
Kiran Panesar, BPharmS (Hons), MRPharmS, RPh, CPh Consultant Pharmacist and Freelance Medical Writer Orlando, Florida
US Pharm. 2011;37(2):44-50.
Hypotension is a relative term that is used to describe a condition whereby an individual’s blood pressure (BP) is lower than the norm for that individual. Since there is no standard definition of hypotension, it is difficult to obtain accurate data on the frequency and incidence of this condition.1 In fact, in some patients, hypotension, or low blood pressure as it is commonly referred to, is normal, and patients with systolic pressures between 90 and 100 mmHg may even have a greater life expectancy than patients who are typically normotensive.2,3
While there is no need for concern in cases where BP is below 120/80 mmHg, patients who experience associated side effects such as dizziness, lightheadedness, and excessive thirst need to be further investigated (TABLE 1).4 These symptoms are a result of hypoperfusion of vital organs, which can lead to organ damage in the long term. In more serious cases, patients may faint, a condition known as syncope.4 In some patients, hypotension can be a debilitating disorder, confining them to bed.5 Furthermore, sudden drops in blood pressure can be life-threatening.6 A recent study conducted in Ireland concluded that postprandial hypotension (PPH) and orthostatic hypotension (OH) are among the most common cardiac disorders that cause falls and syncope.7
Mechanisms
Blood pressure is regulated by a number of mechanisms that are interconnected. According to the hydraulic equation, arterial BP is a product of the blood flow, indicated by cardiac output (CO) and pulmonary vascular resistance (PVR): BP = CO × PVR.8
These two factors provide moment-to-moment control of BP at three main anatomical sites: the arterioles, the postcapillary venules, and the heart. The kidney indirectly controls BP by maintaining the volume of intravascular fluid.8 Baroreceptor reflexes mediated by the autonomic nerves act in combination with humoral mechanisms to control the BP through these four sites. Furthermore, vasoactive substances from vascular endothelium, such as nitric oxide and endothelin-1, also regulate BP by altering vascular resistance.8
Pathophysiology
Hypotension can be caused by a change in either the CO or the PVR. This article discusses two types of hypotension—postprandial and orthostatic. It is important to note that both of these are additive rather than synergistic mechanisms.9
Postprandial Hypotension
A patient is said to have PPH if he or she experiences a fall in systolic BP of at least 20 mmHg or more in a supine/sitting position within 120 minutes following a meal.10 While PPH is distinct from OH, both may exist in the same patient.10 PPH is common in the elderly as well as in those with Parkinson’s disease or a disorder of the autonomic system.9 It is thought that PPH may occur through one or more of the following mechanisms: release of vasodilatory peptides in the gastrointestinal (GI) tract, impairment of the baroreceptor reflex, peripheral vasoconstriction, inadequate CO postprandially, or increased postprandial splanchnic blood.11 The size, content, timing and temperature of the meal all seem to affect PPH (TABLE 2).9,12 Pharmacists can advise patients to try remaining in a supine position following a meal. Specifically, this may help those who have both OH and PPH.12 Particularly in the elderly, adequate hydration is essential in preventing PPH.12 Effective treatment options are presently scarce and relatively limited.13 Up until recently, medications such as caffeine and octreotide were used; acarbose is only just being tested.
Caffeine:There is inconclusive and conflicting evidence to establish the use of caffeine for the management of PPH.9,10,12 While it is thought that caffeine antagonizes the effects of vasodilators, its mechanism is not fully understood.9,14 However, if given before a meal, it may reduce the postprandial fall in BP in some patients. Effective doses range from 60 to 200 mg (about one to two cups of coffee). Since tea and coffee are readily available and relatively cheap, caffeine is worth trying in patients who are affected by PPH. Caffeine is associated with side effects such as diarrhea, tremors, sleep disorders, and tachycardia.
