
US Pharm. 2013;38(3):33-41.
ABSTRACT: Gallbladder disease, particularly cholelithiasis (gallstones), affects more than 20 million Americans each year. Patients often go undiagnosed because cholelithiasis often does not present with symptoms. Symptoms range from nausea or abdominal discomfort to biliary colic and jaundice. Gallbladder diseases are diagnosed most accurately via imaging techniques. However, laboratory values such as CBC, liver-function testing, and serum amylase and lipase should be included to help distinguish the type of gallbladder disease and/or identify associated complications. The most effective treatment for patients with gallbladder disease is surgery. Gallbladder disease is influenced by diet, exercise, and nutrition, and patients should be encouraged to incorporate these healthy habits into their lifestyle in order to reduce their risk of gallbladder disorders.
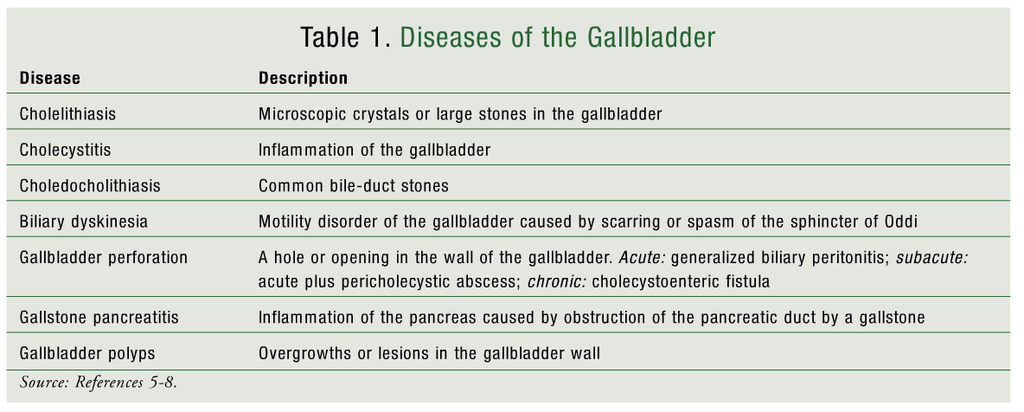
The most common form of gallbladder disease is cholelithiasis (gallstones).1 Cholelithiasis affects more than 20 million Americans annually, resulting in a direct cost of more than $6.3 billion.2 Gallstones generally are asymptomatic and typically are discovered during a surgical procedure for an unrelated condition or during autopsy.1,2 In the United States, cholelithiasis is the most common inpatient diagnosis among gastrointestinal and liver diseases.3,4 Although gallstones are usually asymptomatic, some patients progress to symptomatic disease. The primary clinical manifestation and complication of cholelithiasis is cholecystitis (inflammation of the gallbladder).1,2 Less commonly, patients with severe cases may develop gallstone pancreatitis, gallbladder perforation, or other gallbladder diseases (TABLE 1).1,5-8
Pathophysiology
Gallstones are hard, pebble-like structures that obstruct the cystic duct. The formation of gallstones is often preceded by the presence of biliary sludge, a viscous mixture of glycoproteins, calcium deposits, and cholesterol crystals in the gallbladder or biliary ducts.5 In the U.S., most gallstones consist largely of bile supersaturated with cholesterol.1,2 This hypersaturation, which results from the cholesterol concentration being greater than its solubility percentage, is caused primarily by hypersecretion of cholesterol due to altered hepatic cholesterol metabolism.1,3 A distorted balance between pronucleating (crystallization-promoting) and antinucleating (crystallization-inhibiting) proteins in the bile also can accelerate crystallization of cholesterol in the bile.1-3,5 Mucin, a glycoprotein mixture secreted by biliary epithelial cells, has been documented as a pronucleating protein. It is the decreased degradation of mucin by lysosomal enzymes that is believed to promote the formation of cholesterol crystals.3
Loss of gallbladder muscular-wall motility and excessive sphincteric contraction also are involved in gallstone formation.1 This hypomotility leads to prolonged bile stasis (delayed gallbladder emptying), along with decreased reservoir function.3,5 The lack of bile flow causes an accumulation of bile and an increased predisposition for stone formation. Ineffective filling and a higher proportion of hepatic bile diverted from the gallbladder to the small bile duct can occur as a result of hypomotility.1,5
Occasionally, gallstones are composed of bilirubin, a chemical that is produced as a result of the standard breakdown of RBCs. Infection of the biliary tract and increased enterohepatic cycling of bilirubin are the suggested causes of bilirubin stone formation. Bilirubin stones, often referred to as pigment stones, are seen primarily in patients with infections of the biliary tract or chronic hemolytic diseases (or damaged RBCs).1,3,6 Pigment stones are more frequent in Asia and Africa.3,6
