- Susanne Dallinger, MD; Barbara Bobr, MD; Oliver Findl, MD; Hans-Georg Eichler, MD; Leopold Schmetterer, PhD
Abstract
Background and Purpose—The acetazolamide provocation test is commonly used to study cerebrovascular vasomotor reactivity. On the basis of the effect of a carbonic anhydrase inhibitor in the central nervous system, we hypothesized that acetazolamide may also increase blood flow in the human choroid.
Methods—In a placebo-controlled, randomized, double-blind, three-way crossover design, acetazolamide (500 mg or 1000 mg IV) or placebo was administered to nine healthy subjects. The effect of acetazolamide was studied at 15-minute intervals for 90 minutes. Pulsatile choroidal blood flow was assessed with laser interferometric measurement of fundus pulsation. In addition, mean blood flow velocity and resistive index in the ophthalmic artery were measured with Doppler sonography. In a second study in six healthy subjects, we assessed the effect of acetazolamide (1000 mg IV) on intraocular pressure.
Results—Acetazolamide increased fundus pulsation amplitude in a dose-dependent manner (1000 mg: +33%; 500 mg: +20%; P<0.001, ANOVA). The effect of acetazolamide on MFV (1000 mg: +18%; 500 mg: +8%; P=0.003, ANOVA) and RI (1000 mg: −4%; 500 mg: −2%; P=0.006, ANOVA) was less pronounced but also significant. Acetazolamide did not induce any changes in systemic hemodynamic parameters but significantly decreased intraocular pressure (1000 mg: −37%; P<0.0001).
Conclusions—The present data show for the first time that intravenously administered acetazolamide increases choroidal blood flow in humans. This phenomenon therefore indicates that the acetazolamide provocation test may qualify as a tool to investigate ocular vasomotor reactivity in a variety of ocular diseases. Moreover, the increase in choroidal blood flow after carbonic anhydrase inhibition can be expected to contribute to the therapeutic efficacy of carbonic anhydrase inhibitors in glaucoma.
Several investigators have shown that acetazolamide causes an increase in cerebral blood flow.1 2 3 The so-called acetazolamide provocation test has been used to study cerebral blood flow under both physiological and pathological conditions.2 3 4 5 Compared with other tests such as the CO2 provocation test, the administration of acetazolamide has the distinct advantage of reduced side effects.
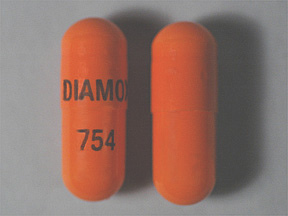
In ophthalmology, carbonic anhydrase inhibitors are used orally in the treatment of primary and secondary open-angle glaucoma. Oral acetazolamide is chosen as an ocular hypotensive treatment if topical antiglaucoma drugs fail to properly reduce IOP. Acetazolamide can also be administered intravenously or intramuscularly as part of the acute treatment of angle-closure glaucoma.6 In addition, this drug has been used for the treatment of macular edema7 and retinitis pigmentosa.8
The therapeutic efficacy of carbonic anhydrase inhibitors suggests potential vasodilator effects of acetazolamide in the ocular vasculature. However, the effect of acetazolamide on choroidal blood flow and its physiological and pathophysiological implications have not yet been investigated. We address this issue in our report.
Subjects and Methods
Subjects
After ethics committee approval, nine healthy male volunteers (age range, 22 to 33 years; mean±SD age, 26.2±3.4 years) participated in study A, and six healthy male volunteers (age range, 22 to 30 years; mean±SD age, 25.7±2.7 years) were enrolled in study B. The nature of these studies, detailed below, was explained, and all subjects gave written consent to participate. Each subject passed a screening examination that included medical history and physical examination; 12-lead ECG; complete blood count; activated partial thromboplastin time; thrombin time; fibrinogen; clinical chemistry (sodium, potassium, creatinine, uric acid, glucose, cholesterol, triglycerides, alanine aminotransferase, aspartate aminotransferase, γ-glutamyltransferase, alkaline phosphatase, total bilirubin, total protein); hepatitis A, B, C, and HIV serology; urine analysis; and a urine drug screen. Subjects were excluded if any abnormality was found as part of the screening unless the investigators considered an abnormality clinically irrelevant. Furthermore, an ophthalmic examination, including slit lamp biomicroscopy and indirect funduscopy, was performed. Inclusion criteria were normal ophthalmic findings and a refractive error of less than 3 diopters in either eye.
