Out-of-hospital cardiac arrest claims hundreds
of thousands of lives each year worldwide.1,2 Successful
resuscitation is challenging but achievable, requiring an interdependent
set of actions that consist of early arrest recognition, early
cardiopulmonary resuscitation (CPR), early defibrillation, expert
advanced life support, and timely postresuscitation care.3
Early initiation of CPR by a layperson can increase the patient's chances of surviving and having a favorable long-term neurologic recovery.4,5 CPR performed by a layperson has traditionally consisted of chest compressions interspersed with rescue breathing, which allows some measure of both circulation and oxygenation.6 Interest in CPR that focuses on chest compressions and minimizes or eliminates rescue breathing is increasing.7 Chest compression alone may be more acceptable to some laypersons and has the potential physiological advantage of fewer compression interruptions, so that circulation is increased, as compared with traditional CPR, although at a possible cost to oxygenation. 8,9
Studies in animal models that involve a primary cardiac cause of arrest and simulate challenges to laypersons performing CPR have shown increased circulation and improved survival with chest compression alone.10,11 In contrast, results in animal models of arrest due to respiratory causes suggest that chest compression plus rescue breathing may be more beneficial.12
Cardiac arrest in humans is a heterogeneous condition. Although a primary cardiac cause is the most common mechanism of arrest, respiratory and mixed mechanisms are important contributing factors.13-15 The pathophysiology of each arrest is dynamic, and the relative importance of oxygenation may depend on the time-dependent phase of the arrest.16 In observational studies of bystander-initiated CPR, the two CPR approaches led to similar survival rates, although interpretation of these findings is limited by potential confounding.14,15 In the only randomized trial comparing these two types of bystander CPR, there was no significant difference in survival between the two groups, although the observed survival difference between patients randomly assigned to chest compression alone and those randomly assigned to compression plus rescue breathing (14.6% vs. 10.4%) is clinically relevant.18 This trial was conducted in a community with a very quick response by emergency medical services (EMS), and the study's main analysis was restricted to patients with a primary cardiac cause of arrest — characteristics that potentially favor the physiological effects of chest compression alone.
To help determine the best approach to bystander CPR, we undertook a randomized trial of dispatcher-assisted CPR to compare outcomes when instructions consisted of chest compression alone with outcomes when instructions consisted of chest compression plus rescue breathing. We hypothesized that instruction consisting of chest compression alone would result in higher survival rates than instruction consisting of chest compression plus rescue breathing.
Methods
Study Design, Population, and Setting
The Dispatcher-Assisted Resuscitation Trial (DART) was a randomized trial of dispatcher-assisted CPR instruction. The study was approved by the appropriate review boards, and patients were enrolled without consent being obtained, although survivors were later informed that they had been enrolled in a clinical investigation of CPR.
The study considered consecutive calls by bystanders to the 911 system for patients in cardiac arrest. Patients were initially eligible if the dispatcher determined that they were unconscious and not breathing normally and that bystander CPR was not under way. If the caller was willing to undertake CPR with the dispatcher's assistance, a randomization envelope containing CPR instructions was opened. Dispatchers attempted to exclude patients with arrest due to trauma, drowning, or asphyxiation (from choking, strangulation, or suffocation), as well as patients who were under 18 years of age; and those who had do-not-resuscitate status or were already receiving CPR. Final eligibility required postrandomization exclusion and was restricted to patients who received basic and advanced arrest care from EMS personnel. Thus, we excluded persons who were unconscious and not breathing normally but who were deemed not to be in arrest and persons who had had a confirmed arrest but were found to have signs of irreversible death, in which case EMS personnel did not attempt resuscitation.19
King County EMS (in Washington State), Thurston County EMS (in Washington State), and London Ambulance Service (in England) participated in the trial. At all three sites, callers use a common emergency number to speak with civilian employee dispatchers. King and Thurston Counties are served by a two-tiered EMS system in which personnel follow the core resuscitation strategy detailed by the American Heart Association guidelines. London is served by a single-tier EMS system in which personnel follow the United Kingdom Resuscitation Council Guidelines. Because of differences in enrollment rates and time required for review processes, enrollment took place from June 1, 2004, through April 15, 2009, in King County; from June 1, 2005, through April 15, 2009, in Thurston County; and from January 1, 2005, through March 15, 2008, in London.
