Updated: Apr 9, 2010
Introduction
Background
Ochronosis is the bluish black discoloration of certain tissues, such as the ear cartilage and the ocular tissue, seen with alkaptonuria, a metabolic disorder. Additionally, ochronosis can occasionally occur from exposure to various substances such as phenol, trinitrophenol, resorcinol, mercury, picric acid, benzene, hydroquinone, and antimalarials.
Pathophysiology
Ochronosis was defined by Virchow who histologically described the connective tissue in alkaptonuria, given the cartilage's ochre, or yellow, hue under the microscope.
Alkaptonuria is a rare autosomal recessive metabolic disorder caused by deficiency of homogentisic acid oxidase, the only enzyme capable of catabolizing homogentisic acid (HGA). Alkaptonuria features a defect in the biochemical pathway by which phenylalanine and tyrosine are normally degraded into fumaric and acetoacetic acid. The genetic defect is autosomal recessive and is mapped to the HGO gene on arm 3q1, and 18 genetic missense mutations are known to cause homogentisic acid oxidase aberrations.[1 ]This deficiency results in accumulation and deposition of HGA in cartilage, causing the characteristic diffuse bluish black pigmentation. These affected connective tissue become weak and brittle with time, leading to chronic inflammation, degeneration, and osteoarthritis.
Exogenous ochronosis, in which bluish black pigmentation of cartilage is noted iatrogenically by exogenous agents, has been seen after exposure to noxious substances, including phenol, trinitrophenol, benzene, and hydroquinone.
Frequency
United States
Alkaptonuria is a rare autosomal recessive disease with a prevalence of 1 case per 1 million population.
International
Alkaptonuria occurs worldwide, with the highest frequency seen in the Czech Republic and Santo Domingo, in which the prevalence approaches 1 case per 25,000 inhabitants.
Mortality/Morbidity
- With the absence of homogentisic acid oxidase in liver and kidney cells, HGA accumulates. The black urine of patients with alkaptonuria results from renal excretion of HGA, while ochronotic pigment is a sequela of HGA accumulation in the connective tissues of individuals who are affected.
- In alkaptonuria, the accumulation of HGA inhibits collagen cross-linking by affecting a crucial enzyme in collagen synthesis, leading to a diminution of structural collagen integrity. This results in ochronotic arthropathy, which occurs in men aged in their fourth and fifth decades; women develop similar complications in their sixth decade. The larger joints are most affected with early calcification, narrowing, and collapse of the intervertebral discs. In addition to joint disease, reports suggest an increased incidence of cardiovascular disease due to cartilaginous changes of vessel walls.
- Homogentisic acid oxidase requires atmospheric oxygen, ferrous ion, and sulfhydryl groups for normal function, and the enzyme is inhibited by quinones. HGA is colorless in solution but darkens on exposure to air, especially in the presence of alkali. Individuals with acidic urine may not demonstrate the very dark-colored urine characteristic of this condition.
Race
Alkaptonuria is seen in persons of all races.
Sex
The incidence of alkaptonuria is equal in both sexes.
Age
Alkaptonuria is present at birth and is often diagnosed by discoloration of the diapers. Up to 25% of patients with alkaptonuria do not have the characteristic dark urine staining, and many patients remain undiagnosed until adulthood.
Clinical
History
- Alkaptonuria is often recognized at birth when parents note discoloration of the urine.
- Nevertheless, many patients with this metabolic disorder are symptomless until ochronotic changes occur with bluish black pigmented patches in the sclera developing in patients aged 30-39 years. These ocular discolorations are located between the corneal margin and the inner canthus.
- The fourth decade often marks the onset of thickening and blue-black or gray-blue discoloration of the ear cartilage.
- Other body locations that frequently display the alteration in skin hue are the eyelids, the forehead, the cheeks, the axillae, the genital region, the nail beds, the buccal mucosa, the larynx, the tympanic eardrum, and the tendons (most easily demonstrated by the patient making a fist).
- Ochronotic arthropathy develops later with arthritic symptoms.[2 ]
Physical
- Dark urine noted in diapers is usually the presenting manifestation of this entity.
- For those cases of alkaptonuria not diagnosed in infancy, black cerumen and axillary pigmentation may be noted before age 10 years.
