US Pharm. 2011;36(12):49-52.
Traveler’s diarrhea (TD) is the most common ailment affecting persons from industrialized countries who visit developing areas. Depending upon the region being visited, approximately 30% to 70% of international travelers develop TD, with the highest rates occurring in Latin America, Southern Asia, and Africa.1 TD is rarely life threatening, but it can be severely debilitating in children and the elderly, since severe dehydration can occur rapidly. Millions of travelers are affected by TD annually, so it is vital that pharmacists proactively educate individuals who will be traveling about preventive measures and treatment.
Epidemiology
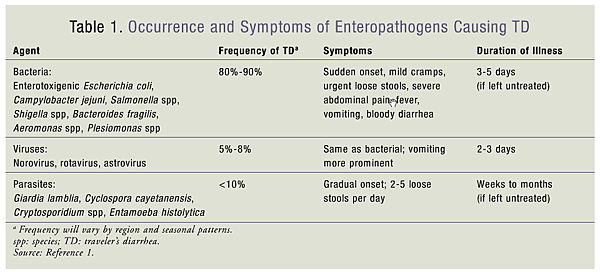
Bacterial pathogens are thought to account for 80% to 90% of TD. The most causative organism is enterotoxigenic Escherichia coli, followed by Campylobacter jejuni, Shigella species, and Salmonella species.1 Some bacteria release toxins that bind to the intestinal wall and cause diarrhea, while others damage the intestine merely by their presence. Enteric viruses (e.g., rotavirus and norovirus), which occur primarily in infants and children, can cause TD; parasitic pathogens such as Giardia and Cryptosporidium can cause it as well (TABLE 1).
According to the CDC, the traveler’s destination is the most important determinant of risk, with the world divided into three risk grades: low, intermediate, and high.1 The highest-risk regions for acquiring TD are the Middle East, Latin America, Southern Asia, Mexico, and Africa. Rates of TD in these regions range from 20% to 90% per 2-week stay.2 Intermediate-risk areas include Eastern Europe, South Africa, and parts of the Caribbean Islands, with TD occurring in approximately 8% to 20% of visitors. The United States, Canada, Australia, New Zealand, Japan, and Western Europe are considered low-risk regions, with TD rates of less than 8%.2 Travelers who are immunosuppressed or who have a history of inflammatory bowel disease or diabetes are at higher risk for developing TD.
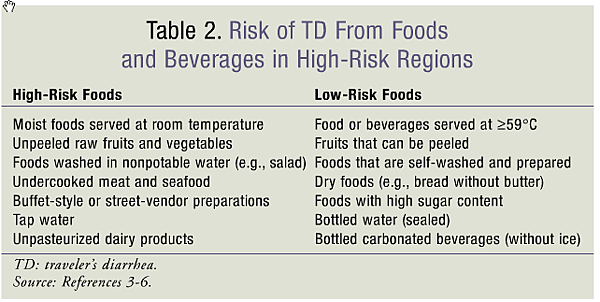
Contact with contaminated objects or with a person who has poor hygiene can lead to the transmission of TD; however, the most common mode of transmission is the consumption of contaminated food and water.1 Travelers should be mindful of high-risk food items that may predispose them to TD (TABLE 2). Foods that are raw or not freshly cooked are often unsafe for consumption since they provide an excellent growth medium for microorganisms, as opposed to hot, freshly cooked foods and dry foodstuffs such as bread. Consumption of moist foods served at room temperature—such as salads and buffet-style or street-vendor preparations—and excessive consumption of alcohol (>5 drinks/day) increase the traveler’s risk of TD.3-6 Bottled water and carbonated beverages with an unbroken seal are less likely than tap water to cause TD. Beverages (e.g., coffee and tea) that are heated to a temperature of at least 59°C are less likely to cause TD because the bacteria are effectively killed.4
Clinical Presentation
Often considered a clinical syndrome, TD may present with a variety of enteric symptoms, including abdominal cramps, nausea, vomiting, low-grade fever, low or nonexistent appetite, and bloody stools. A classic TD episode may be described as the passage of three or more loose stools in a 24-hour period, plus one or more enteric symptoms. The onset of TD can occur rapidly if a high concentration of bacteria was ingested, with most TD cases lasting for 3 to 5 days. Commonly found on cruise ships and commercial airliners, viral pathogens such as norovirus present with vomiting and a similar duration of illness.7,8 Symptoms of TD are generally self-limited and short in duration. Approximately 20% of travelers are confined to bed for 1 to 2 days, and up to 40% must reschedule their planned activities.5 The majority of TD cases occur during the first week of travel and may resolve within a few days without treatment; however, it is possible to have more than one episode on the same trip.
