US Pharm. 2013;38(5):43-46.
ABSTRACT: Acne is no longer considered a health problem strictly of adolescence, as its prevalence in adults has significantly increased. Acne vulgaris and acne rosacea are diagnosed based on the clinical presentation of the patient’s skin and are classified primarily according to severity. The treatment of acne should be approached in a stepwise fashion. Successful outcomes generally involve combination therapy with different drug mechanisms. Although acne vulgaris and acne rosacea may be considered minor issues from a medical standpoint, either form can have a significant psychosocial impact on the patient’s quality of life. Health care providers involved in the care of patients with acne should be extremely sensitive not only to acne’s physical manifestations, but also to the emotional burdens resulting from it.
Acne, once viewed as strictly an adolescent health problem, now affects an increasing number of adults. The exact cause of this dermatologic disorder is unclear. Both acne vulgaris and acne rosacea are discussed in this article.
ACNE VULGARIS
An estimated 17 to 28 million Americans suffer from acne vulgaris.1 Although up to 85% to 90% of all teenagers report having some degree of acne, this dermatologic disorder also can affect adults aged 20 to 40 years. Pubescent acne is more common in males than in females. In contrast, between 30% and 50% of adult women are diagnosed with acne.1-3 This shift in the incidence of acne from adolescence to an older age group has produced a much more demanding and articulate set of patients with high expectations of improvement.4
The underlying cause of acne is usually multifactorial, and the precise cause remains unknown. There are numerous precipitating factors, however, and these should be identified during the initial health history. Certain pharmacologic agents, including isoniazid, phenytoin, and lithium, have been associated with drug-induced acneiform eruptions. Personal care products such as moisturizers and cosmetics should be water based, noncomedogenic, and fragrance free. Hair products should be water based and should not come in contact with the forehead and temporal regions of the face. Although the ingestion of specific foods (e.g., chocolate, colas, greasy foods) does not cause acne, some studies have found that exposure to the cooking oils used in establishments such as fast-food restaurants may exacerbate the condition. This correlation has been debated, however. Hormonal imbalances such as androgen excess should be evaluated in women who present with treatment-resistant acne.1,3,5
