[EXCERPTS]
Major Recommendations
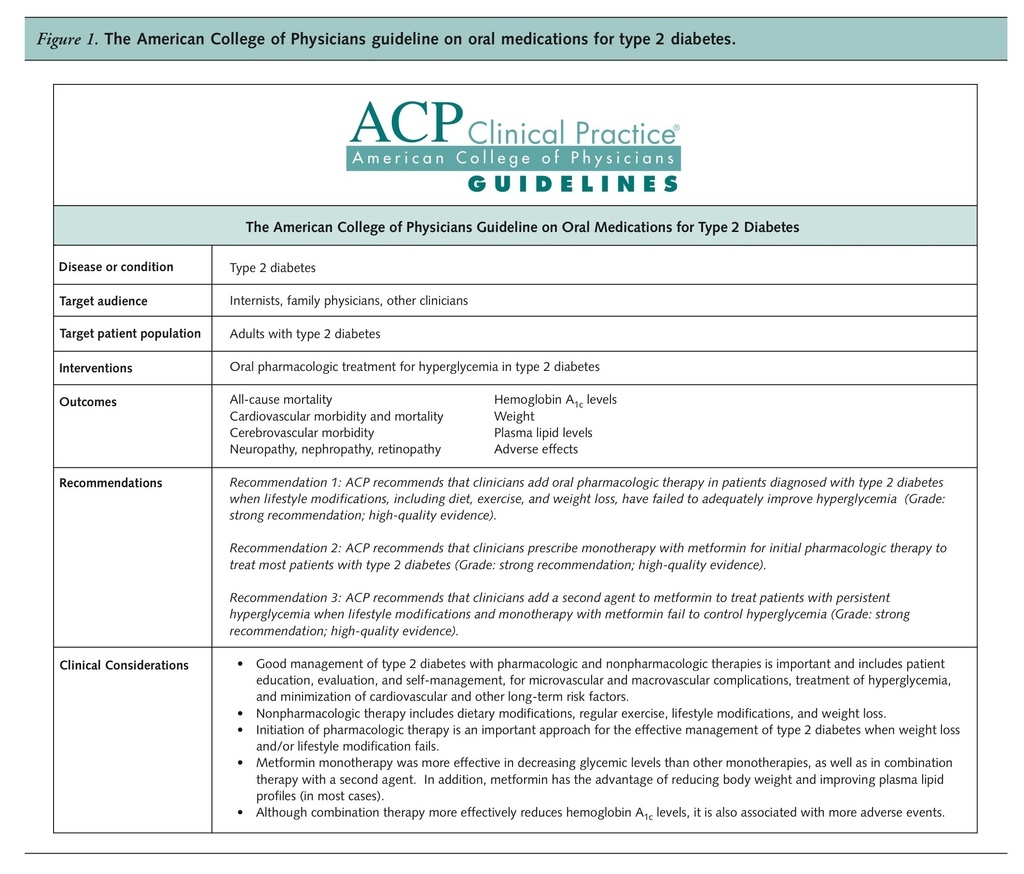
Recommendation 1: The American College of Physicians (ACP) recommends that clinicians add oral pharmacologic therapy in patients diagnosed with type 2 diabetes when lifestyle modifications, including diet, exercise, and weight loss, have failed to adequately improve hyperglycemia (Grade: strong recommendation; high-quality evidence).
Initiation of oral pharmacologic therapy is an important approach to effective management of type 2 diabetes. There are no data on the best time to add oral therapies to lifestyle modifications; thus, to avoid an unacceptable burden on patients, other complicating factors should be considered, such as life expectancy of the patient, presence or absence of microvascular and macrovascular complications, risk for adverse events related to glucose control, and patient preferences. The goal for hemoglobin A1c (HbA1c) should be based on individualized assessment of risk for complications from diabetes, comorbidity, life expectancy, and patient preferences. An HbA1c level less than 7% based on individualized assessment is a reasonable goal for many but not all patients.
Recommendation 2: ACP recommends that clinicians prescribe monotherapy with metformin for initial pharmacologic therapy to treat most patients with type 2 diabetes (Grade: strong recommendation; high-quality evidence).