Octreotide:Octreotide has established its use in elderly hypertensive patients with PPH and in those with autonomic failure. Its effect is thought to be mediated through a direct increase in splanchnic blood flow and forearm vascular resistance as well as the blockage of intestinal and pancreatic hormones.9,12,14 Octreotide, however, is relatively expensive and is administered as a single premeal dose of 25 to 50 mcg via subcutaneous injection. The patient may experience pain at the site of injection as well as diarrhea, nausea, and alopecia.12
Acarbose:Acarbose has been shown to reduce PPH in patients with autonomic failure.14 In part, it is thought that by decreasing the breakdown of complex carbohydrates, acarbose inhibits the action of alpha-glucosidase. This results in the decreased secretion of insulin, which has a vasodilatory effect, as well as other GI hormones. This finding may explain why the carbohydrate portion of a meal exerts the greatest hypotensive effect.14 The normal dose is 100 mg of acarbose taken 20 minutes before meals three times a day. Common side effects include abdominal pain, diarrhea, and flatulence.
A number of drugs, including midodrine, dihydroergotamine, indomethacin, diphenhydramine, cimetidine, fludrocortisone, and vasopressin, have all given variable results in different studies for the management of PPH.12
Orthostatic Hypotension
The joint consensus of the American Autonomic Society and the American Academy of Neurology defines OH as a “reduction of systolic blood pressure of at least 20 mmHg or diastolic blood pressure of at least 10 mmHg within 3 minutes of standing.”15 The effective management of OH is essential since it is a predictor of vascular deaths, particularly in the elderly and in patients with diabetes.16 The prevalence in the elderly population ranges between 5% and 30% and differs depending upon whether the patient is experiencing a reduction in the systolic or diastolic BP.16,17 OH can be caused by both neurogenic and nonneurogenic factors that fall into one of four categories: drugs, autonomic disorders, hypovolemia, and miscellaneous disorders (TABLE 3).5
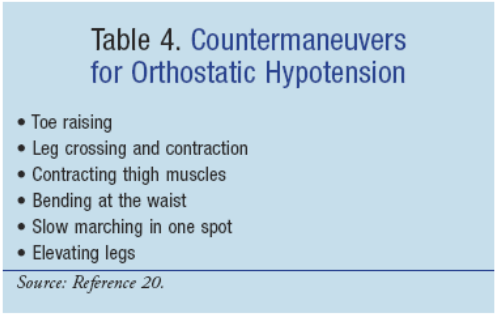
Treatment is aimed at improving postural symptoms and removing the underlying cause.18-20 Patients may be advised to increase their salt and fluid intake as a first step to management.18 There are a number of other nonpharmacologic measures that can be used to overcome OH, including compression of the venous capacitance bed and physical countermaneuvers before pharmacologic therapy is initiated.21 Some examples of countermaneuvers that should be performed for around 30 seconds at a time are listed in TABLE 4.
Any drug that the patient is taking may be responsible for the patient’s symptoms, and this possibility needs to be ruled out before treatment can be started.18 In some cases, hypotension can be the result of combining two medications. If the benefits of discontinuing the contributory medications do not outweigh the risks, then other methods to manage the hypotension need to be sought. On the other hand, it is important to avoid supine hypertension, a common flip side to pharmacologic therapy, and congestive heart failure, particularly in patients with diabetes or ischemic heart disease.5,22
Drug Therapy
Drug therapy can have a beneficial effect on OH if used correctly. It is important to note that currently all of the drugs listed below, except for midodrine, are used off-label for the management of OH.22
Fludrocortisone:Fludrocortisone is a mineralocorticoid that increases the volume of extravascular body fluid and improves alpha-adrenergic sensitivity.5,18,22 The normal dose is 0.1 to 0.2 mg/day, but can be increased to 0.4 to 0.6 mg/day.22 Since it can cause volume overload as well as hypokalemia and/or hypomagnesemia, fludrocortisone should be administered in minimally effective doses.18 With higher doses, patients may require potassium supplementation.23 Unfortunately, treatment is limited by the consequential supine hypertension.22 Patients may also complain of headache, edema, and weight gain.18
Midodrine:Midodrine is an inactive prodrug that is converted to the selective alpha1-adrenoceptor agonist desglymidodrine by hydrolysis following oral administration.5 Desglymidodrine is 15 times more potent than midodrine.23 It acts as a vasoconstrictor that is useful in the management of neurogenic OH.20,24 Since it is a vasopressor, midodrine is not useful in patients whose OH is due to low fluid volume.20 It has been shown to increase the standing systolic BP, reduce orthostatic lightheadedness, and increase standing and walking time.20