Pathophysiology
Acne is believed to be caused by an abnormality in the structure or function of the pilosebaceous follicle, most likely because of the increased production of adrenogenic hormone. As a result, the follicular canal widens and cell production or keratinization increases. The sebaceous glands eventually atrophy, and sebum mixes with the loose cells to form a keratinous plug appearing as a blackhead (open comedo). Trauma or inflammatory changes may lead to the formation of a whitehead (closed comedo). If the follicular canal is damaged, the contents of the follicle may extrude into the dermis and initiate an inflammatory response. If the inflammation is close to the surface, a papule or pustule forms. If the inflammation is deeper in the dermis, a nodule or cyst develops; permanent scarring is possible.3
The anaerobic gram-positive bacterium Propionibacterium acnes, part of the normal flora colonization in the pilosebaceous follicle, plays an important role in the initial development and maintenance of acne. Although P acnes itself is not a cause of infection, the bacterium converts triglycerides in the sebum into free fatty acids that attract inflammatory cells, including polymorphonuclear leukocytes and monocytes.6
Diagnosis
Acne vulgaris is diagnosed based on the clinical presentation of the patient’s skin, with classification primarily made according to severity. The mildest form is comedonal (open or closed comedones). Mild inflammatory acne is manifested by papules. Moderate inflammatory acne consists of pustules and some cysts. Severe cystic acne manifests as cysts, nodules, and scarring.3,4
Treatment