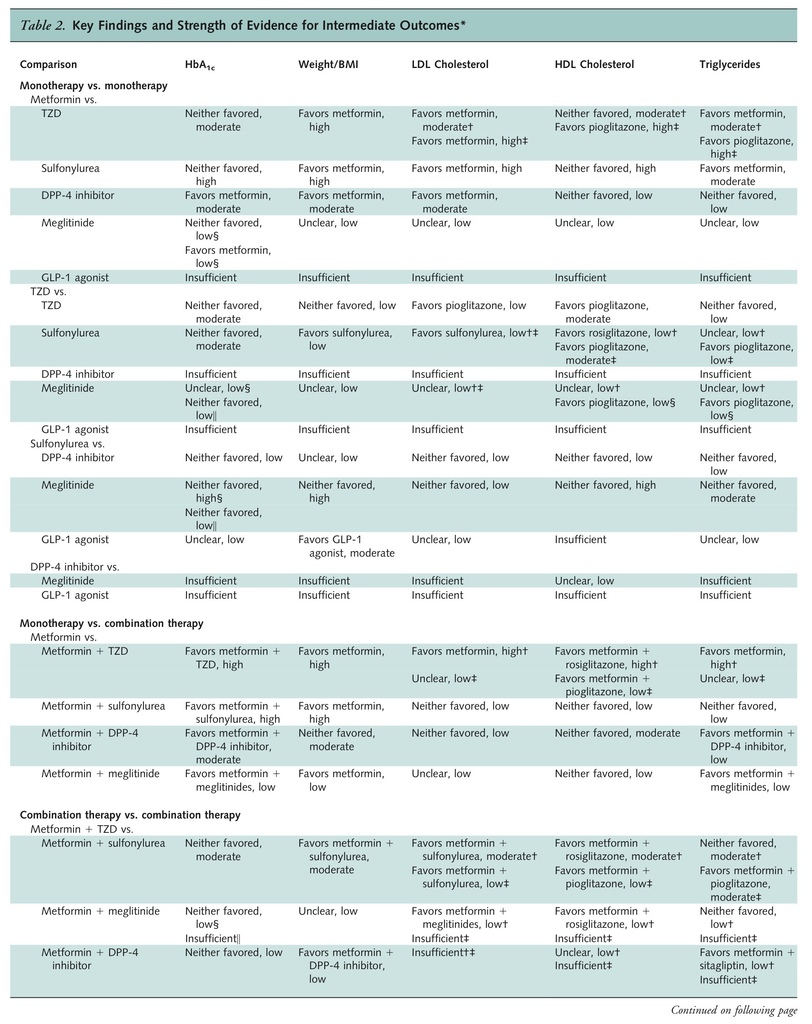
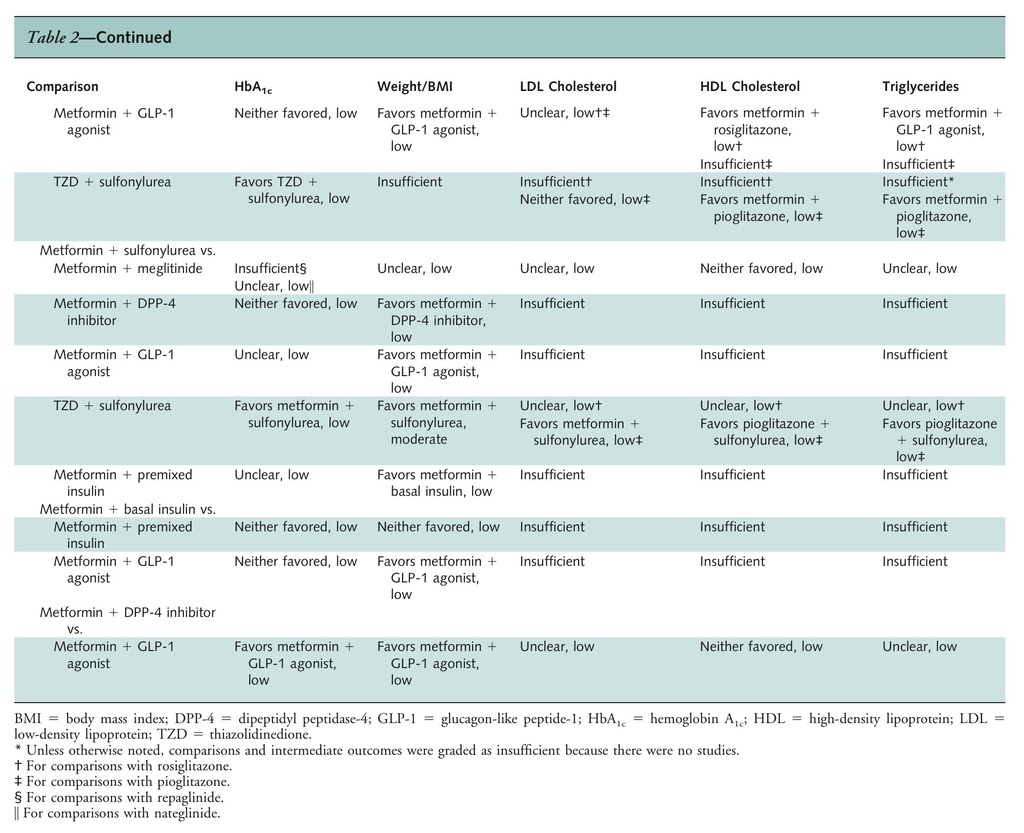
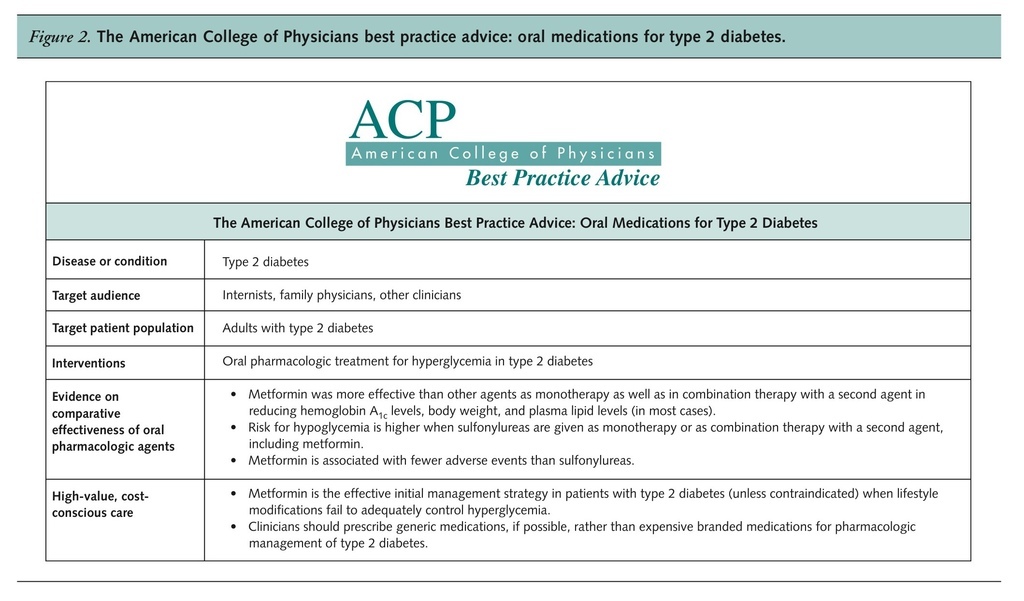
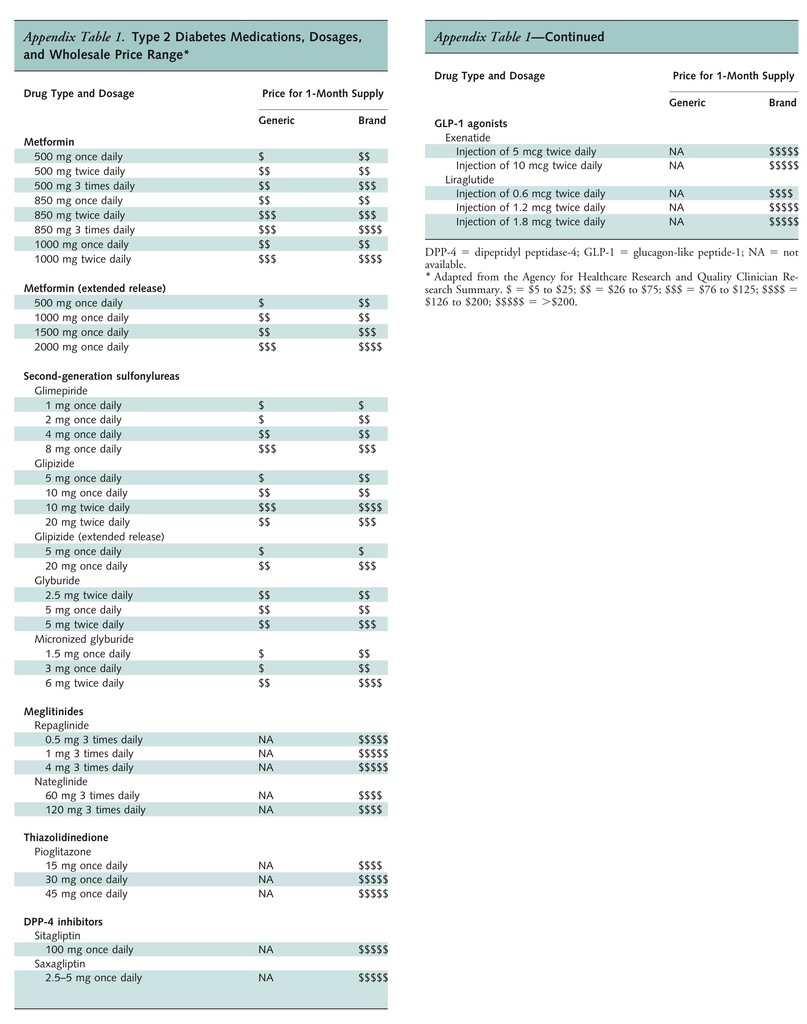
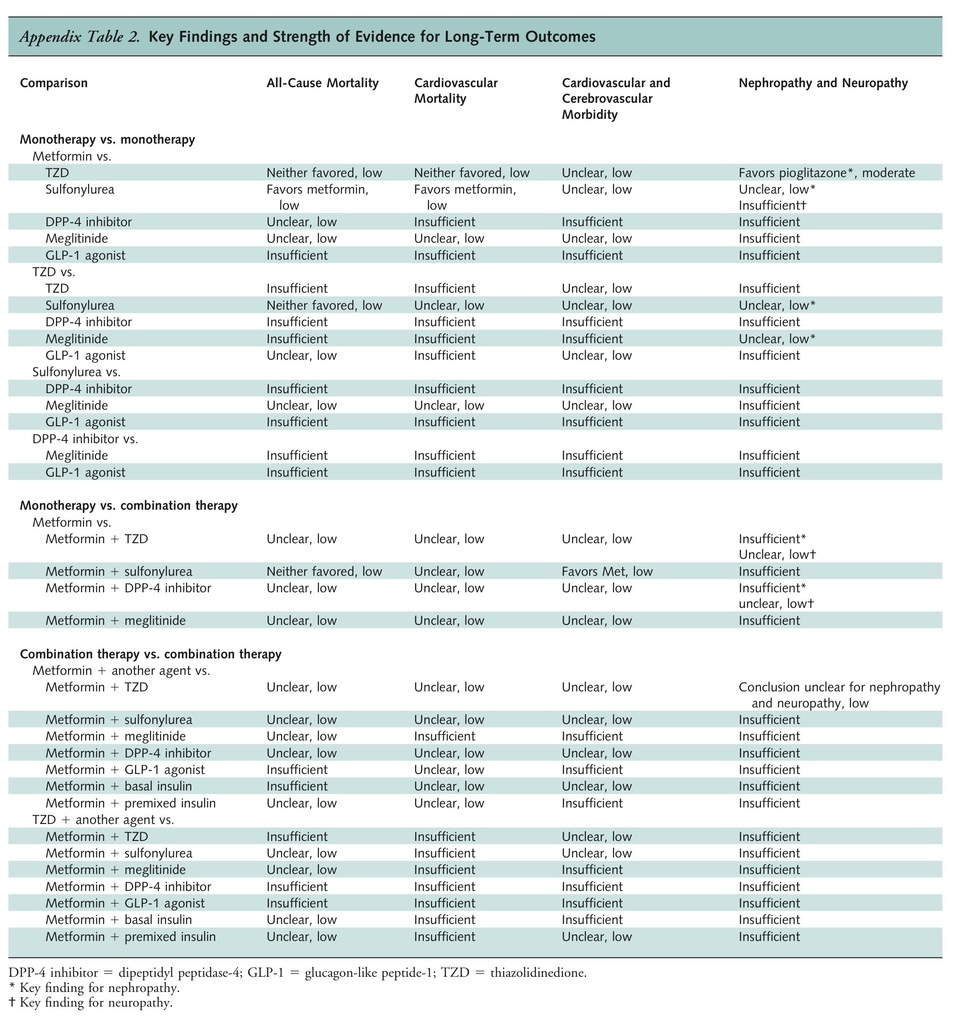
The effectiveness, adverse effect profiles, and costs of various oral pharmacologic treatments vary. Metformin is more effective than other pharmacologic agents in reducing glycemic levels and is not associated with weight gain. In addition, metformin aids in decreasing weight and reduces low-density