Persistent TD is described as diarrhea in the traveler or recently returned traveler that lasts more than 14 days.9 Often seen in long-term travelers, persistent TD is most likely due to protozoal parasites, with a delayed onset of symptoms that may persist for several weeks. Coinfection with Clostridium difficile may occur in patients who have already been treated with antibiotics for malaria prophylaxis or post–infectious irritable bowel syndrome.10,11 In general, fever and vomiting resolve first, but the traveler will continue to experience abdominal pain and diarrhea that improves with defecation.
Prevention
There are several preventive measures that may reduce the likelihood of developing TD, including education about the avoidance of high-risk foods and beverages, good hygiene, and use of prophylactic medications.
The best means of preventing TD is education regarding food and beverage selection, with the goal that the traveler avoid the consumption of high-risk products. The aphorism “Boil it, cook it, peel it, or forget it” remains standard preventive advice, as travelers to high-risk areas should avoid consuming untreated tap water, raw fruits and vegetables not washed by the traveler, and undercooked meats and seafood.1 In addition, travelers should be informed that boiled water and foods treated with iodine or chlorine may be safely consumed. Although preventive measures are recommended, travelers may not be able to adhere to the recommendations, since many factors for ensuring food safety, such as restaurant hygiene, are beyond their control.
Hand washing has been shown to reduce the incidence of diarrhea by up to 30% in community settings.12 Travelers should routinely wash their hands using soap and water while preparing food, before eating, and after using the toilet. If soap and water are not available, an alcohol-based hand sanitizer containing at least 60% alcohol should be used to sterilize the hands.1
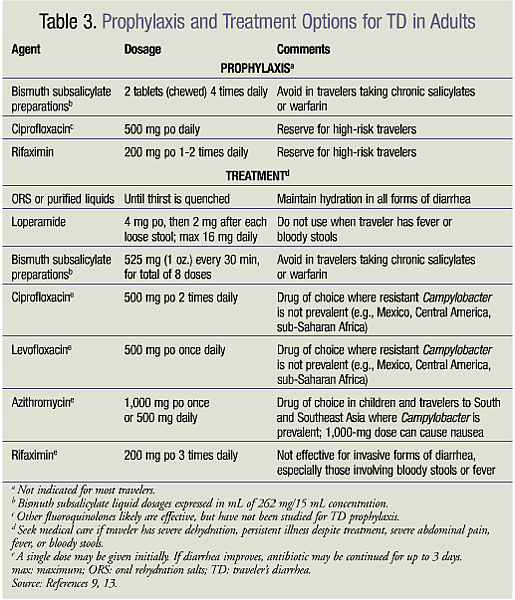
Bismuth subsalicylate (BSS), the active ingredient in Pepto-Bismol, has been shown to be effective in the prevention of TD.13 When 4.2 g and 2.1 g of BSS were taken four times a day for 3 weeks, protection rates of 62% and 65%, respectively, were achieved.14,15 To date, the safety of BSS use beyond 3 weeks has not been established. BSS should not be used in children aged less than 3 years, patients allergic to aspirin, those taking oral anticoagulants, and those with a history of renal insufficiency or gout. Caution should be exercised in travelers currently taking aspirin or salicylates because of the risk of salicylate toxicity, and in children with viral infections owing to the risk of Reye’s syndrome. BSS commonly causes blackening of the tongue and stools and can cause nausea, constipation, and tinnitus. To avoid developing a black tongue, travelers should brush their teeth and rinse their mouth after each dose, and should consider gently brushing the tongue after an evening dose.3
Although prophylactic antibiotics have been shown to be effective for TD, they are not recommended in most situations because of the risk of adverse reactions and the risk of antibiotic resistance should a serious infection occur. Prophylaxis should be used only in travelers who are immunocompromised and in those with chronic intestinal disorders or a history of disabling bouts of TD. Antibiotic prophylaxis should be considered for individuals in whom a single episode of TD would have costly adverse consequences, such as a critically important business or athletics trip. Ciprofloxacin and rifaximin—a nonabsorbed antibiotic that achieves high concentrations in the intestine—can prevent TD, with efficacy rates of 70% to 90%.5 Rifaximin is not currently FDA approved for TD prophylaxis but should be considered for short-term travelers who are high-risk hosts.16 TABLE 3 lists the various medications used for the prevention and treatment of TD.9,13