The main goals of pharmacotherapy for acne vulgaris are to prevent new lesions and reduce the number and severity of existing lesions; prevent scarring and hyperpigmentation; and limit the duration of disease.7 The patient should be counseled that improvement is seen approximately 4 to 6 weeks after initiation of therapy. Some forms of acne may require continuous treatment throughout adolescence into early adulthood. Nonpharmacologic measures should include a gentle, nondrying skin cleanser used no more than twice daily. Skin scrubbing and excessive face washing do not necessarily open or cleanse pores, and these practices may lead to irritation and acne exacerbation.3,4
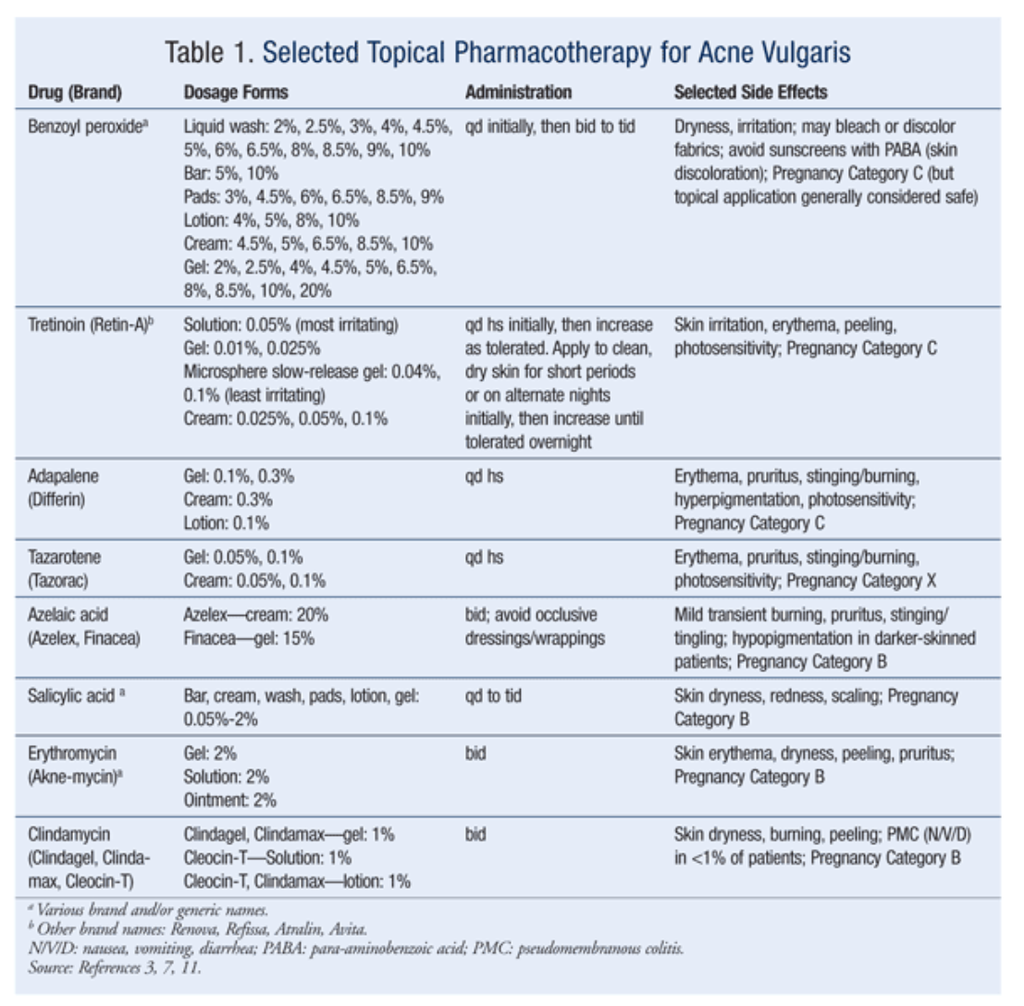
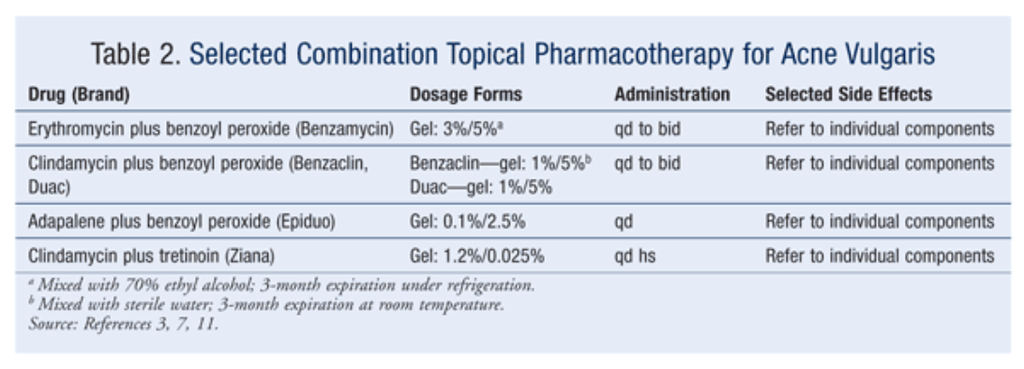
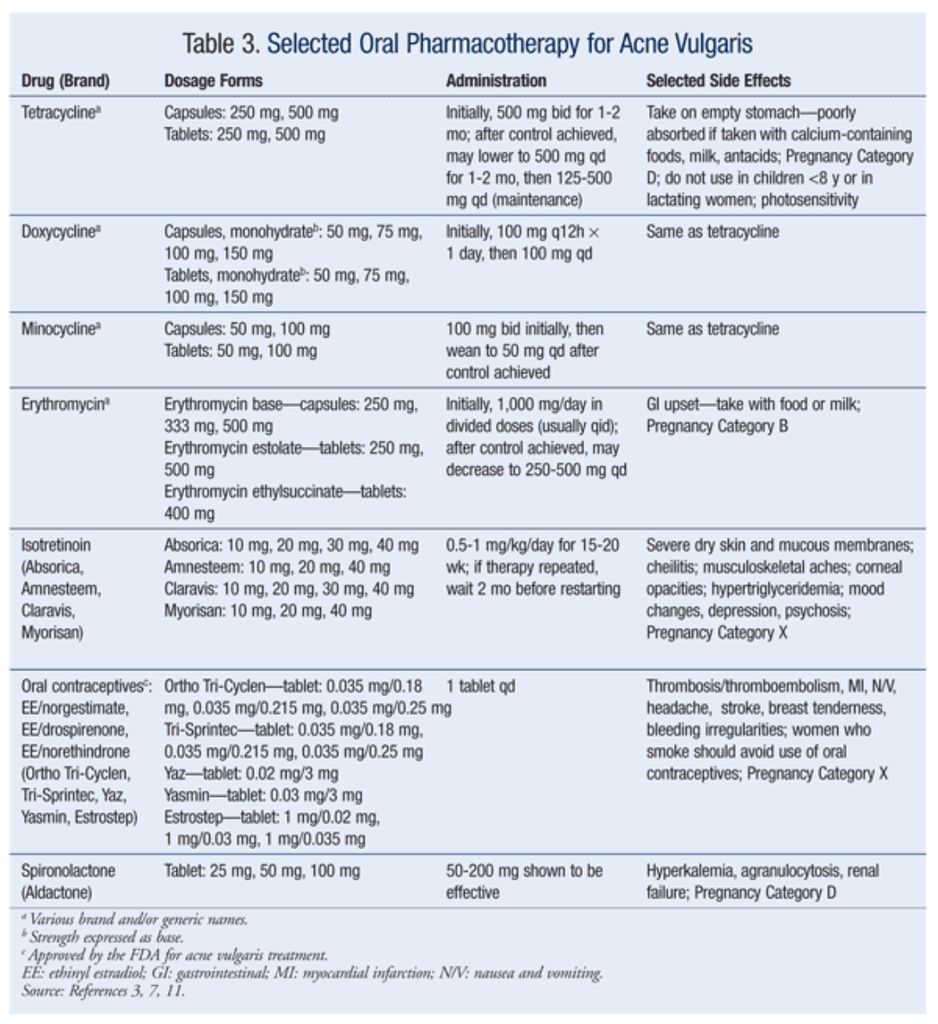
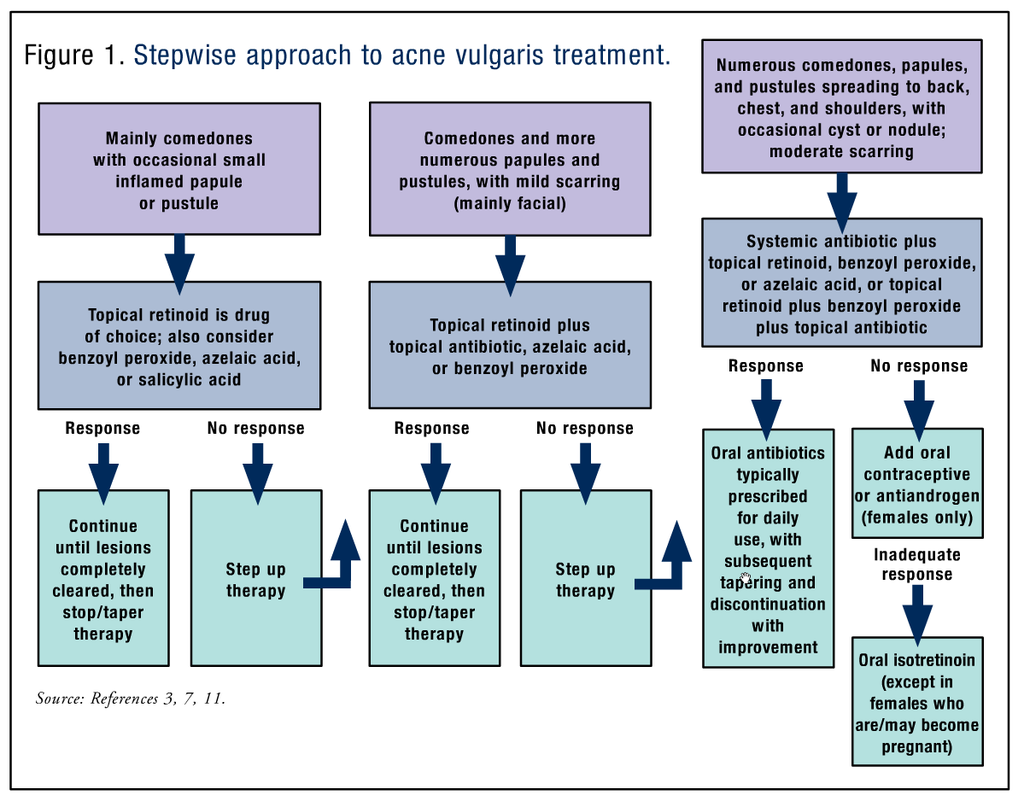
The treatment of acne should be approached in a stepwise fashion.7 If the acne is mild or moderate and involves primarily comedonal lesions with an occasional small inflamed papule or pustule, the preferred products are benzoyl peroxide, azelaic or salicylic acid, and topical retinoids. These topical agents improve the defect in keratinization by promoting effective skin exfoliation. Currently, successful treatment outcomes generally involve combination therapy with different drug mechanisms.8-10 TABLES 1, 2, and 3 summarize the various topical and oral preparations for acne vulgaris.
Topical treatment forms include creams, lotions, solutions, gels, and disposable wipes in various concentrations. The patient’s response to these formulations varies depending upon individual skin type. Many gels and solutions contain considerable amounts of alcohol. If a patient is experiencing significant dryness despite a low concentration of active drug component, the provider should consider switching to a preparation that does not contain alcohol, such as a cream or aqueous gel.3
For moderate-to-severe acne with predominantly inflammatory lesions, it is important to reduce the growth of P acnes in the follicular canal and the generation of its extracellular products and inflammatory effects. A combined topical retinoid with benzoyl peroxide, azelaic acid, or a topical antibiotic is recommended. If no considerable improvement is seen after approximately 6 weeks, or if the condition worsens, combination topical therapy is generally initiated before adding an oral antibiotic such as tetracycline, doxycycline, or minocycline.11 Other antimicrobials, including erythromycin and trimethoprim-sulfamethoxazole, may be used, but they may be less effective. Antimicrobial resistance, a growing concern, should be suspected in patients who do not respond within 8 to 16 weeks of antibiotic initiation.7
