這算是很古早的一種用法了,曾經也有用過治療很輕度的肺高壓。
使用的原因是因為吸入性的lasix可以抑制氣喘病人在運動時所發生的氣管收縮和antigen challenge。
雖然也可以保護allergen誘導的氣喘反應。主要都是做用在肺部,和其原本利尿的效果比較沒有關係。
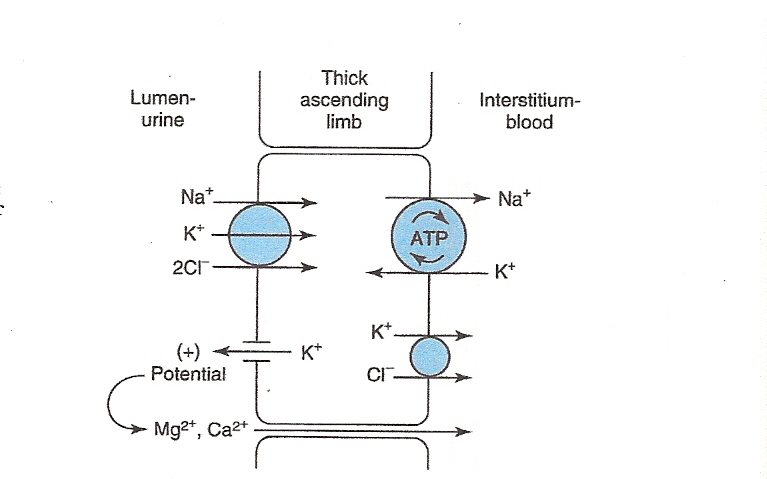
回憶一下我們熟知的furosemide機轉:
圖解藥理學 05腎元05
作用在亨利氏環上行枝厚部,抑制Na+-K+-2Cl-共同運送 系統(cotransport system),使Na+、Cl-、K+的排出量增加, 而Ca2+、Mg2+排出量亦增加。
可促進PGE2釋放,降低腎臟 血管阻力、增加腎血流量。
所以可能機轉為:
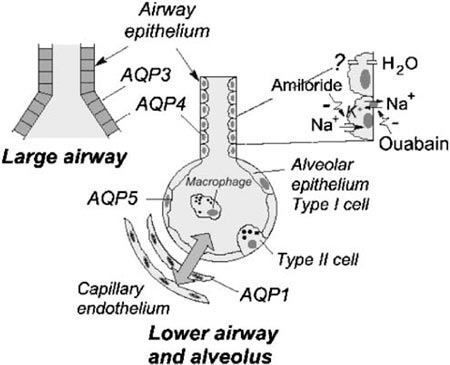
1. 在氣管的上皮細包有個Na/K/Cl的通道,而lasix會抑制這個通道,進而增加氣管的滲透度(和水份進出有關)。
2. 由於細胞的鈣、鎂、鈉排出量增加,進而讓氣管平滑肌放鬆。
3. 增加氣管中的prostaglandin E2 還有 pulmonary endothelium-derived prostaglandin I2,這些都有些血管保護的作用。
另外也有人說可能是因為抑制由發炎細胞釋放出來的物質,如:LTC4、histamine、neutrophil chemotactic factors,
你也可以從這邊回憶一下他們的機轉:圖解藥理學-10 發炎機轉 01
事實上,Amiloride也被這樣用過,不過機轉是減少氣管水腫
最後補充一些相關資料給各位:
Protective effect of inhaled furosemide on allergen-induced early and late asthmatic reactions.
The New England Journal Of Medicine [N Engl J Med] 1989 Oct 19; Vol. 321 (16), pp. 1069-73.
摘要
The movement of ions and water across the membranes of bronchial cells is part of the control of the bronchial obstructive response to physical stimuli. In a double-blind, randomized, crossover study, we compared the effect of an aerosol of the loop diuretic furosemide with that of a placebo on the early (within 60 minutes) and late (4 to 12 hours) asthmatic responses to a specific inhaled allergen. We studied 11 subjects with mild allergic asthma, who had both early and late asthmatic responses to a specific inhaled allergen in a preliminary challenge. After placebo administration, the maximal changes (mean +/- SE) from base line in the forced expiratory volume in one second (FEV1) and specific airway resistance were, respectively, a decrease of 35 +/- 4 percent and an increase of 288 +/- 56 percent between 0 and 60 minutes after inhalation of the allergen (early response) and a decrease of 35 +/- 5 percent and an increase of 301 +/- 40 percent between 4 and 12 hours (late response). After furosemide administration (4 ml; 10 mg per milliliter), the early response to inhaled allergen was markedly attenuated in all the subjects, and the late response in all but one. The maximal changes in the FEV1 and specific airway resistance were, respectively, a decrease of 11 +/- 2 percent and an increase of 61 +/- 2 percent between 0 and 60 minutes and a decrease of 20 +/- 4 percent and an increase of 178 +/- 25 percent between 4 and 12 hours (P less than 0.05 for all comparisons). No significant differences were seen in the bronchoconstrictor response to inhaled methacholine after furosemide or placebo administration. We conclude that a furosemide-sensitive mechanism in the airways is involved in the pathogenesis of the reactions of patients with allergic asthma. Whether inhaled furosemide might be useful in the treatment of allergic asthma is uncertain and will require further study.
J Pediatr Pharmacol Ther. 2011 Jan-Mar; 16(1): 14–22.
Nebulized Furosemide in the Treatment of Bronchopulmonary Dysplasia in Preterm Infants
另外幾篇給大家參考:
Effect of Inhaled Furosemide on Bronchial Responsiveness to Methacholine.pdf (1.7 MB)
Topical_furosemide_versu.pdf (205 KB)
Furosemide_inhalation_in.pdf (103 KB)
不過實際使用的效果並不好,建議是沒有方法可以用的時候再考慮吧。






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 