- Gray-black scleral pigmentation in the configuration of small, dark rings is noted in the third decade.
- Ear cartilage alterations in the fourth decade include discoloration with a grayish blue hue, followed by structural changes with stiffness, contour irregularities, and calcification. Note the images below.

Ochronosis revealing a perioral bluish black macular eruption after hydroquinone use.

Periorbital discoloration due to excessive use of topical bleaching preparations containing hydroquinone.
- Ochronotic discoloration can also be detected on the nasal tip, the costochondral junctions, the extensor tendons of the hands, the cheeks, the fingernails, and the buccal mucosa.
- Arthritic signs of ochronotic arthropathy develop in the third and fourth decades. Narrowing of the joint spaces and disk calcifications occur.[3 ]Lower back, hip, and knee pain and stiffness are not uncommon.
- The clinical discoloration of the skin is a result of the formation of ochronotic pigment granules in the dermis and in the apocrine glands. Thus, the ochronotic changes of cartilaginous and tendinous structures are best appreciated in regions in which the overlying skin is of minimal thickness, such as the ears, the nasal tip, and the extensor tendons of the hands.
- Accumulation of this pigment in cardiac tissue can lead to an inflammatory reaction and progressive heart valve dysfunction.[4,5 ]
Causes
- Alkaptonuria is a genetic disorder related to a deficiency of homogentisic acid oxidase.[6 ]
- Ochronotic pigmentation can develop from medications. Similar skin and cartilage alterations can be induced by quinacrine administration and at sites of quinine injections.[7 ]Quinines directly inhibit homogentisic acid oxidase. Carbolic acid topical applications to cutaneous ulcers have also induced ochronotic skin alterations.
- Exogenous ochronosis has been reported with topical applications of phenol and hydroquinones to the skin.[8,9,10,11 ]In the case of hydroquinone, it is reported that 35% of African blacks exhibit ochronotic skin changes when using a 6-8% hydroquinone preparation over a prolonged period. Indeed, the prevalence among users of these skin lighteners has been stated to be 69% in a South African study. In African Americans, this cutaneous adverse effect of hydroquinones has been reported, even when using 2% hydroquinone products. With exogenous ochronosis, the arthropathy seen with alkaptonuria does not occur.
Differential Diagnoses
Argyria
Arsenical Keratosis
Other Problems to Be Considered
Ankylosing spondylitis[12 ]
Workup
Laboratory Studies
Most laboratory testing for alkaptonuria detects the alterations in the urine. Increased urinary levels of homogentisic acid (HGA) are characteristic of this metabolic disorder.
- Elevated levels of HGA in the urine, blood, and other tissues can be determined by specific enzymatic and colorimetric tests, direct spectrophotometric methods, high-performance liquid chromatographic testing, and molecular techniques.
- Other simple urinary studies include darkening of urine with the addition of sodium hydroxide, black reaction with FeCl3, and blackening of photographic emulsion paper with alkali added to urine.
Imaging Studies
In patients with ochronotic arthropathy, radiography and MRI help identify characteristic and diagnostic features, including articular space narrowing up to osseous ankylosis, calcifications, osteophytosis, and reactive sclerosis of the articular surfaces.[11,13,14 ]Bone scintigraphy can be useful in evaluation, correlation with the clinical course, and follow-up of such patients.[15 ]
Procedures
Dermoscopy has proved useful in exogenous ochronosis. In addition to melasma findings, dermoscopy reveals amorphous densely pigmented structures obliterating some follicular openings.[16 ]
Histologic Findings
Skin
biopsy samples with hematoxylin and eosin staining reveal yellowish
brown – pigmented bodies in the dermis that represent altered widened
elastic fibers, as well as in macrophages, endothelial cells, apocrine
glands, and epidermal basement membranes. The deposits do not lose their
pigmentation after 3 days in 10% hydrogen peroxide. Furthermore, the
ochronotic pigment reacts with all routine stains for melanin. Such
deposits can also be seen in cartilage and elastic tissue.
Exogenous ochronosis reveals ochronotic collagen fibers leading to the formation of ochronotic colloid milium.[17 ]The
dermal cell infiltrate is variable but often granulomatous.