For severe recalcitrant acne with inflammatory lesions, extensive nodules, cysts, or scars, drugs that decrease sebaceous activity, such as selected oral contraceptives, antiandrogens, or isotretinoin, may be added to the regimen.12-14 Local corticosteroid injections are another effective option for large inflammatory lesions.7
The algorithm in FIGURE 1 summarizes the pharmacologic management of acne vulgaris.
Women of childbearing age who are using isotretinoin or tazarotene, which are teratogenic and classified as Pregnancy Category X, should be counseled to avoid becoming pregnant. Tetracycline, doxycycline, and minocycline, which also are contraindicated during pregnancy, may decrease the effectiveness of oral contraceptives. Women taking this antibiotic class should use a long-acting contraceptive, such as Depo-Provera, or a barrier method to prevent pregnancy. Retinoic acid, adapalene, and salicylic acid are Pregnancy Category C and should be avoided in women of childbearing age. Topical application of benzoyl peroxide is also Pregnancy Category C, but is generally considered safe for use during pregnancy.3,11,15
All patients receiving isotretinoin must participate in the iPLEDGE program, a pregnancy-prevention system designed to enhance safe and appropriate use of the drug through patient education.15,16 All female patients must have two negative urine or serum pregnancy tests before the initial isotretinoin prescription is written. In addition, for each month of therapy, a negative pregnancy test result must be obtained before the patient receives the next prescription, regardless of whether she is sexually active. Female patients who are or might become sexually active with a male partner must use two forms of effective contraception simultaneously for at least 1 month before initiation of therapy, throughout treatment, and for up to 4 months following discontinuation of therapy. The patient should be given patient information and a consent form detailing the association between isotretinoin and birth defects and other potentially serious drug-related risks.