The pathogenesis of cholecystitis most commonly involves the impaction of gallstones in the bladder neck, Hartmann’s pouch, or the cystic duct; gallstones are not always present in cholecystitis, however.5 Pressure on the gallbladder increases, the organ becomes enlarged, the walls thicken, the blood supply decreases, and an exudate may form.2,5 Cholecystitis can be either acute or chronic, with repeated episodes of acute inflammation potentially leading to chronic cholecystitis. The gallbladder can become infected by various microorganisms, including those that are gas forming. An inflamed gallbladder can undergo necrosis and gangrene and, if left untreated, may progress to symptomatic sepsis.1,2,5 Failure to properly treat cholecystitis may result in perforation of the gallbladder, a rare but life-threatening phenomenon.2,5,7 Cholecystitis also can lead to gallstone pancreatitis if stones dislodge down to the sphincter of Oddi and are not cleared, thus blocking the pancreatic duct.1
Risk Factors
Genetic and environmental factors contribute to gallbladder disease. Female gender, previous pregnancies, and family history of gallstone disease are highly correlated with cholelithiasis.1,3 Approximately 60% of patients with acute cholecystitis are women; however, the disease tends to be more severe in men.2 Estrogen increases cholesterol and its saturation in bile and promotes gallbladder hypomotility.1 Diminished gallbladder motility is commonly seen during pregnancy.9
Other risk factors include a high dietary intake of fats and carbohydrates, a sedentary lifestyle, type 2 diabetes mellitus, and dyslipidemia (increased triglycerides and low HDL).3,9 A diet high in fats and carbohydrates predisposes a patient to obesity, which increases cholesterol synthesis, biliary secretion of cholesterol, and cholesterol hypersaturation. However, a direct correlation between high dietary intake of fats and cholelithiasis risk has not been established because previous studies have yielded controversial results.9 Acute cholecystitis develops more frequently in symptomatic cholelithiasis patients with type 2 diabetes mellitus than in symptomatic patients without it.2 These patients also are more likely to have complications.
American Indians have the highest prevalence of cholelithiasis, with the disease reaching epidemic proportions in this population. Gallstone disease is also prevalent in Chilean and Mexican Hispanics.3,9 In addition to ethnicity, age plays a role in gallstone disease. Patients who develop complicated symptomatic cholelithiasis tend to be older, and the typical patient with gallstones is in her 40s.1,2
Clinical Presentation
Gallstones are generally asymptomatic. In the uncommon event that a patient develops symptomatic cholelithiasis, presentation can range from mild nausea or abdominal discomfort to biliary colic and jaundice.1,5,10 Biliary colic, usually sharp in nature, is postprandial epigastric or right-quadrant pain that lasts for several minutes to several hours. The pain often radiates to the back or the right shoulder, and in more intense cases it may be accompanied by nausea and vomiting. Upper-right-quadrant tenderness and palpable infiltrate in the region of the gallbladder are revealed upon physical examination.5,10 Cholecystitis presents in the same manner; however, the obstruction of the cystic duct is persistent (rather than transient), and fever is common.10 A patient with cholecystitis also may exhibit Murphy’s sign (discomfort so severe that the patient stops inspiring during palpation of the gallbladder) or jaundice. Jaundice, a yellow discoloration of the skin and the sclera of the eyes, occurs when the common bile duct is obstructed because of an impacted stone in Hartmann’s pouch (Mirizzi’s syndrome). Other nonspecific symptoms, such as indigestion, intolerance to fatty or fried foods, belching, and flatulence, may also be present.1,5,10
Diagnosis
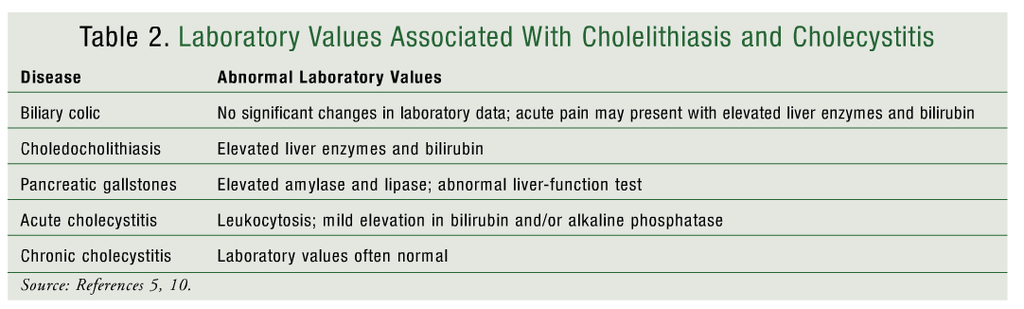