Transfollicular elimination of these ochronotic fibers has been
reported.
Note the images below.
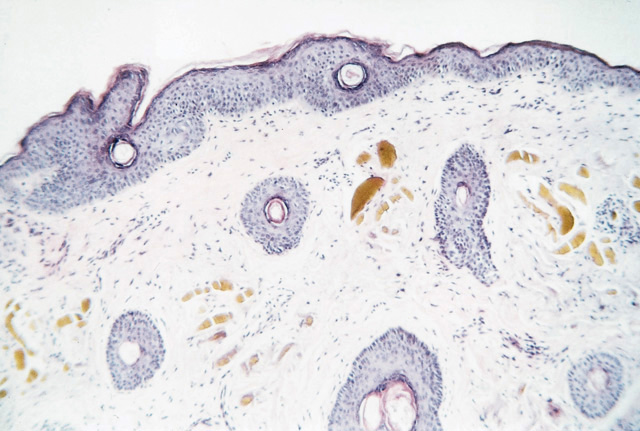
Upon microscopic examination, amber-colored, oval structures are detected in the mid-to-upper dermal tissues (hematoxylin and eosin, original magnification X40).
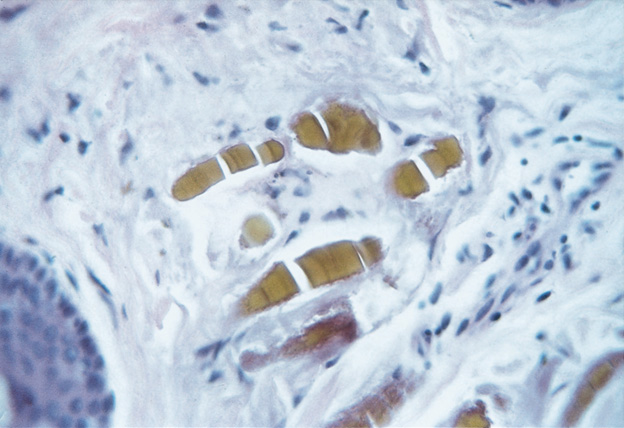
Upon higher magnification (of Image 3), ochronosis reveals homogenization and swelling of collagen bundles (hematoxylin and eosin, original magnification X100).
Treatment
Medical Care
Although
no present medical treatment is available for alkaptonuria, genetic
advances offer hope that corrective measures are forthcoming. Some have
advocated diets low in tyrosine and phenylalanine, thereby reducing the
toxic byproduct homogentisic acid (HGA). Additionally, a diet high in
vitamin C might prevent oxidation of homogentisic acid. Dietary changes
have been advocated by some authors.[18 ]
One possible hope is that nitisinone proves effective.[19 ]The
US Food and Drug Administration (FDA) has approved this drug for the
treatment of tyrosinemia type 1. It significantly lowers the urinary
excretion of HGA by inhibiting 4-hydrophenylpyruvate dioxygenase and,
thoracally, would reduce HGA accumulation. Testing presently is
assessing safety and long-term results.
Ochronotic arthropathy is treated with physiotherapy, analgesia, rest, and prosthetic joint replacement when necessary.
Also
see the clinical trials, Study of Alkaptonuria (recruiting)
and Long-Term Study of Nitisinone to Treat Alkaptonuria (completed).
Surgical Care
With exogenous cutaneous ochronosis induced by topical hydroquinones, carbon dioxide lasers and dermabrasion have been reported to be helpful.[20,21 ]Reports have described effective therapy with the Q-switched alexandrite 755-nm laser.[22 ]
Consultations
- Consultations with a rheumatologist for the arthropathies that develop should be considered.
- An expert in medical genetics may be of assistance in screening families for this autosomal recessive metabolic disorder.
- A cardiac assessment and follow-up care are needed upon entering the fourth decade of life.
Activity
Activities are restricted in adult life because of arthritic complaints.
Medication
At the present state of knowledge, no medical therapy for ochronosis and alkaptonuria is available. The FDA has approved this drug for the treatment of tyrosinemia type 1. It significantly lowers the urinary excretion of HGA by inhibiting 4-hydrophenylpyruvate dioxygenase and, thoracally, would reduce HGA accumulation. Testing presently is assessing safety and long-term results.