Although the iPLEDGE program is beneficial and effective, criticisms abound. For many patients, the system has caused numerous delays in receiving isotretinoin therapy. The provider may not prescribe more than a 30-day supply, and a new prescription may not be written for at least 30 days.16 Moreover, pharmacists are under similar restrictions, and no more than a 30-day supply may be filled and dispensed to the patient. In addition, both the provider and the pharmacist must verify these written prescriptions in the online system before filling, and phone-in orders are not permitted.
There is also a 7-day window during which the medication must be picked up at the pharmacy once the prescription is dated by the prescriber. If the original prescription is lost or the prescription is not picked up during the 7-day window, the patient must wait 30 days to receive the drug. This strict sequence of requirements can make it extremely difficult for patients to receive and take isotretinoin according to the prescribed schedule. Recently, iPLEDGE procedures regarding nonchildbearing patients have been relaxed. However, these patients must still answer online questions monthly (as must their physician) and obtain regular blood tests (including CBC, chemistry profile, and fasting triglyceride and cholesterol levels), and they are subject to the 7-day window requirement.16,17
ACNE ROSACEA
Sometimes mistaken for acne vulgaris, acne rosacea is a dermatologic disorder that usually develops in middle-aged patients (30-50 years). It is characterized as a chronic inflammatory condition that primarily affects the central portion of the face. Rosacea is more likely to occur in women, although men may have more severe manifestations of the disorder.18
Pathophysiology
The etiology of rosacea is unclear, but various theories suggest nonspecific bacterial or fungal infections, accumulation of theDemodex folliculorum mite in the hair follicle, and menopausal changes. Easy flushing and blushing of the face and exacerbation of the disorder is often associated with the ingestion of alcohol, spicy foods, or caffeine-containing products and exposure to sun, strong winds, strenuous exercise, and stress.3,18
Diagnosis