Intervention
On determining patients' initial eligibility, dispatchers enrolled and randomly assigned each patient to one of the two CPR strategies by opening an opaque, sequentially numbered envelope to determine which instructions to give the bystander. Randomization was stratified by dispatch center and blocked in sets of 10. The bystander was then instructed to perform either chest compressions alone, providing 50 consecutive compressions (one cycle), or chest compressions plus rescue breathing, with 2 initial rescue breaths followed by 15 chest compressions and subsequent cycles continuing the pattern in a ratio of 2 to 15 (see Fig. 1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). With the dispatcher still on the telephone, the bystander then performed one cycle of CPR during which the dispatcher asked the bystander to count the chest compressions out loud. After the first cycle, the dispatcher could inquire about signs of life and, if warranted, encourage the bystander to continue CPR.
Outcomes
The primary outcome was survival to hospital discharge. Secondary outcomes were a return of spontaneous circulation at the end of EMS care and a favorable neurologic status at the time of hospital discharge, defined as a Cerebral Performance Category (CPC) of 1 or 2. (There are five CPC categories; category 1 represents good cerebral performance, 2 moderate cerebral disability, 3 severe cerebral disability, 4 coma or vegetative state, and 5 death.20,21)
Data Collection and Definitions
Dispatch, EMS, and hospital information was reviewed with the use of a uniform data-abstraction form.21 The review of EMS and hospital information was done without knowledge of patients' randomization status. Step-by-step progress in the provision of instructions and the initiation of chest compressions by the bystander was determined by a review of the dispatch audiotape.
Statistical Analysis
The trial was designed to detect an absolute difference of 3.5 percentage points in the survival rates between the two study groups, with the use of a two-sided alpha level of 0.05 and a power of 80%. To compare the distribution of characteristics and outcomes for the two types of CPR instruction, we used the chi-square statistic for categorical variables and the independent-samples t-test or the nonparametric Mann–Whitney U test for continuous variables. Primary comparisons were performed according to randomization status. We also performed an efficacy analysis restricted to cases in which bystander CPR progressed to chest compression as a consequence of dispatcher instructions. Because one site was unable to assess neurologic status at discharge, we present the overall results as well as results restricted to the two sites that were able to ascertain neurologic status.
We conducted four prespecified subgroup analyses designed to examine the physiological mechanisms of the intervention as well as to provide a context for interpreting the results in relation to other investigations. The subgroup analyses stratified outcomes according to the underlying cause of arrest, presenting arrest rhythm, witness status, and EMS response interval among witnessed arrests (≤6 minutes vs. >6 minutes). No other subgroup analyses were performed. We used the Breslow–Day test for homogeneity to determine whether the intervention differed according to subgroup status. Statistical analyses were completed with the use of SPSS software, version 18.0 (SPSS).
The study was conducted according to the protocol. The funding organizations did not have a role in the study design, conduct of the study, or interpretation of the results.
Results
Patients, Arrests, and Progression of CPR Instructions
During the course of the trial, 5525 randomization envelopes were opened for patients presumed to be in cardiac arrest. Of these patients, 1941 (35%) met the inclusion criteria (Figure 1 Figure 1Enrollment, CPR Status, and Eligibility.). The two most common reasons for exclusion were that EMS personnel found the patient to be alive without arrest or to have signs of irreversible death (in which case resuscitation by EMS was not attempted). The distribution of exclusions in the two groups was similar according to randomization status.