Study Design
In study A, subjects were studied according to a placebo-controlled, randomized, double-blind, three-way balanced crossover design with washout periods of at least 2 days between study days. On the trial days subjects arrived after an overnight fast and were studied in a sitting position. After steady state conditions were reached, which was ensured by repeated blood pressure measurements during the resting period, hemodynamic baseline measurements were taken. Thereafter, acetazolamide (500 or 1000 mg; Wyeth Lederle) or placebo was administered intravenously as a short-term infusion. Measurements were performed during every 15 minutes after the start of the infusion for 90 minutes. Subjects crossed over to the other treatment regimen on the remaining days of the trial.
In study B, six subjects were studied in an open design. On the trial days subjects arrived after an overnight fast and were studied in a sitting position. After steady state conditions were reached, which was again ensured by repeated blood pressure measurements during the resting period, hemodynamic baseline measurements were taken. Thereafter, acetazolamide (1000 mg) was administered intravenously as a short-term infusion. IOP and flow velocities of the OA were measured during every 15 minutes after the start of the infusion for 60 minutes.
IOP was not measured in study A because it is difficult to obtain technically adequate interference fringes when applanation tonometry is performed before laser interferometry. For the assessment of ocular fundus pulsation, the light portions reflected from the front side of the cornea and the fundus are overlapped. To obtain an adequate reflection from the front side of the cornea a regular tear film is necessary, which may not be the case after multiple IOP measurements. Hence, the effect of acetazolamide on IOP was investigated in a separate study.
Study Methods
Blood Pressure and Pulse Rate
Systolic, diastolic, and mean blood pressures were measured on the upper arm by an automated oscillometric device (HP-CMS patient monitor, Hewlett Packard). Pulse rate was automatically recorded from a finger pulse–oxymetric device (HP-CMS patient monitor).
Fundus Pulsations
Pulse-synchronous pulsations of the eye fundus were assessed by laser interferometry in the subject’s right eye. The method is described in detail by Schmetterer et al.9 Briefly, the eye is illuminated by the beam of a single-mode laser diode with a wavelength (λ) of 783 nm. The light is reflected at both the front side of the cornea and the retina. The two re-emitted waves produce interference fringes that allow the calculation of the distance changes between cornea and retina during a cardiac cycle. Distance changes between cornea and retina lead to a corresponding variation of the interference order [ΔN(t)]. This change in interference order can be evaluated by counting the fringes moving inward and outward during the cardiac cycle. Changes in optical distance [ΔL(t)], corresponding to the cornea-retina distance changes, can then be calculated by ΔL(t)=ΔN(t) · λ/2. The maximum distance change is termed the fundus pulsation amplitude (FPA) and estimates the local pulsatile blood flow.10 FPA was calculated as the mean of at least five cardiac cycles. The short-term and day-to-day variability of the method is small, which allows detection of even minor changes in local pulsatile blood flow following pharmacological stimulation.11 In contrast to systems recording ocular pressure pulse,12 13 14 information on the ocular circulation can be obtained with high transverse resolution. To obtain information on the choroidal blood flow, the macula, which lacks retinal vasculature, was chosen for measurements.
Doppler Sonography
In study A and study B, MFV, PSV, and EDV were determined in the right OA with color Doppler ultrasound.15 MFV was measured manually as time mean of the spectral outline. Measurements were performed with a 7.5-MHz probe (CFM 750, Vingmed Sound). The OA was measured at the point where it crosses the optic nerve. The sample volume marker was placed approximately 25 mm posterior to the globe. The RI in the OA was calculated as RI=(PSV−EDV)/PSV. The pulsatile fraction of blood flow in the OA was calculated as (MFV−EDV)/MFV.16 17 All parameters were determined as mean values over at least three cardiac cycles.
Applanation Tonometry
IOP was measured by Goldmann applanation tonometry (Haag-Streit). Measurements were performed on the right eye.
