JAMA.
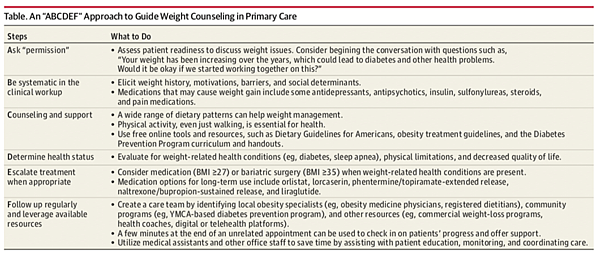
An “ABCDEF” Approach to Guide Weight Counseling in Primary Care
|
Steps 步驟 |
What to Do 作法 |
|
Ask “permission” 徵得同意 |
•Assess patient readiness to discuss weight issues. Consider begining the conversation with questions such as, “Your weight has been increasing over the years, which could lead to diabetes and other health problems. Would it be okay if we started working together on this?” 評估患者討論體重問題的準備情況。可以考慮從 "多年來你的體重一直在增加, 這可能導致糖尿病和其他健康問題" 等問題開始。如果我們開始合作可以嗎? " |
|
Be systematic in the clinical workup 系統化臨床工作 |
•Elicit weight history, motivations, barriers, and social determinants. 了解減重歷史、動機、阻礙與社會決定因素 •Medications that may cause weight gain include some antidepressants, antipsychotics, insulin, sulfonylureas, steroids, and pain medications. 找出可能導致體重增加的藥物包括一些抗憂鬱藥、抗精神病藥、胰島素、磺脲、類固醇、和止痛藥。 |
|
Counseling and support 諮詢與協助 |
• A wide range of dietary patterns can help weight management. 廣泛的飲食模式有助於體重控制 • Physical activity, even just walking, is essential for health. 體能活動,就算是健走都有助於健康 • Use free online tools and resources, such as Dietary Guidelines for Americans, obesity treatment guidelines, and the Diabetes Prevention Program curriculum and handouts. 使用一些線上工具還有資源,例如飲食準則、肥胖治療準則或是糖尿病預防計畫課程和講義 |
|
Determine health status 決定健康狀態 |
• Evaluate for weight-related health conditions (eg, diabetes, sleep apnea), physical limitations, and decreased quality of life. 體重相關的健康狀況,例如糖尿病、睡眠呼吸中止症、體能限制與生活品質的下降 |
|
Escalate treatment when appropriate 適時升級治療 |
• Consider medication (BMI ≥27) or bariatric surgery (BMI ≥35) when weight-related health conditions are present. 但相關的體重健康狀況出現時,可以在BMI ≥27 時進行藥物治療或是BMI ≥35時進行減重手術 • Medication options for long-term use include orlistat, lorcaserin, phentermine/topiramate-extended release,naltrexone/bupropion-sustained release, and liraglutide. 長期藥物的選項包含有orlistat、lorcaserin、phentermine/topiramate-extended release、naltrexone/bupropion-sustained release及liraglutide |
|
Follow up regularly and leverage available resources 定期跟進並利用資源 |
• Create a care team by identifying local obesity specialists (eg, obesity medicine physicians, pharmacist, registered dietitians), community programs (eg, YMCA-based diabetes prevention program), and other resources (eg, commercial weight-loss programs, health coaches, digital or telehealth platforms). 透過一些認證的肥胖專科 (如肥胖醫學醫生、藥師、營養師)、社區專案 (YMCA 的糖尿病預防計畫) 和其他資源 (如商業減肥計畫、健康教練), 建立一個護理團隊、數位或遠端保健平臺)。 • A few minutes at the end of an unrelated appointment can be used to check in on patients’ progress and offer support. 可以在一些預約(或是掛號)之外的時間花幾分鐘與患者討論減重進程並提供幫助 • Utilize medical assistants and other office staff to save time by assisting with patient education, monitoring, and coordinating care. 利用醫療助理和其他辦公室工作人員, 通過協助病人教育、監測和協調護理, 節省時間。 |
This ABCDEF approach, although not formally validated, is based on published guidelines and is meant to be practical and useful for clinicians.