Current techniques for diagnosing gallbladder disease are less invasive and allow patients to recover more quickly than was the case with earlier diagnostic procedures.10 Although the incidence of cholelithiasis is quite high in the U.S., few patients present with symptoms.4 This can complicate and prolong the diagnosis. CBC, liver-function testing, and serum amylase and lipase should be included in the laboratory tests to help discriminate between the various types of gallbladder disease and/or identify complications caused by gallbladder disease (TABLE 2).5,10
The diagnosis of cholelithiasis, cholecystitis, and other gallbladder diseases can be confirmed via a number of different imaging techniques. Ultrasonography and cholescintigraphy are the imaging studies most commonly used to diagnose cholelithiasis and cholecystitis.10 Positive findings upon ultrasonography include stones, thickening of the gallbladder wall, pericholecystic fluid, and Murphy’s sign (i.e., pain) upon contact with the ultrasonographic probe.10 Ultrasonography performed in the fasting state reveals the correct diagnosis in more than 90% of cases, but bile-duct stones may be missed in 50% of cases.3
Cholescintigraphy, also called hepatobiliary iminodiacetic acid (HIDA) scan, is used to assess the function of the gallbladder and to diagnose acute cholecystitis. HIDA scans are not helpful in identifying cholelithiasis or chronic cholecystitis.11 In ambulatory patients, cholescintigraphy provides a correct diagnosis more than 95% of the time. However, cholescintigraphy may produce false-positive results in 30% to 40% of hospitalized patients, particularly those receiving parenteral nutrition. Ultrasonography is the preferred diagnostic method in these patients.10 Cholescintigraphy results are considered abnormal when the radioactive tracer or dye does not visualize the gallbladder, moves slowly through the bile ducts, or is detected outside the biliary system.12
If choledocholithiasis is suspected, endoscopic retrograde cholangiopancreatography (ERCP) may be beneficial. ERCP is used to identify common bile-duct stones and also may be used to remove them. ERCP is associated with complications such as pancreatitis. Noninvasive techniques, such as endoscopic ultrasonography, may be used to detect cholelithiasis, but not to remove the stones.4,11 CT may be used, but it is considered less accurate than other imaging methods, as it detects approximately 75% of gallstones.4,10 Magnetic resonance cholangiopancreatography (MRCP) is an imaging method used to detect choledocholithiasis and other abnormalities of the biliary tract. MRCP has a sensitivity of approximately 98%.4,11
Treatment
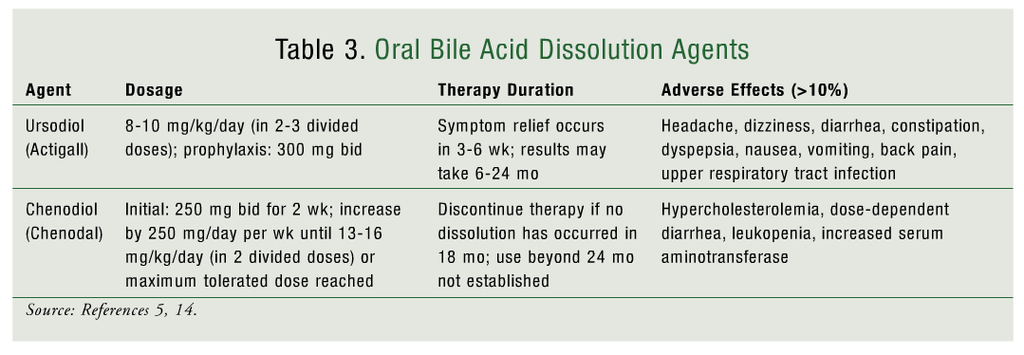
Patients experiencing asymptomatic cholelithiasis do not require treatment.5 The treatment of choice for symptomatic cholelithiasis currently is laparoscopic cholecystectomy, whereas previously it was open cholecystectomy.3,10 Laparoscopic cholecystectomy is associated with a shorter hospital stay and a faster recovery period than open cholecystectomy is. Absolute contraindications to this procedure include the inability to withstand general anesthesia, an intractable bleeding disorder, and end-stage liver disease.3,5 In patients who are unable or unwilling to undergo surgery, endoscopic decompression by internal gallbladder stent can help prevent complications from developing and can serve as palliative long-term treatment.5 Nonoperative therapy, which includes dissolution of gallstones using oral bile acids and shock wave lithotripsy, may be another option in such patients. However, nonoperative therapy is time consuming and is associated with high cost, low effectiveness, and a high recurrence rate.5,13
Oral bile acids used for the dissolution of gallstones include chenodeoxycholic acid (chenodiol) and ursodeoxycholic acid (ursodiol) (TABLE 3).5,14 Oral bile acids are most effective for small gallstones (0.5-1 cm) and may take up to 24 months to clear the stones. Ursodiol is the most commonly used oral bile acid, secondary to its safer side-effect profile compared with chenodiol. Chenodiol is associated with dose-dependent diarrhea as well as with hepatotoxicity, hypercholesterolemia, and leukopenia, all of which limit its use.14