Follow-up
Further Outpatient Care
- Patients with alkaptonuria need cardiovascular follow-up care upon entering their fourth decade of life.
Complications
- Complications of alkaptonuria include arthropathy and possible cardiovascular disease (see Mortality/Morbidity).
Prognosis
- Patients with alkaptonuria can expect a normal life span; nevertheless, the complications of debilitating arthritis, cardiovascular compromise, and ochronotic skin alterations will occur.
Patient Education
- Patients with alkaptonuria need to know that they will have a normal life span, despite pigmentary alterations and arthritis that materialize in mid life.
- Patients need cardiovascular follow-up care in their later years.
References
-
Felbor U, Mutsch Y, Grehn F, Müller CR, Kress W. Ocular ochronosis in alkaptonuria patients carrying mutations in the homogentisate 1,2-dioxygenase gene. Br J Ophthalmol. Jun 1999;83(6):680-3. [Medline].
-
Zhao BH, Chen BC, Shao de C, Zhang Q. Osteoarthritis? Ochronotic arthritis! A case study and review of the literature. Knee Surg Sports Traumatol Arthrosc. Jul 2009;17(7):778-81. [Medline].
-
Gurkanlar D, Daneyemez M, Solmaz I, Temiz C. Ochronosis and lumbar disc herniation. Acta Neurochir (Wien). Aug 2006;148(8):891-4; discussion 894. [Medline].
-
Butany JW, Naseemuddin A, Moshkowitz Y, Nair V. Ochronosis and aortic valve stenosis. J Card Surg. Mar-Apr 2006;21(2):182-4. [Medline].
-
Yoshikai M, Murayama J, Yamada N. Aortic valve regurgitation in alkaptonuria. J Heart Valve Dis. Sep 2004;13(5):863-5. [Medline].
-
Vilboux T, Kayser M, Introne W, et al. Mutation spectrum of homogentisic acid oxidase (HGD) in alkaptonuria. Hum Mutat. Dec 2009;30(12):1611-9. [Medline].
-
Bruce S, Tschen JA, Chow D. Exogenous ochronosis resulting from quinine injections. J Am Acad Dermatol. Aug 1986;15(2 Pt 2):357-61. [Medline].
-
Bongiorno MR, Aricò M. Exogenous ochronosis and striae atrophicae following the use of bleaching creams. Int J Dermatol. Feb 2005;44(2):112-5. [Medline].
-
Findlay GH, Morrison JG, Simson IW. Exogenous ochronosis and pigmented colloid milium from hydroquinone bleaching creams. Br J Dermatol. Dec 1975;93(6):613-22. [Medline].
-
Hoshaw RA, Zimmerman KG, Menter A. Ochronosislike pigmentation from hydroquinone bleaching creams in American blacks. Arch Dermatol. Jan 1985;121(1):105-8. [Medline].
-
Zawar VP, Mhaskar ST. Exogenous ochronosis following hydroquinone for melasma. J Cosmet Dermatol. Dec 2004;3(4):234-6. [Medline].
-
Balaban B, Taskaynatan M, Yasar E, Tan K, Kalyon T. Ochronotic spondyloarthropathy: spinal involvement resembling ankylosing spondylitis. Clin Rheumatol. Jul 2006;25(4):598-601. [Medline].
-
Koçyigit H, Gürgan A, Terzioglu R, Gürgan U. Clinical, radiographic and echocardiographic findings in a patient with ochronosis. Clin Rheumatol. 1998;17(5):403-6. [Medline].
-
Perrone A, Impara L, Bruni A, Primicerio P, Marini M. Radiographic and MRI findings in ochronosis. Radiol Med. Oct 2005;110(4):349-58. [Medline].
-
Cortes Hernandez J, Ruiz-Oliva Ruiz F, Alonso Colmenares JI, Alvarez Ruiz S, Caton Santaren B, Alcorta Armentia MP. [Ochronotic arthropathy: the value of bone scintigraphy in alkaptonuria]. Rev Esp Med Nucl. May-Jun 2004;23(3):189-92. [Medline].