lipoprotein (LDL) cholesterol and triglyceride levels. Metformin was also associated with slightly lower all-cause mortality and cardiovascular mortality compared with sulfonylureas. Finally, metformin is associated with fewer hypoglycemic episodes and is cheaper than most other pharmacologic agents. Therefore, unless contraindicated, metformin is the drug of choice for patients with type 2 diabetes, in addition to lifestyle modification. Metformin is contraindicated in patients with impaired kidney function, decreased tissue perfusion or hemodynamic instability, liver disease, alcohol abuse, heart failure, and any condition that might lead to lactic acidosis.
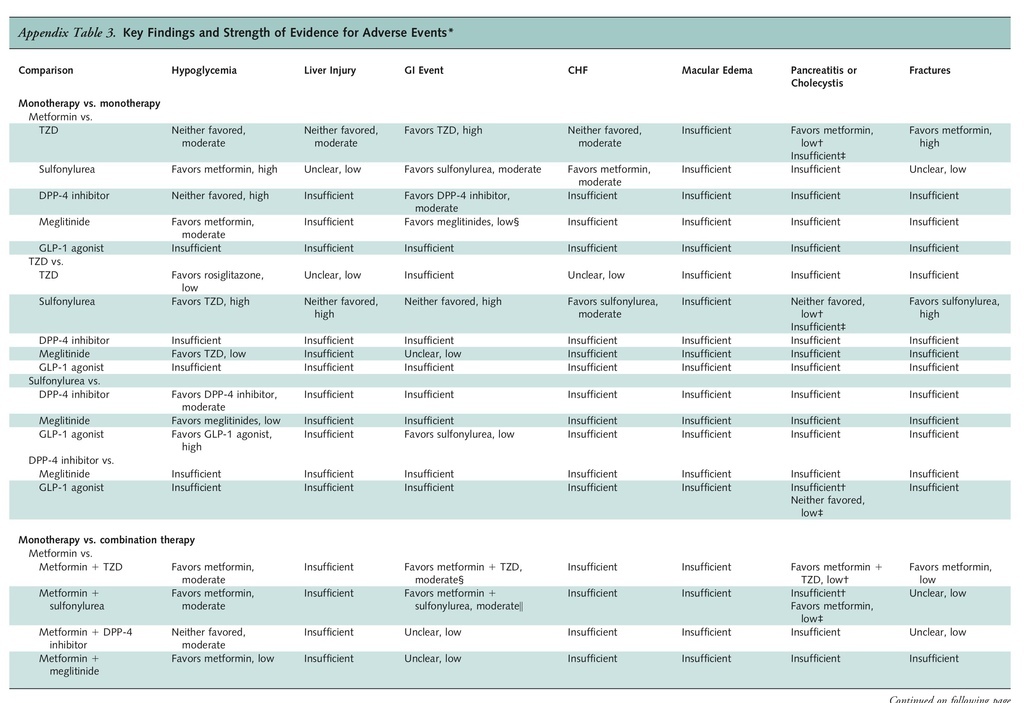
Physicians and patients should discuss adverse event profiles before selecting a medication. Compared with baseline values, most diabetes medications (metformin, thiazolidinediones, and sulfonylureas) reduced baseline HbA1c by about 1 percentage point 3 or more months after the initiation of treatment. For adverse effects, metformin is associated with an increased risk for gastrointestinal side effects, sulfonylureas and meglitinides are associated with an increased risk for hypoglycemia, and thiazolidinediones are associated with an increased risk for heart failure (with no conclusive evidence for an increase in ischemic cardiovascular risk). However, in comparing the effectiveness of various agents, the evidence shows that metformin is the most efficacious agent as monotherapy and in combination therapy.