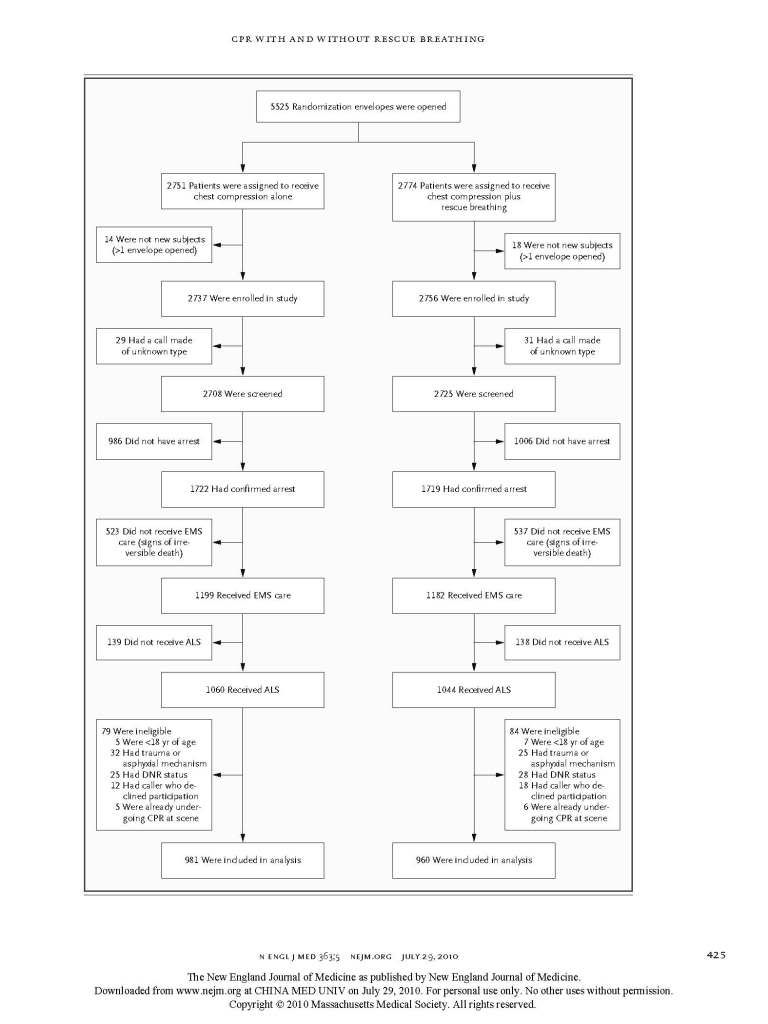
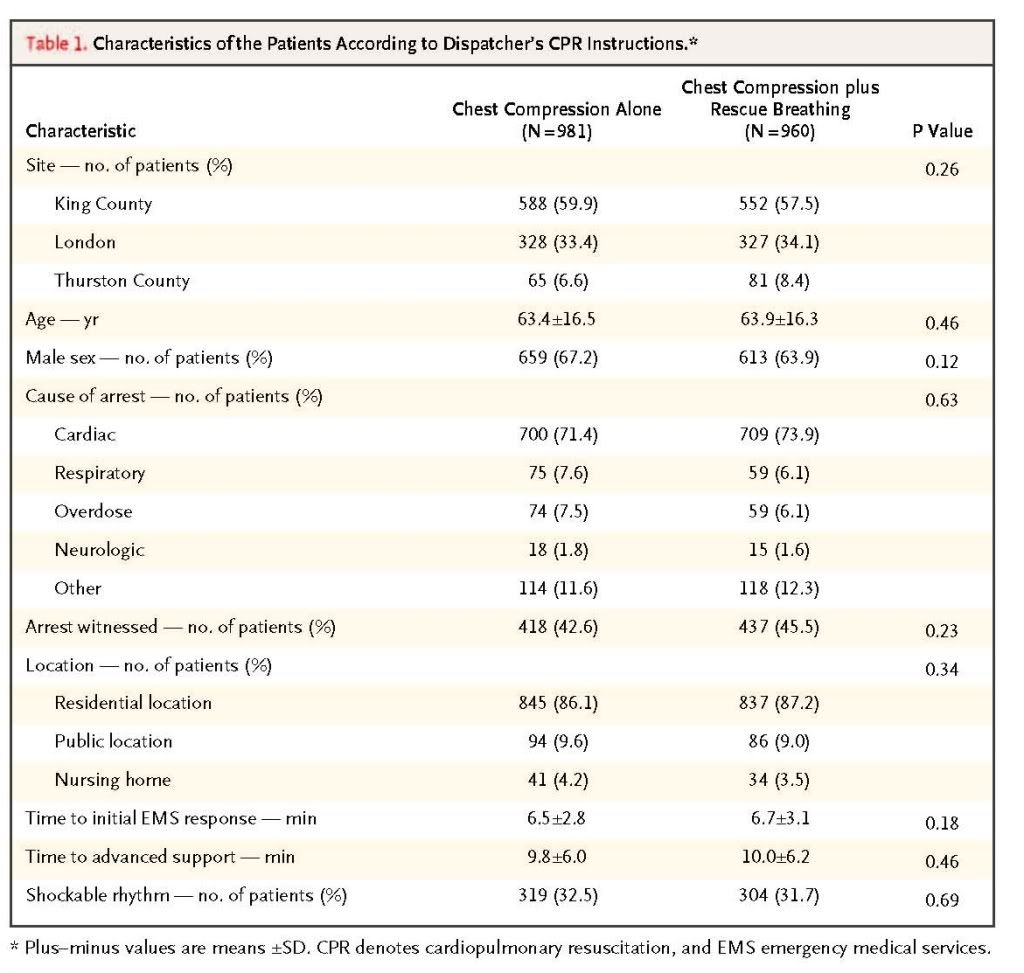
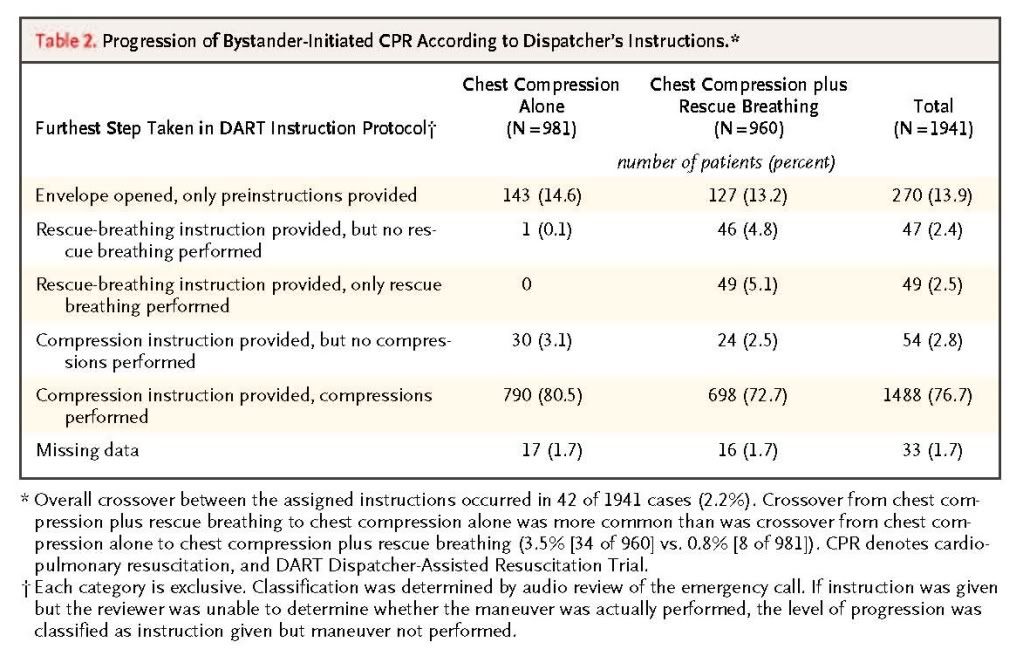
Among the 1941 eligible patients, approximately 70% had arrests with a cardiac cause, less than half the arrests were witnessed, and nearly a third had a shockable rhythm. The average EMS response time from dispatch to arrival at the scene was 6.5 minutes. Patients, circumstance, EMS response, and presenting rhythm characteristics were similar in the two groups (Table 1 Table 1Characteristics of the Patients According to Dispatcher's CPR Instructions.). Patients randomly assigned to instructions for the bystander to perform chest compression alone were more likely to undergo bystander-performed chest compression (80.5% vs. 72.7%, P<0.001)