Treatment
If left untreated, severe cases of acute TD can lead to potential fluid and electrolyte losses and significant volume depletion. All individuals traveling to high-risk regions should be equipped with medications for initiation of self-treatment for potential illness. Treatment goals include avoiding dehydration, reducing the severity and duration of symptoms, and preventing disruption of the traveler’s planned activities. Bacterial causes of TD outnumber other microbial causes; therefore, antibiotics are the mainstay of treatment, whereas adjunctive agents are used for symptomatic control.
Antibiotics may be given to travelers with moderate-to-severe symptoms who have not responded to symptomatic treatment. A single oral dose of an antibiotic is often sufficient to effectively treat TD; however, the antibiotic may be taken for up to 3 days if there is no improvement following the first dose.1 The efficacy of the empiric antibiotic depends upon the susceptibility of the bacteria. Fluoroquinolones are the most effective antibiotics for the treatment of bacterial TD; however, their use has been limited owing to the increasing rate of fluoroquinolone resistance, specifically in the Campylobacter species. The empiric use of fluoroquinolones should be avoided in individuals traveling to Southern or Southeastern Asia, where Campylobacter is prevalent.1 Macrolides such as azithromycin are not as rapidly effective as the fluoroquinolones, but are active against fluoroquinolone-resistant Campylobacter isolates. Macrolides should be considered as an alternative to fluoroquinolones and as first-line antibiotic therapy in children. Rifaximin, which is as effective as ciprofloxacin for the treatment of TD, is approved for the treatment of noninvasive TD caused by strains of E coli; however, travelers will find it difficult to distinguish between invasive and noninvasive diarrhea.16-18
The combination of an antimotility agent, such as loperamide, plus an antibiotic will provide the fastest clinical response and is useful for travelers who need prompt reversal of their illness.19 Antimotility agents may be used to reduce bowel-movement frequency and provide symptomatic relief, allowing the individual to travel on an airplane or bus while waiting for adjunctive antibiotics to take effect. Of note, antimotility agents can shorten the duration of illness, but they do not eradicate an infection; therefore, they should be avoided in complicated cases of TD involving fever or bloody stools.
Because TD can cause a severe loss of fluid and electrolytes, adequate hydration should be maintained for all forms of diarrhea and is especially important in young children and adults with chronic medical conditions. For mild cases of TD, oral hydration may be all that is necessary. In infants, breastfeeding and adequate fluid intake should be maintained. Travelers should consume only beverages that are sealed or known to have been purified. Sports drinks are fine for maintaining hydration, but are inappropriate for the treatment of diarrhea. For severe fluid loss, fluid replacement may be achieved through the use of the World Health Organization’s oral rehydration salts (ORS). ORS, which may be purchased in pharmacies in most developing countries, is prepared by dissolving the contents of one packet in the appropriate volume of boiled or treated water.20 Alternatively, oral rehydration solutions such as Pedialyte or similar commercially available solutions containing appropriate amounts of sodium, potassium, and glucose may be used for rehydration if the traveler can drink the required volume. Hydration should continue until the traveler’s thirst has been quenched.