Early vascular rosacea usually presents after exposure to cold weather environments. In response, increased blood flow to the superficial dermis results in erythema, with persistent telangiectasia occurring later in this stage. During this period, approximately 50% of patients report ocular involvement, from mild conjunctivitis, blepharitis, and dry eye syndrome to more severe cases of keratitis and corneal ulceration. Patients diagnosed with second-stage rosacea often present with telangiectasia and persistent papules and pustules superimposed on the existing erythemic rash. Hyperplasia of the sebaceous glands and connective tissue can lead to development of a large, red, bulbous nose (rhinophyma), which is almost exclusively seen in males older than 40 years and is treatable only by surgery. Late-stage rosacea also presents with persistent edema.3,18
Treatment
The main goal of therapy for acne rosacea is patient recognition of the specific triggers that potentiate the condition and cause flare-ups. As with acne vulgaris, patients should be advised to avoid harsh cleansers and to use only fragrance-free, hypoallergenic skin care and makeup products in order to reduce the risk of skin irritation.18
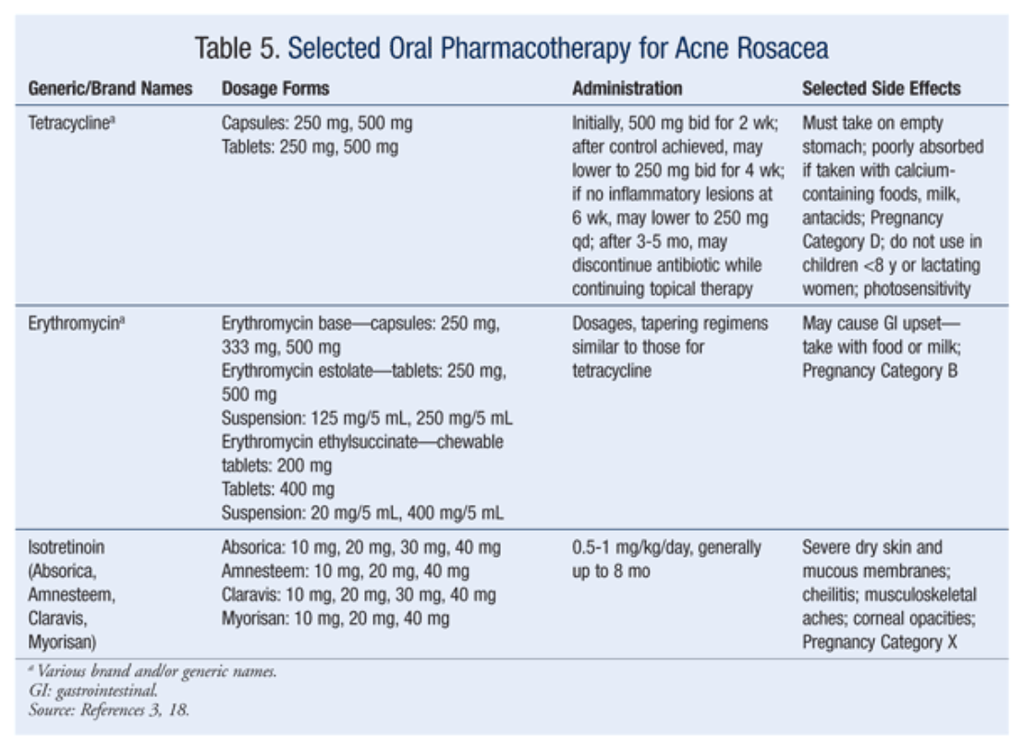
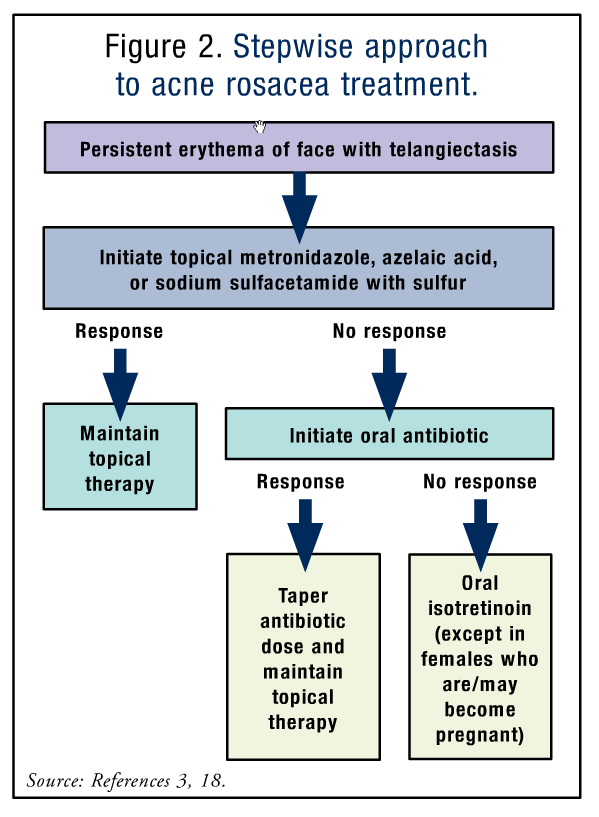
First-line treatment should include a topical agent. Cases that involve ocular symptoms should be treated with oral antibiotics. Metronidazole, sodium sulfacetamide with sulfur, and azelaic acid are treatment options. Topical clindamycin is an effective alternative for patients who cannot tolerate metronidazole. The mechanism by which topical metronidazole works to improve the inflammation is unknown, but it is most likely related to the drug’s antibacterial effect. Sodium sulfacetamide with sulfur and azelaic acid also exhibit anti-inflammatory properties and have been shown to be effective in treating mild-to-moderate rosacea.3,18
If no improvement is seen after 6 weeks, second-line therapy should be initiated. This involves adding an oral antibiotic mainly for its anti-inflammatory effect, rather than for its antibacterial properties. After 2 weeks, the dosage should be decreased by 50% and discontinued after 6 weeks while continuing the topical agent indefinitely.3,18
Third-line treatment consists of isotretinoin.3,18 Precautions and laboratory monitoring similar to those for acne vulgaris should be followed. TABLES 4 and 5 (available at www.uspharmacist.com) summarize the various topical and oral preparations for acne rosacea. The algorithm in FIGURE 2 summarizes the pharmacologic management of rosacea.