(Table 2Table 2 Progression of Bystander-Initiated CPR According to Dispatcher's Instructions.).
Survival to Discharge
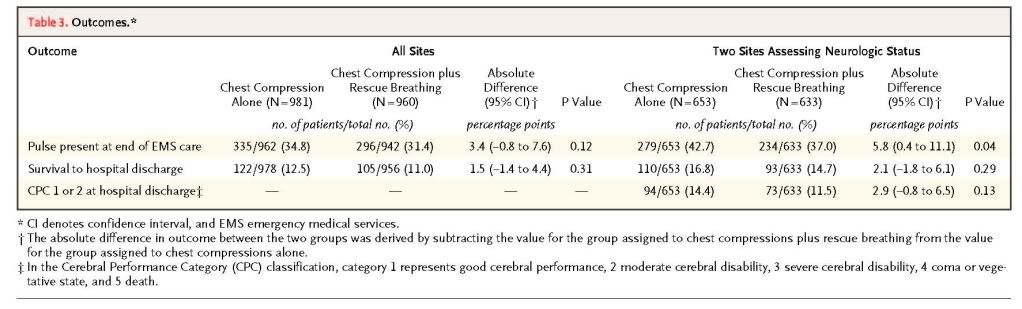
Survival to hospital discharge could not be ascertained for seven subjects (0.4%), three randomly assigned to chest compression alone and four to chest compression plus rescue breathing. We observed no significant difference in the proportion of patients surviving to hospital discharge according to randomization status (12.5% for instructions to perform chest compression alone and 11.0% for instructions to perform chest compression plus rescue breathing, P=0.31) or the proportion surviving to discharge with a favorable neurologic status (14.4% for chest compression alone and 11.5% for chest compression plus rescue breathing, P=0.13)
(Table 3Table 3 Outcomes.).