Conclusion
Despite advances in understanding its pathogenesis and geographic distribution, TD continues to remain an important cause of morbidity among international visitors. In most cases, TD is acquired primarily through the consumption of contaminated food or water. TD can be prevented with proper education and may be treated with OTC products and prescription antibiotics. Pharmacists should provide travelers to high-risk areas the best information regarding TD to avoid disruption of their planned activities.
REFERENCES
1. CDC. CDC Health Information for International Travel 2012. New York, NY: Oxford University Press; 2012. 2. Steffen R. Epidemiology of traveler’s diarrhea. Clin Infect Dis. 2005;41:S536-S540. 3. Ericsson CD. Travellers’ diarrhoea. Int J Antimicrob Agents. 2003;21:116-124. 4. Dupont HL, Steffen R. Textbook of Travel Medicine and Health. Hamilton, ON: BC Decker; 1997:78-86. 5. Okhuysen PC. Current concepts in travelers’ diarrhea: epidemiology, antimicrobial resistance and treatment. Curr Opin Infect Dis. 2005;18:522-526. 6. Huang DB, Sanchez AP, Triana E, et al. United States male students who heavily consume alcohol in Mexico are at greater risk of travelers’ diarrhea than their female counterparts. J Travel Med. 2004;11:143-145. 7. CDC. Outbreaks of gastroenteritis associated with noroviruses on cruise ships—United States, 2002. MMWR Morb Mortal Wkly Rep. 2002;51:1112-1115. 8. Thornley CN, Emslie NA, Sprott TW, et al. Recurring norovirus transmission on an airplane. Clin Infect Dis. 2011;53:515-520. 9. Guerrant RL, Van Gilder T, Steiner TS, et al. Practice guidelines for the management of infectious diarrhea. Clin Infect Dis. 2001;32:331-351. 10. Dupont HL. New insights and directions in travelers’ diarrhea. Gastroenterol Clin North Am. 2006;35:337-353. 11. Connor BA. Sequelae of traveler’s diarrhea: focus on postinfectious irritable bowel syndrome. Clin Infect Dis. 2005;41:S577-S586. 12. Ejemot RI, Ehir JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev. 2008;(1):CD004265. 13. Hill DR, Ericsson CD, Pearson RD, et al. The practice of travel medicine: guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43:1499-1539. 14. DuPont HL, Sullivan P, Evans DG, et al. Prevention of traveler’s diarrhea (emporiatric enteritis): prophylactic administration of subsalicylate bismuth. JAMA. 1980;243:237-241. 15. DuPont HL, Ericsson CD, Johnson PC, et al. Prevention of travelers’ diarrhea by the tablet formulation of bismuth subsalicylate. JAMA. 1987;257:1347-1350. 16. Xifaxan (rifaximin) package insert. Raleigh, NC: Salix Pharmaceuticals, Inc; October 2011. 17. DuPont HL, Jiang ZD, Ericsson CD, et al. Rifaximin versus ciprofloxacin for the treatment of traveler’s diarrhea: a randomized, double-blind clinical trial. Clin Infect Dis. 2001;33:1807-1815. 18. DuPont HL, Jiang ZD, Okhuysen PC, et al. A randomized, double-blind, placebo-controlled trial of rifaximin to prevent travelers’ diarrhea. Ann Intern Med. 2005;142;805-812. 19. Sanders JW, Frenck RW, Putnam SD, et al. Azithromycin and loperamide are comparable to levofloxacin and loperamide for the treatment of traveler’s diarrhea in United States military personnel in Turkey. Clin Infect Dis. 2007;45:294-301. 20. World Health Organization. Oral Rehydration Salts: Production of the New ORS. Geneva, Switzerland: World Health Organization; 2006.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 