Data Analysis
It was assumed that changes of the flow pulsatility in the choroid in response to acetazolamide occurred approximately at the rate changes in the OA16 occurred. Hence, the change in (FPA*MFV)/(MFV−EDV) provoked by administration of acetazolamide was taken as an estimate of the change in total choroidal blood flow.
All statistical analyses were performed with the use of the Statistica software package (Release 4.5, StatSoft Inc). In study A, the effect of acetazolamide on hemodynamic parameters was assessed by Friedman ANOVA versus placebo. Post hoc comparison was performed with the Wilcoxon signed rank test with Bonferroni adjustment. In study B, the effect of acetazolamide on IOP and blood flow velocities in the OA was assessed by Friedman ANOVA versus baseline. For data description, values were expressed as percentage of baseline and are presented as mean±SEM. A two-tailed P<0.05 was considered the level of significance.
Previous Section
Next Section
Results
Study A
Baseline ocular hemodynamic parameters are presented in Table 1⇓. Notably, there were no significant differences in FPA, MFV, or RI between the 3 study days.
View this table:
Table 1.
Baseline Ocular Hemodynamic Parameters of the 3 Study Days
Figure 1⇓ and Table 2⇓ show the effect of acetazolamide or placebo on ocular hemodynamic parameters. All parameters under study showed a dose-dependent response to administration of acetazolamide. Both doses of acetazolamide significantly increased FPA compared with placebo (P<0.001, ANOVA). The maximum effects observed were +33% (P<0.001) and +20% (P<0.001) versus baseline at 1000 mg and at 500 mg, respectively. This effect remained significant for 45 minutes after drug administration.
Figure 1.
Effects of acetazolamide (1000 mg, ▿; 500 mg, ▴) or placebo (no symbols) on FPA, estimated choroidal blood flow (ChBF), RI, and MFV in the OA. Data are presented as mean±SD (n=9).
View this table:
Table 2.
Effect of Acetazolamide or Placebo on Systemic and Ocular Hemodynamic Parameters
The effect on MFV (P=0.003, ANOVA) and RI (P=0.006, ANOVA) in the OA was less pronounced but also reached the level of significance. The maximum effect of 1000 mg acetazolamide was +18% (P=0.011) on MFV and −4% on RI (P=0.023). In contrast, however, the changes in OA hemodynamic parameters induced by infusion of 500 mg acetazolamide did not reach the level of significance, as evidenced from post hoc comparisons (MFV, +8%; RI, −2%).
Acetazolamide caused a decrease in flow pulsatility in the OA, as also evidenced by the decrease in RI. Hence, the effect on estimated choroidal blood flow was more pronounced than that on FPA and improved highly significantly (P<0.001, ANOVA). Acetazolamide 1000 mg induced a maximum increase in estimated choroidal blood flow of +38% (P<0.001), whereas the effect of 500 mg was considerably less pronounced (+22%, P<0.001).
Notably, systemic blood pressure and pulse rate showed only minor changes during administration of the carbonic anhydrase inhibitor (Table 2⇑), despite pronounced changes of the ocular hemodynamic parameters.
Study B
The effect of acetazolamide on IOP, MFV, and RI of the OA is shown in Figure 2⇓ and Table 3⇓. Acetazolamide significantly decreased IOP (−37%, P<0.0001). The effect of acetazolamide on MFV (+19%, P=0.001) and RI (−4%, P=0.007) was also significant. Again, acetazolamide caused only minor changes in systemic hemodynamic parameters (Table 3⇓).
Figure 2.
Effects of acetazolamide (1000 mg) on MFV, RI, and IOP in the OA. Data are presented as mean±SD (n=6).
View this table:
Table 3.
Effect of Acetazolamide on IOP, MFV, and RI of the OA
Discussion
The present study shows that intravenous acetazolamide strongly increases choroidal blood flow in healthy subjects. In contrast, the response in MFV and RI in the OA was considerably lower, although still significant. This acetazolamide-induced effect was present until 45 minutes after drug administration. Our findings are in accordance with earlier reports elaborating that the response to acetazolamide in the blood flow velocity of the OA is smaller than the blood flow velocity in the cerebral artery.18 19 This phenomenon indicates that certain brain regions are more sensitive to carbonic anhydrase inhibition than others.