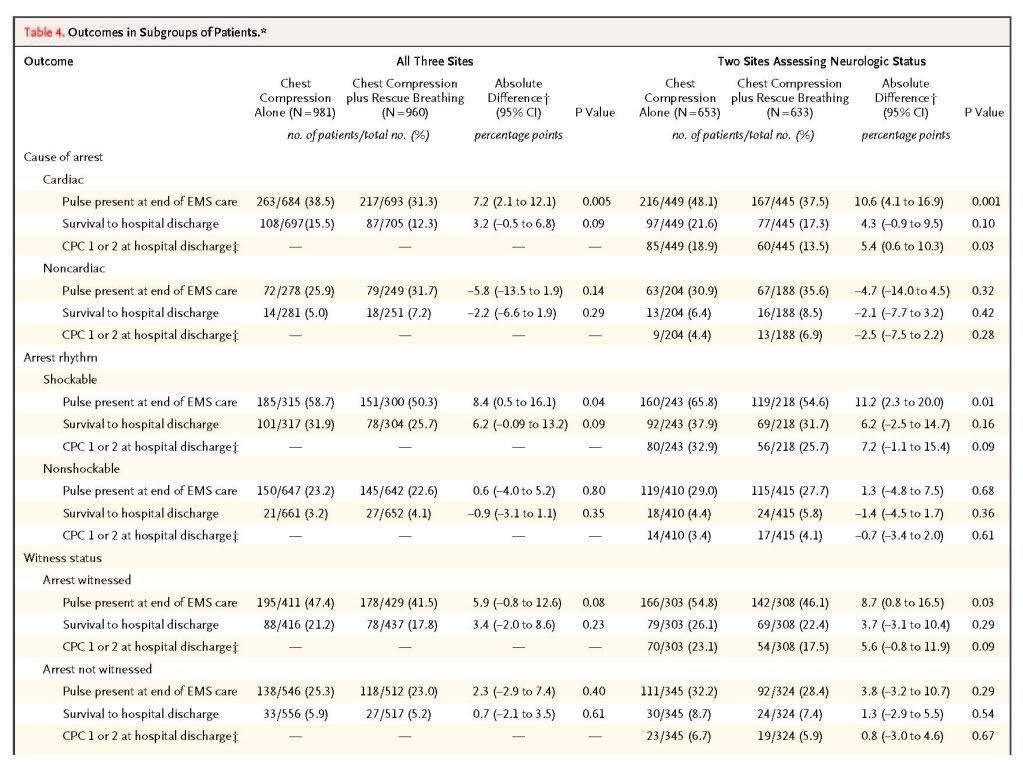
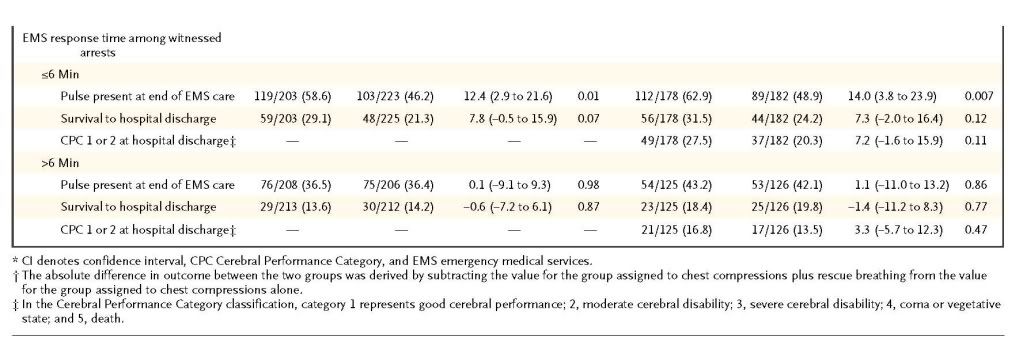
Subgroup Analyses
The Breslow–Day test showed some evidence that the effect of the two sets of CPR instructions on outcomes differed according to the underlying cause of arrest (P=0.007 for return of pulse, P=0.10 for survival to discharge, and P=0.06 for survival with a favorable neurologic status) and presenting arrest rhythm (P=0.14, P=0.09, and P=0.20, respectively). (Tests for heterogeneity showed no evidence that the outcome differed according to whether the arrest was witnessed [P>0.20].) For example, among patients whose arrest had a cardiac cause, there was a trend toward an increased proportion of patients surviving to hospital discharge (15.5%, vs. 12.3% for patients with other causes of arrest; P=0.09) and an increased proportion surviving with a favorable neurologic status at discharge (18.9% vs. 13.5%, P=0.03) with chest compression alone
(Table 4Table 4 Outcomes in Subgroups of Patients.). The survival rate among patients with a noncardiac cause of arrest was 5.0% with instructions to perform chest compression alone, as compared with 7.2% with instructions to perform chest compression plus rescue breathing (P=0.29).