The recommended starting dose for midodrine is 2.5 mg orally given two to three times daily and gradually increased up to 10 mg three times daily only in patients who respond to initial therapy.24 The drug has an onset of action of 0.5 to 1 hour, and its effect can last up to 4 hours.22 For optimal therapy, the doses should be spread out based on when the patient experiences the most severe symptoms.24 Midodrine does cause supine hypertension in up to 25% of patients, a side effect that can reduced by taking the dose at least 4 hours before retiring and by tilting the patient’s bed.24 Pharmacists and other health care professionals should advise patients to have their BP checked regularly to monitor for any excessive increases in supine BP.24 Patients may also complain of pupillary dilation, piloerection (“goose bumps”), paresthesias, pruritus, and scalp tingling.18,22 Midodrine is contraindicated in patients with renal disease, urinary retention, heart disease, pheochromocytoma, or thyrotoxicosis.24
Pyridostigmine:Pyridostigmine causes a fairly small but noticeable improvement in OH without producing supine hypertension.22 The use of pyridostigmine is based on the fact that by inhibiting the action of acetylcholinesterase, it improves ganglionic neurotransmission in the sympathetic baroreflex pathway.20,22 In some patients, autonomic failure affects the neurotransmitter acetylcholine. By reducing the degradation of acetylcholine by acetylcholinesterase, pyridostigmine results in an improvement in standing BP, particularly the diastolic component.25
Pyridostigmine is useful in patients with mild OH in doses of 30 to 60 mg given two to three times daily.22 It may be combined with 5 mg of midodrine for patients experiencing more severe OH, but the use of these drugs in combination is yet to be further investigated.22 Patients taking pyridostigmine commonly experience cholinergic side effects such as abdominal cramps, diarrhea, nausea and vomiting, urinary frequency, miosis, blurred vision, and hypersalivation.22,26 More serious side effects include atrioventricular block, arrhythmias, hypotension, severe syncope, hypertension, cardiac arrest, bronchospasm, pulmonary edema, paralysis, anaphylaxis, and seizures.26
Pyridostigmine is contraindicated in any patient with a GI obstruction or peritonitis. It should be used with caution in patients with asthma, cardiovascular disorders, epilepsy, hyperthyroidism, parkinsonism, renal impairment, or peptic ulcer disease.26
Epoetin alfa:This agent works by rectifying the anemia that is often associated with autonomic disorders. It produces an increased standing BP and orthostatic tolerance in patients with OH.23 The usual dose is 25 to 75 U/kg three times weekly given subcutaneously or intravenously.23 Often patients are prescribed supplemental iron to increase the hematocrit.23 Pharmacists are ideally positioned to discuss any GI symptoms patients may suffer while taking iron supplements. Erythropoietin is also associated with supine hypertension as well as an increased appetite, which is a common side effect, along with an increased sense of well-being.18
Prospective Drug Therapy
Droxidopa (l-threo-3,4-dihydroxyphenylserine or l-DOPS) is a precursor amino acid that is converted to norepinephrine in the body. Patients who suffer from disorders of autonomic failure such as Parkinson’s disease that are frequently associated with OH are missing the neurotransmitter norepinephrine. The basis for the use of this drug in such patients is to replenish this neurotransmitter, with the aim of managing the OH. Droxidopa is usually given in doses of 300 to 600 mg daily as a divided dose for the treatment of OH.26 While this agent has been used in Japan for many years, it has not yet been approved by the FDA for use in the United States.
Other drugs under investigation for use in OH include yohimbine, dihydroergotamine, cyclooxygenase inhibitors, domperidone, and metoclopramide.23,27
Role of the Pharmacist
Pharmacists play a wide and varied role in supporting patients with OH. This ranges from monitoring patients’ BP regularly to counseling them on lifestyle and medications. Additionally, pharmacists should encourage patients to update them on any medication they are taking that may interfere with BP.