其他全文我就附在下面
A. Ask “permission” before discussing obesity. It may seem awkward to ask patients for permission to discuss a clinical issue, but doing so supports patients’ autonomy and is a respectful and strategic way to broach a sensitive topic. Patients who decline counseling will nonetheless know that they can seek support when they are ready.
B. Be systematic in the clinical workup. Advising patients to “just eat less and exercise more” is unhelpful, especially for patients affected by binge eating disorder, adverse childhood experiences and trauma, medication-induced weight gain, and other common contributors to weight gain. A clinical problem-solving approach should be used, with an eye toward identifying causes and leverage points. Elicit a weight history and explore the patient’s weight trajectory, what has contributed to weight gain, what has or has not worked in the past, and barriers that may get in the way of sustained behavioral changes.
C. Counseling and support improve weight loss perceptions (eg, awareness of weight status, motivation to manage weight) and outcomes (eg, short- and long-term weight loss, improvement in weight-related conditions).2For example, in a trial of 415 patients with cardiovascular risk factors, patients randomized to receive primary care counseling maintained greater weight loss over 2 years, compared with self-directed weight loss (11.2 lb vs 1.7 lb).6 Support motivation by appealing to patients’ interests, values, and preferences. Because current evidence does not define a “best diet,” patients should be counseled on how to strategically decrease energy intake within a dietary pattern that is reasonably appealing and convenient. It remains important to encourage intake of whole foods and minimize ultraprocessed foods and added sugars. Helping patients manage expectations is important; whereas achieving a “normal” weight is unrealistic for many patients, sustained weight loss of 5% to 10% is often achievable and improves health. Then, aiming for additional weight loss and positive behavioral changes over time is still an option.
D. Determine health status. Patients should be evaluated for weight-related health conditions (eg, diabetes, hypertension, sleep apnea, osteoarthritis), disability, and impaired quality of life so that intensity of treatment can be aligned with severity of disease. Obesity treatment is indicated when a patient’s weight affects health, quality of life, or functioning. In contrast, some excess weight beyond normative levels or societal norms in the absence of adverse health effects does not necessarily demand management beyond preventive monitoring.
E. Escalate treatment when appropriate. According to the USPSTF, current evidence is insufficient to recommend pharmacotherapy in healthy individuals, despite elevated weight.5 However, when excess weight is complicated by health risks and if a patient does not achieve enough improvement in weight and health with counseling alone, then obesity medications (BMI ≥27) approved by the US Food and Drug Administration (FDA) or bariatric surgery referral (BMI ≥35) should be considered. Medications and surgery lead to more weight loss and health improvements than behavioral counseling alone. In patients with type 2 diabetes mellitus (T2D), obesity medications combined with counseling improves hemoglobin A1c by 0.5% to 1.6%—as much improvement as with many FDA-approved diabetes medications; for patients at risk of T2D, medications decrease the risk for progression to T2D by as much as 40% to 80% over 2 to 4 years.7 Bariatric surgery improves numerous comorbidities and decreases mortality.8
F. Follow up regularly and leverage available resources. Obesity will not be solved in a single clinic visit, yet only 24% of 3008 patients in a recent survey reported having a follow-up appointment scheduled after an initial weight loss discussion.2 Clinicians should offer support and monitor weight and other metrics, such as changes in waist circumference and weight-related risk factors, as well as subjective improvements in energy, mobility, and chronic pain symptoms. Frequent counseling is essential, but clinicians need not provide this alone. When expertise or time demands exceed the clinician’s capacity, referral of patients to other practitioners or services, such as obesity medicine physicians, registered dietitians, behavioral therapists, commercial or community programs, or digital and telehealth programs, should be considered. Increasingly, these services are becoming more available throughout the United States and many are covered by health plans. A trial involving 1882 patients and 137 primary care physicians in the United Kingdom showed that a basic, 30-second intervention, in which physicians screened patients and offered referral to a community weight loss program, led to more weight loss than in the control group (5.4 lb vs 2.2 lb over 12 months).9





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 