In efficacy analyses restricted to patients for whom the intervention progressed to chest compression, the magnitude of outcome differences potentially favoring chest compression alone was typically larger than that observed in the effectiveness analyses (Tables 1 and 2 in the Supplementary Appendix).
Discussion
In this multicenter, randomized trial, CPR instructions consisting of chest compression alone did not increase survival to hospital discharge overall, as compared with instructions consisting of chest compression plus rescue breathing. However, the results suggest that chest compression alone may increase survival among certain subgroups of patients — those with a cardiac cause of arrest and those with ventricular fibrillation.
The current trial was designed to acknowledge the heterogeneity of the arrest condition and the potential for disparate intervention effects across the arrest population, providing in turn the truest translation of the intervention effects to community-based care.22-24 We found no significant difference between the two types of CPR instruction with respect to the proportion of patients who survived to hospital discharge. We did, however, observe a consistent trend toward clinically meaningful survival differences in favor of chest compression alone over chest compression plus rescue breathing among patients whose arrest was due to a cardiac cause (15.5% vs. 12.3%) and among those with a shockable arrest rhythm (31.9% vs. 25.7%). These findings in specific clinical groups are consistent with the results of investigations that have focused on the same subgroups of patients or have used corresponding animal models.10,11 One possible explanation is that the beneficial physiological effects of continuous chest compressions outweigh the beneficial physiological effects of chest compressions interspersed with rescue breathing.25 Alternatively, rescue breathing attempted by bystanders may have no physiological effects, so the comparison is essentially between two strategies: continuous chest compressions and interrupted chest compressions.
We did not observe significant differences in outcome among the patients with noncardiac causes of arrest or nonshockable rhythms, although the proportion of patients who survived was greater in the group randomly assigned to chest compressions plus rescue breathing. Because these two (nonexclusive) subgroups accounted for 14.0% (32 of 227) and 21.1% (48 of 227) of survivors, respectively, they cannot be dismissed as clinically unimportant. One interpretation of these results is that the type of bystander CPR does not make a difference in these subgroups. Alternatively, one may speculate that the potential difference is consistent with the physiological understanding of rescue breathing and that the study was underpowered to rigorously evaluate the type of CPR in these subgroups.
Taken together, the potential differential effects of CPR with and without rescue breathing may support a more targeted application of type-specific CPR. On the basis of data from the current study, such a tailored approach, if correctly applied according to the cause of arrest, would theoretically result in 156 survivors with a favorable neurologic outcome per 1000 patients, as compared with 144 per 1000 if chest compression alone were used for all patients or 115 per 1000 if chest compression plus rescue breathing were used for all patients. Future investigation may consider whether straightforward, operational etiologic surrogates can facilitate type-specific CPR aimed at the underlying cause of arrest.
