類似碳酸苷酶抑制劑的效果,增加了K+及HCO3-的排泄。
看起來好像是利尿沒錯呀,但是對於尿崩為何有幫助呢?因為當腎臟的NaCl的再吸收被抑制時,腎的稀釋功能降低(即非滲透壓所吸引的水生成減少),導致血中的滲透壓增加,而減少血流量,進而加強ADH的作用來減少排尿量。
Thiazide透過排出增加導致血漿晶體滲透壓降低,結果口渴感減輕而病人就會減少喝水故尿量減少,故thiazide的抗尿崩症作用是在用藥兩天排除大量NaCl後開始出現的。
JASN有提到:Paradoxical Antidiuretic Effect of Thiazides in Diabetes Insipidus: Another Piece in the Puzzle
(doi: 10.1097/01.ASN.0000146568.82353.04 JASN November 1, 2004 vol. 15 no. 11 2948-2950 )
Thiazide diuretics inhibit the NaCl co-transporter (NCC/TSC) in the renal distal convoluted tubule (DCT) . The DCT is water impermeable and considered to be part of the diluting
segment. Therefore, the water-preserving effect of thiazides is unlikely related to a direct effect on the DCT. In fact, the most widely accepted hypothesis suggests that the antidiuretic action of thiazides is secondary to increased renal sodium excretion .
The renal sodium loss causes extracellular volume contraction leading to lowered GFR and increased proximal tubular sodium and water reabsorption. Hence, less water and solutes are delivered to the distal tubule and collect ing duct and are lost as urine.
至於那為何LOOP 沒有此效果 也有說明:
A loop diuretic, although also capable of inducing mild volume depletion, is not as likely to lower the urine output in nephrogenic DI. These agents decrease sodium chloride reabsorption in the medullary thick ascending limb of the loop of Henle, thereby decreasing the accumulation of NaCl in the medullary interstitium that is essential for the production of a concentrated urine. Thus, a loop diuretic induces relative ADH resistance, an effect that is counterproductive in nephrogenic DI.
另外,利用NSAID抑制PDE 來達到對水的通透性也是一種治療:
Nonsteroidal anti-inflammatory drugs — The efficacy of NSAIDs in this setting is dependent upon inhibition of renal prostaglandin synthesis. In normal subjects, prostaglandins antagonize the action of ADH and NSAIDs increase concentrating ability . If, for example, normal subjects are given a submaximal dose of ADH, the ensuing rise in urine osmolality can be increased by more than 200 mosmol/kg if the patient has been pretreated with a NSAID . The net effect in patients with DI may be a 25 to 50 percent reduction in urine output , a response that is partially additive to that of a thiazide diuretic .
This approach is particularly beneficial in patients with polyuria due to complex congenital polyuric-polydipsic Bartter-like syndromes, in whom prostaglandins appear to be pathogenetically important.
Not all NSAIDs are equally effective in a given patient; as an example, indomethacin appears to have a greater effect than ibuprofen. A variety of complications may ensue with long-term use of NSAIDs.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 