CONCLUSION
Although both acne vulgaris and rosacea may be considered minor clinical issues, numerous studies have determined that these disorders can have a significant psychosocial impact on the patient’s quality of life.19 Adolescents, who are already self-conscious and can be highly sensitive to physical imperfections no matter how little perceived by others, are generally stereotyped as being the most affected by acne. However, studies have demonstrated a direct correlation between the patient’s age and the negative impact on quality-of-life scores, regardless of severity. The patient’s concerns about personal appearance must be identified early in the course of treatment, as many patients experience psychological stress or depression secondary to the physical effects of the disorder.19,20 Health care providers should be extremely sensitive not only to acne’s physical manifestations, but also to the emotional burdens resulting from the condition.
REFERENCES
1. Feldman SR, Fleischer AB Jr, McConnell RC. Most common dermatologic problems identified by internists, 1990-1994.Arch Intern Med. 1998;158:726-730.
2. Fleischer AB Jr, Herbert CR, Feldman SR, O’Brien F. Diagnosis of skin disease by nondermatologists. Am J Manag Care.2000;6:1149-1156.
3. Poole Arcangelo V, Peterson A. Pharmacotherapeutics for Advanced Practice: A Practical Approach. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012:183-193.
4. Healey E, Simpson N. Acne vulgaris. BMJ. 1994;308:831-833.
5. Bowe WP, Joshi SS, Shalita AR. Diet and acne. J Am Acad Dermatol. 2010;63:124-147.
6. Webster GF, McGinley KJ, Leyden JJ. Inhibition of lipase production in Propionibacterium acnes by sub-minimal-inhibitory concentrations of tetracycline and erythromycin. Br J Dermatol. 1981;104:453-457.
7. Strauss JS, Krowchuk DP, Leyden JJ, et al. Guidelines of care for acne vulgaris management. J Am Acad Dermatol. 2007;56:651-663.
8. Leyden JJ, Hickman JG, Jarratt MT, et al. The efficacy and safety of a combination benzoyl peroxide/clindamycin topical gel compared with benzoyl peroxide alone and a benzoyl peroxide/erythromycin combination product. J Cutan Med Surg. 2001;5:37-42.
9. Wolf JE Jr, Kaplan D, Kraus SJ, et al. Efficacy and tolerability of combined topical treatment of acne vulgaris with adapalene and clindamycin: a multicenter, randomized, investigator-blinded study. J Am Acad Dermatol. 2003;49(suppl 3):S211-S217.
10. Richter JR, Bousema MT, De Boulle KL, et al. Efficacy of a fixed clindamycin phosphate 1.2%, tretinoin 0.025% gel formulation (Velac) in the topical control of facial acne lesions. J Dermatol Treat. 1998:9:81-90.
11. Tan HH. Antibacterial therapy for acne: a guide to selection and use of systemic agents. Am J Clin Dermatol. 2003;4:307-314.
12. Redmond GP, Olson WH, Lippman JS, et al. Norgestimate and ethinyl estradiol in treating acne vulgaris: a randomized, placebo-controlled trial. Obstet Gynecol. 1997;89:615-622.
13. Shaw JC. Low-dose adjunctive spironolactone in the treatment of acne in women: a retrospective analysis of 85 consecutively treated patients. J Am Acad Dermatol. 2000;43:498-502.
14. Layton AM, Knaggs H, Taylor J, Cunliffe WJ. Isotretinoin for acne vulgaris—10 years later: a safe and successful treatment. Br J Dermatol. 1993;129:292-296.
15. FDA. MedWatch 2002 Safety Alert—Accutane (isotretinoin) Dear Accutane Prescriber letter. Rockville, MD: FDA.
16. iPLEDGE. www.ipledgeprogram.com. Accessed April 8, 2013.
17. Barth JH, MacDonald-Hull SP, Mark J, et al. Isotretinoin therapy for acne vulgaris: a re-evaluation of the need for measurements of plasma lipids and liver function tests. Br J Dermatol. 1993;129:704-707.
18. Goldgar C, Keahey DJ, Houchins J. Treatment options for acne rosacea. Am Fam Physician. 2009;80:461-468.
19. Lasek RL, Chren MM. Acne vulgaris and the quality of life of adult dermatology patients. Arch Dermatol. 1998;134:454-458.
20. Aktan S, Ozmen E, Sanli B. Anxiety, depression, and nature of acne vulgaris in adolescents. Int J Dermatol.2000;39:354-357.






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 