We also did not observe outcome differences overall when we evaluated neurologic status at discharge. This finding provides assurance that improved resuscitation with chest compression alone is not achieved at the cost of neurologic impairment. Indeed, there was some suggestion that the brain may derive specific benefit, given the increase in the magnitude of both the relative and absolute differences favoring chest compression alone over chest compression plus rescue breathing, as evident from the two contrasting outcomes — survival (16.8% and 14.7%, respectively) and survival with favorable neurologic status (14.4% and 11.5%) (Table 3). Because CPR has a host of effects, a brain-specific advantage related to chest compression alone may be plausible.26
It is also useful to contrast the effectiveness and efficacy results in this study. The trial was an effectiveness study, since about one fourth of the patients did not progress to chest compressions. Conversely, three fourths did progress to chest compressions (the group constituting efficacy results) — a finding that underscores the important contribution a well-trained, assertive emergency dispatch program can make to increase bystander CPR. The magnitude of outcome differences potentially favoring chest compression alone was typically larger in the efficacy analysis as compared with the effectiveness analysis (Tables 1 and 2 in the Supplementary Appendix). One interpretation is that the efficacy associations better reflect the intervention's true physiological effects, suggesting that the potential benefit of chest compression alone is not due simply to a greater proportion of bystanders implementing chest compressions but may be due instead to the specific physiological effects of chest compression alone.
The current trial has limitations. The intervention randomized bystander CPR either to chest compressions alone or to chest compressions interspersed with rescue breathing in a ratio of 2 breaths to 15 compressions. This 2:15 ratio was the guideline specified during the first portion of the trial. One might expect that the results — and specifically the differences observed — would be attenuated if the ratio had been 2:30. Such an inference is uncertain given the incomplete understanding of the mechanisms underlying the benefit of CPR and the fixed logistic considerations of incorporating rescue breathing.27 We were able to assess progress through the study protocol, although we were not able to objectively and quantitatively measure the core components of the resuscitation maneuver (e.g., chest compression depth).
This investigation involved dispatcher-instructed CPR. The results do not apply to health professionals, who have a duty to respond and are more practiced and proficient in CPR, often engaging at a later stage of arrest physiology. Also, the results do not necessarily apply to bystanders who have been previously trained, are able to identify a cardiac arrest, and can provide CPR without dispatcher assistance. Nonetheless, CPR performed by lay responders trained in compression plus rescue breathing often falls short of the guideline standards during an actual cardiac arrest.28
The optimal outcome measure incorporates both heart and brain resuscitation. Our study determined the neurologic status of survivors at two of the three trial sites. We do not know whether the distribution of neurologic status differed at the third site, although those who survived from the third site represent only about 10% of all the survivors.
Although nearly 2000 eligible patients were enrolled, the study may still be criticized for having insufficient power to detect clinically important differences. For example, the study would need approximately 4200 subjects to have 80% power to demonstrate a significant difference in survival with a favorable neurologic outcome between the group treated with chest compression alone and the group treated with chest compression plus rescue breathing (14.4% and 11.5%, respectively).
We used a 95% confidence interval to designate statistical significance, although multiple comparisons were performed. Thus, caution should be exercised when interpreting the results, since one might expect about 5% of comparisons to be statistically significant simply by chance.29 It is important to note that the subgroup analyses were all prespecified. Moreover, the pattern of results across subgroups is consistent with the scientific understanding of type-specific CPR mechanistic effects, so collectively these results may strengthen the interpretation.
The study's limitations should be balanced against its strengths. Cardiac arrest is a major public health challenge for which high-level evidence to guide care is lacking. Our trial was conducted in three different emergency medical systems, the intervention was randomized and was validated through audio review, the outcomes are clinically meaningful, and the design allowed for capture of a comprehensive study population so that translation of the results to the community can be reasonably gauged.
In conclusion, this randomized trial showed that dispatcher CPR instruction consisting of chest compression alone did not increase survival when compared with chest compression plus rescue breathing overall. However, there was a consistent trend toward meaningful outcome differences in favor of chest compression alone in key clinical subgroups (i.e., patients with a cardiac cause of arrest and patients with shockable rhythms). The results, viewed within the context of other investigations, strengthen a layperson CPR strategy that emphasizes chest compression and minimizes the role of rescue breathing.
Supported in part by grants from the Laerdal Foundation for Acute Medicine and the Medic One Foundation.
Drs. Rea and Eisenberg report receiving defibrillators and funding from Philips Medical Systems and Physio-Control to evaluate research questions related to automated external defibrillator training and use, and report that their institutions, the University of Washington and Public Health for Seattle and King County, have received funding from the Medtronic Foundation involving community-based translation of resuscitation science. Dr. Rea reports being a member of the American Heart Association Basic Life Support Committee. No other potential conflict of interest relevant to this article was reported.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 