Recommendation 3: ACP recommends that clinicians add a second agent to metformin to treat patients with persistent hyperglycemia when lifestyle modifications and monotherapy with metformin fail to control hyperglycemia (Grade: strong recommendation; high-quality evidence).
All dual-therapy regimens were more efficacious than monotherapies in reducing the HbA1c level in patients with type 2 diabetes by about 1 additional percentage point. Combination therapies with more than 2 agents were not included in the evidence review. No good evidence supports one combination therapy over another, even though some evidence shows that the combination of metformin with another agent generally tends to have better efficacy than any other monotherapy or combination therapy. However, combination therapies are also associated with an increased risk for adverse effects compared with monotherapy. Generic sulfonylureas are the cheapest second-line therapy; however, adverse effects are generally worse with combination therapies that include a sulfonylurea.
Although this guideline addresses only oral pharmacological therapy, patients with persistent hyperglycemia despite oral agents and lifestyle interventions may need insulin therapy.
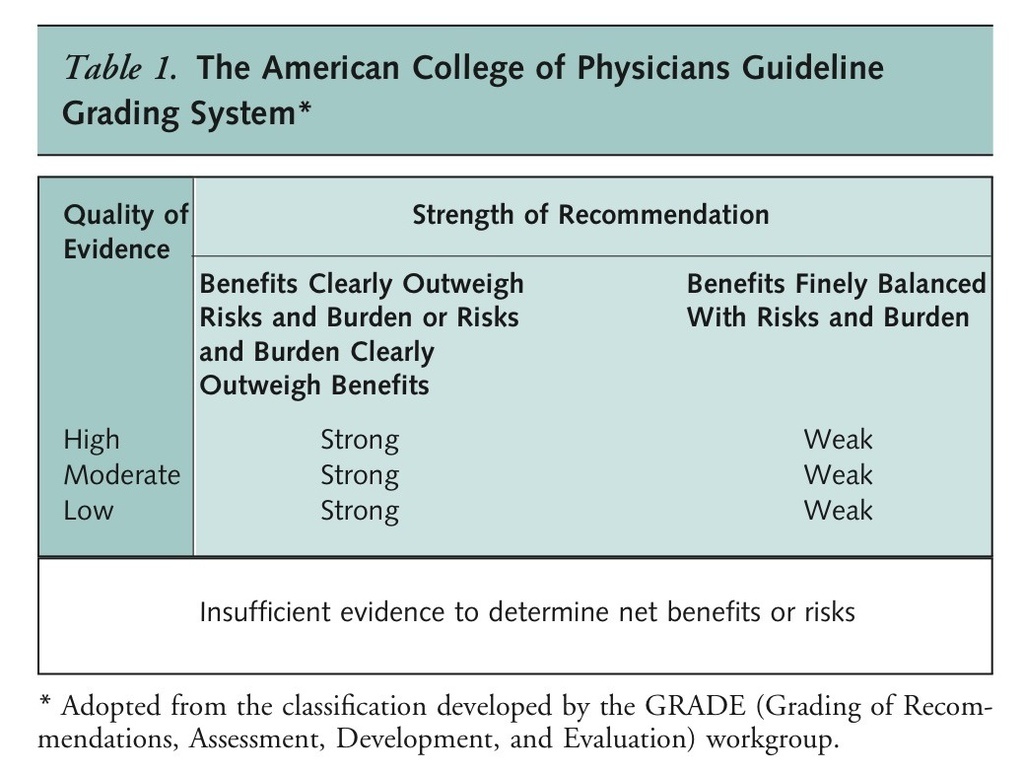
DefinitionsLevels of Evidence [Available Online]
[Link to free full-text guideline at National Guideline Clearinghouse | Annals article PDF]






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 