Nutrition and lifestyle changes may be beneficial for the prevention and treatment of cholelithiasis. Because obesity is associated with an increased risk of cholelithiasis, weight loss may help prevent gallstone formation.15 However, excessively rapid weight loss may promote gallstone formation. Dietary factors that may help prevent gallstone formation include polyunsaturated fat, monounsaturated fat, fiber, and caffeine.15 Fish oil and moderate alcohol consumption have been shown to lower triglycerides, lessen bile cholesterol saturation, and increase HDL.3,9
Patients with acute cholecystitis require hospitalization for complete bowel rest, parenteral fluids and nutrition, and IV antibiotics.5Surgical treatment options for cholecystitis include percutaneous cholecystostomy, open cholecystostomy, and laparoscopic cholecystostomy.10
Conclusion
Gallbladder diseases are most commonly secondary to cholelithiasis. While most cases of gallstones are asymptomatic, some cases may progress to a symptomatic disease. Factors that may increase the risk or susceptibility to gallbladder disease include gender, ethnicity, medical history, family history, and diet and nutrition. Gallbladder disease is diagnosed primarily via imaging techniques. These diagnostic techniques have their pros and cons, and, most important, their accuracy varies. One technique may be preferred over another depending upon the type of gallbladder disease or the presenting symptoms. Asymptomatic patients generally do not require treatment. Surgery is the most common treatment, but nonsurgical alternatives are available for patients who cannot or are unwilling to undergo surgery. Pharmacists can play a role in the treatment of gallbladder disease by educating patients about the risk factors for gallbladder disease—particularly cholelithiasis—and about how the risk can be reduced with proper nutrition, diet, and exercise.
REFERENCES
1. Mills JC, Stappenbeck TS, Bunnett NW. Gastrointestinal disease. In: McPhee SJ, Hammer GD, eds. Pathophysiology of Disease: An Introduction to Clinical Medicine. 6th ed. New York, NY: McGraw-Hill Medical; 2010.
2. Strasberg SM. Acute calculous cholecystitis. N Engl J Med. 2008;358:2804-2811.
3. Marschall HU, Einarsson C. Gallstone disease. J Intern Med. 2007;261:529-542.
4. Bar-Meir S. Gallstones: prevalence, diagnosis and treatment. Isr Med Assoc J. 2001;3:111-113.
5. Kalloo AN, Kantsevoy SV. Gallstones and biliary disease. Prim Care. 2001;28:591-606.
6. Choi Y, Silverman WB. Biliary tract disorders, gallbladder disorders and gallstone pancreatitis. American College of Gastroenterology. http://patients.gi.org/topics/biliary-tract-disorders-gallbladder-disorders-and-gallstone-pancreatitis. Accessed October 27, 2012.
7. Derici H, Kara C, Bozdag AD, et al. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006;12:7832-7836.
8. Myers RP, Shaffer EA, Beck PL. Gallbladder polyps: epidemiology, natural history and management. Can J Gastroenterol. 2002;16:187-194.
9. Cuevas A, Miquel JF, Reyes MS, et al. Diet as a risk factor for cholesterol gallstone disease. J Am Coll Nutr. 2004;23:187-196.
10. Vogt DP. Gallbladder disease: an update on diagnosis and treatment. Cleve Clin J Med. 2002;69:977-984.
11. University of Maryland Medical Center. Gallstones and gallbladder disease. www.umm.edu/patiented/articles/what_gallstones_gallbladder_disease_000010_1.htm. Accessed November 27, 2012.
12. Mayo Clinic. HIDA scan. www.mayoclinic.com/health/hida-scan/MY00320/DSECTION=results. Accessed November 27, 2012.
13. Ahmed A, Cheung RC, Keeffe EB. Management of gallstones and their complications. Am Fam Physician. 2000;61:1673-1680.
14. Nunes D. Dissolution therapy for the treatment of gallstones. UpToDate [by subscription]. www.uptodate.com/contents/dissolution-therapy-for-the-treatment-of-gallstones. Accessed February 4, 2013.
15. Gaby AR. Nutritional approaches to prevention and treatment of gallstones. Altern Med Rev. 2009;14:258-267.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 