However, previous studies did not observe an effect of acetazolamide on RI in the OA. Harris et al19 administered 1000 mg acetazolamide orally and measured MFV and RI in the OA 3 hours after drug intake. No changes in hemodynamic parameters in the OA were reported. However, when hypercapnia was superimposed on acetazolamide, RI was significantly lowered in the central retinal artery. In contrast to our study, Harris et al19 administered acetazolamide orally, resulting in lower plasma levels. Our results suggest that the vasodilator action of acetazolamide in the OA can only be observed at high plasma levels, because a decrease in RI was only observed after 1000 mg IV acetazolamide. Kerty et al18 reported a significant decrease in OA flow velocities and in pulsatile ocular blood flow after administration of 1000 mg IV acetazolamide. These findings are in contrast to our results, and further studies will be needed to elucidate this discrepancy.
The role of the vasodilator response to acetazolamide in the overall therapeutic effect of carbonic anhydrase inhibitors in ocular diseases is not well understood. In glaucoma patients at least part of the beneficial effect can be attributed to the IOP-lowering effects of acetazolamide. However, several authors focused on the question of whether retinal vasodilation could also contribute to therapeutic efficacy. Not unexpectedly, Grunwald and Zinn20 did not observe an effect of oral acetazolamide on retinal blood flow. In contrast, Rassam et al21 reported an increase in retinal blood flow after intravenous administration of the same agent. This difference may again be attributed to the higher plasma levels obtained in the latter group. Furthermore, the beneficial effect of acetazolamide in patients with macular edema7 is compatible with a vasodilating effect in the choroid, since the central fovea contains no retinal vessels.
The mechanism underlying the vasodilator effect of acetazolamide in cerebral vessels has not yet been fully elucidated. However, there is evidence that carbonic anhydrase inhibitors may cause extracellular acidosis.22 It is worth noting that an increase in arterial PCO2, a stimulus that produces extracellular acidosis, also strongly increases choroidal23 24 25 26 27 and cerebral1 3 5 18 19 27 blood flow. Moreover, the response to hypercapnia is considerably smaller in the OA.19 27 These findings and our own observations allow speculations that the vascular reactivity to extracellular acidosis is particularly low in the OA.
The IOP-lowering effect of acetazolamide is well known and used in the treatment of glaucoma. Robinson et al28 reported an increase in ocular perfusion pressure after a reduction in IOP, and a rise in perfusion pressure may certainly contribute to an increase in choroidal blood flow. However, there is evidence from recent studies29 30 that choroidal blood flow is autoregulated in response to increased ocular perfusion pressure.
Although interesting from both a mechanistic and a clinical point of view, there are limitations of our study that need to be taken into account when the data are interpreted. Doppler sonography in the OA is only capable of measuring blood flow velocity. A calculation of blood flow in this artery, however, would require an accurate measurement of vessel diameter. Consequently, if acetazolamide increases the diameter of the OA, velocity measurements may underestimate the blood flow effect. This limitation has been discussed in detail for the middle cerebral artery,31 and this also seems to be true for the OA. The vasodilator action of acetazolamide in the vessels distal to the OA is evidenced from the decrease in RI. However, the ocular blood flow is only a small fraction of OA blood flow,32 and therefore changes in RI do not necessarily indicate changes in ocular vascular tone. For the estimation of acetazolamide-induced effects on choroidal blood flow, we used flow pulsatility as assessed in the OA, since fundus pulsation measurement only yields the pulsatile component of choroidal blood flow. However, this method does not require that baseline pulsatility in the OA and the choroid is equal; it only requires that acetazolamide-induced changes in flow pulsatility are comparable.
The results of the present study strongly indicate that the acetazolamide provocation test could be used to study choroidal vascular reactivity in patients with ocular vascular disease, such as glaucoma or age-related macular degeneration. Compared with the CO2 provocation test, the administration of acetazolamide induces less severe side effects3 and requires less compliance of the patient. Moreover, ocular fundus pulsation measurement can also be used to investigate carotid physiology and pathophysiology. Ocular pressure pulse measurement with the pneumotonometer has already been used extensively to investigate carotid occlusive disease.33 34 35 36 37 38 39 40 41 42 43 An additional advantage of laser interferometry over systems recording the ocular pressure pulse is improved reproducibility,11 44 although direct contact with the eye is not required for measurements.










 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 