REFERENCES
1. Dahlgren G, Irestedt L. The definition of hypotension affects its incidence. Acta Anaesthesiol Scand. 2010;54:907-908. 2. Zanni GR, Wick JY. Hypotension: not a normal part of aging. Pharmacy Times. August 1, 2006. www.pharmacytimes.com/publications/issue/2006/2006-08/2006-08-5782/. Accessed September 6, 2011. 3. Longo DL, Fauci As, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2011. 4. Low blood pressure. American Heart Association. www.heart.org/HEARTORG/HealthcareResearch/GetWithTheGuidelinesHFStroke/GetWithTheGuidelinesStrokeHomePage/Contact-Get-With-The-Guidelines-Stroke_UCM_308038_Article.jsp/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Low-Blood-Pressure_UCM_301785_Article.jsp. Accessed September 11, 2011. 5. Maule S, Papotti G, Naso D, et al. Orthostatic hypotension: evaluation and treatment. Cardiovasc Hematol Disord Drug Targets. 2007;7:63-70. 6. Understanding low blood pressure—the basics. WebMD. www.webmd.com/heart/understanding-low-blood-pressure-basics. Accessed September 11, 2011. 7. Cronin H, Kenny RA. Cardiac causes for falls and their treatment. Clin Geriatr Med. 2010;26:539-567. 8. Katzung BG, Masters S, Trevor AJ. Basic and Clinical Pharmacology. 11th ed. New York, NY: McGraw-Hill Medical; 2009. 9. Luciano GL, Brennan MJ, Rothberg MB. Postprandial hypotension. Am J Med. 2010;123:281.e1-e6. 10. O’Mara G, Lyons D. Postprandial hypotension. Clin Geriatr Med. 2002;18:307-321. 11. Aronow WS, Ahn C. Postprandial hypotension in 499 elderly persons in a long-term health care facility. J Am Geriatr Soc. 1994;42:930-932. 12. Jansen RW, Lipsitz LA. Postprandial hypotension: epidemiology, pathophysiology, and clinical management. Ann Intern Med. 1995;122:286-295. 13. Gentilcore D, Horowitz M, Jones KL. Acarbose and postprandial hypotension. Hypertension. 2007;50:e159-e160. 14. Shibao C, Gamboa A, Diedrich A. Acarbose, an a-glucosidase inhibitor, attenuates postprandial hypotension in autonomic failure. Hypertension. 2007;50:54-61. 15. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J Neurol Sci. 1996;144:218-219. 16. Luukinen H, Koski K, Laippala P, Kivelä SL. Prognosis of diastolic and systolic orthostatic hypotension in older persons. Arch Intern Med. 1999;159:273-280. 17. Low PA. Prevalence of orthostatic hypotension. Clin Auton Res. 2008;18(suppl 1):8-13. 18. Bradley JG, Davis KA. Orthostatic hypotension. Am Fam Physician. 2003;68:2393-2398. 19. Hollister AS. Orthostatic hypotension: causes, evaluation, and management. West J Med. 1992;157:652-657. 20. Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: as easy as A, B, C. Cleve Clin J Med. 2010;77:298-306. 21. Grubb BP, Kosinski DJ, Kanjwal Y. Orthostatic hypotension: causes, classification, and treatment. Pacing Clin Electrophysiol. 2003;26:892-901. 22. Low PA, Singer W. Update on management of neurogenic orthostatic hypotension. Lancet Neurol. 2008;7:451-458. 23. Freeman R. Treatment of orthostatic hypotension. Semin Neurol. 2003;23:435-442. 24. McClellan KJ, Wiseman LR, Wilde MI. Midodrine: a review of its therapeutic use in the management of orthostatic hypotension. Drugs Aging. 1998;12:76-86. 25. Singer W, Sandroni P, Opfer-Gehrking TL, et al. Pyridostigmine treatment trial in neurogenic orthostatic hypotension. Arch Neurol. 2006;63:513-518. 26. Sweetman SC, ed. Martindale: The Complete Drug Reference. 34th ed. London, UK: Pharmaceutical Press; 2005 [electronic version]. 27. Kaufmann H. Neurogenic orthostatic hypotension: new prospects in treatment. Clin Auton Res. 2008;18(suppl 1):1. 28. Jansen RW, Hoefnagels WH. Postprandial blood pressure reduction. Neth J Med. 1990;37:80-88.







 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 