-
Charlin R, Barcaui CB, Kac BK, Soares DB, Rabello-Fonseca R, Azulay-Abulafia L. Hydroquinone-induced exogenous ochronosis: a report of four cases and usefulness of dermoscopy. Int J Dermatol. Jan 2008;47(1):19-23. [Medline].
-
Gonul M, Cakmak SK, Kilic A, Gul U, Heper AO. Pigmented coalescing papules on the dorsa of the hands: pigmented colloid milium associated with exogenous ochronosis. J Dermatol. Apr 2006;33(4):287-90. [Medline].
-
Turgay E, Canat D, Gurel MS, Yuksel T, Baran MF, Demirkesen C. Endogenous ochronosis. Clin Exp Dermatol. Dec 2009;34(8):e865-8. [Medline].
-
Suwannarat P, O'Brien K, Perry MB, Sebring N, Bernardini I, Kaiser-Kupfer MI, et al. Use of nitisinone in patients with alkaptonuria. Metabolism. Jun 2005;54(6):719-28. [Medline].
-
Diven DG, Smith EB, Pupo RA, Lee M. Hydroquinone-induced localized exogenous ochronosis treated with dermabrasion and CO2 laser. J Dermatol Surg Oncol. Nov 1990;16(11):1018-22. [Medline].
-
Lang PG Jr. Probable coexisting exogenous ochronosis and mercurial pigmentation managed by dermabrasion. J Am Acad Dermatol. Nov 1988;19(5 Pt 2):942-6. [Medline].
-
Bellew SG, Alster TS. Treatment of exogenous ochronosis with a Q-switched alexandrite (755 nm) laser. Dermatol Surg. Apr 2004;30(4 Pt 1):555-8. [Medline].
-
Fernandez-Canon JM, Granadino B, Beltran-Valero de Bernabe D, et al. The molecular basis of alkaptonuria. Nat Genet. Sep 1996;14(1):19-24. [Medline].
-
Garcia SF, Egbert B, Swetter SM. Hereditary ochronosis: hyperpigmented skin overlying cartilaginous structures. Cutis. Jun 1999;63(6):337-8. [Medline].
-
Hardwick N, Van Gelder LW, Van der Merwe CA, Van der Merwe MP. Exogenous ochronosis: an epidemiological study. Br J Dermatol. Feb 1989;120(2):229-38. [Medline].
-
Huerta Brogeras M, Sánchez-Viera M. Exogenous ochronosis. J Drugs Dermatol. Jan 2006;5(1):80-1. [Medline].
-
Jordaan HF, Van Niekerk DJ. Transepidermal elimination in exogenous ochronosis. A report of two cases. Am J Dermatopathol. Aug 1991;13(4):418-24. [Medline].
-
Keller JM, Macaulay W, Nercessian OA, Jaffe IA. New developments in ochronosis: review of the literature. Rheumatol Int. Mar 2005;25(2):81-5. [Medline].
-
Lawrence N, Bligard CA, Reed R, Perret WJ. Exogenous ochronosis in the United States. J Am Acad Dermatol. May 1988;18(5 Pt 2):1207-11. [Medline].
-
Mannoni A, Selvi E, Lorenzini S, et al. Alkaptonuria, ochronosis, and ochronotic arthropathy. Semin Arthritis Rheum. Feb 2004;33(4):239-48. [Medline].
-
Martin RF, Sanchez JL, Gonzalez A, Lugo-Somolinos A, Ruiz H. Exogenous ochronosis. P R Health Sci J. Apr 1992;11(1):23-6. [Medline].
-
O'Brien WM. Biochemical, pathologic and clinical aspects of alkaptonuria, ochronosis and ochronotic arthropathy. Am J Med. 1963;34:813-9.
-
Suzuki Y, Oda K, Yoshikawa Y, Maeda Y, Suzuki T. A novel therapeutic trial of homogentisic aciduria in a murine model of alkaptonuria. J Hum Genet. 1999;44(2):79-84. [Medline].
Keywords
ochronosis, alkaptonuria, bluish black discoloration of tissue, exogenous ochronosis, exposure to hydroquinone, homogentisic acid oxidase, homogentisic acid, HGA





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 