因為網路分級的關係,本篇文章具有大量引起妳不舒服及可能改變妳身心狀態的圖片,請確定妳已經成年及心智成熟,否則請不要閱讀,謝謝

Herpes zoster is a reactivation of the varicella zoster virus (VZV), which remains dormant in the dorsal root ganglion following primary varicella infection. After years of latency, the virus travels along the nerve to the skin, resulting in a dermatomal distribution (shown). Lesions are often preceded by pain and hyperesthesia of the skin. Zoster is more common in patients who are older or immunosuppressed, including organ transplant recipients and patients with human immunodeficiency virus (HIV).[1] Image courtesy of Brooke Army Medical Center.
Herpes zoster (shown) usually has a benign course, but complications can occur, ranging from mild to life threatening. Common complications of herpes zoster infections include acute pain, postherpetic neuralgia, persistent neuropathy, hemorrhage, ulceration, necrosis, myonecrosis, necrosis of bone, and (uncommonly) secondary bacterial infection.[1] Image courtesy of Wikimedia Commons.
Morphologically, the classic lesions of herpes zoster consist of umbilicated vesicles on an erythematous base. The vesicles occur in small clusters referred to as herpetiform groupings (shown). With time, the vesicles become confluent, crusted, and often heal with scarring. Zoster sine herpete presents with neuralgic pain in the absence of skin lesions. Pain and weakness can persist for months.
Early herpes zoster outbreaks can be easily mistaken for what other condition?
A. Arthropod bites
B. Furuncles
C. Impetigo
D. All of the above
Answer: D. All of the above
The morphology of herpes zoster can result in misdiagnosis by clinicians who are not familiar with the typical patterns of presentation. The dermatomal distribution of zoster typically stops abruptly at the midline, as shown. Dermatomes on the trunk have a horizontal distribution, whereas those on the arms and legs have an arcuate or roughly linear distribution. Within the dermatome, the clusters of vesicles and crusts often have a patchy distribution, in clustered herpetiform groupings. The hypersensitivity of the overlying skin to light touch and presence of spontaneous pain are helpful diagnostic features.
Discontinuous round lesions, such as the one pictured, are often misdiagnosed because the dermatomal distribution is not apparent.
Which of the following tests is the most appropriate to confirm the diagnosis of zoster?
A. Traditional viral culture
B. Shell vial viral culture
C. Direct fluorescent antibody (DFA)
D. Polymerase chain reaction (PCR)
E. Bacterial culture
Answer: D. Polymerase chain reaction (PCR)
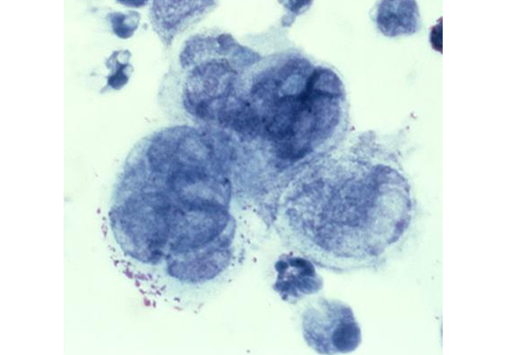
The Tzanck smear (shown) is a classic test for the diagnosis of VZV, in which the base of an ulcerated lesion is scraped and then stained. However, it cannot differentiate between VZV and herpes simplex. PCR has high sensitivity and specificity, approaching 100%.[2] PCR is inexpensive and has replaced DFA as the assay of choice in many large labs. Viral cultures have high false-negative rates and take 2 weeks for a result. Bacterial cultures can help exclude secondary bacterial infection, but do not confirm a diagnosis of zoster. Image courtesy of the Centers for Disease Control and Prevention.
This patient shown here presented with a week of severe pain involving the leg, followed by eruption of herpetiform vesicles. The vesicles rapidly progressed to pustules with necrosis and ulceration.
Which of the following is the most appropriate 1-week treatment course for zoster?
A. 1 g of famciclovir 3 times daily
B. 1 g of alacyclovir 3 times daily
C. 1 g of valacyclovir 3 times daily
D. 1 g of methylprednisolone 3 times daily
E. 1 g of prednisone 3 times daily
Answer: C. 1 g of valacyclovir 3 times daily
Treatment for zoster usually involves a 1-week course of an antiviral medication, such as valacyclovir or famciclovir. Standard adult doses are 1 g of valacyclovir or 500 mg of famciclovir 3 times daily for 7 days. The dosing for alacyclovir is 800 mg 5 times daily. If initiated within 72 hours of the rash onset, antiviral medication may reduce the length of acute pain and speed cutaneous healing.[3]
Zoster can often mimic other pathological entities. This patient developed acute weakness and pain in the left arm and was initially evaluated for an acute cardiac event. Patients developing Ramsay Hunt syndrome (also known as herpes zoster oticus, geniculate neuralgia, or herpes zoster auricularis) are often suspected of having trigeminal neuralgia or even a cerebrovascular event when they present with symptoms such as acute onset of facial pain or facial hemiparesis.
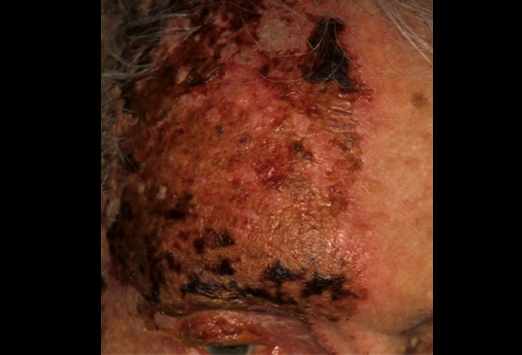
Ramsay Hunt syndrome is a rare complication in which VZV travels down the geniculate ganglion, causing otalgia, facial hemiparesis, and the classic vesicular eruption shown here. Vesicular eruptions may manifest on the pinna, tragus, or tympanic membrane; in the auditory canal; or anywhere on the facial nerve distribution. The patient may experience hearing impairment, nystagmus, vertigo, facial nerve palsy (mimicking Bell palsy), or loss of taste sensation in the anterior two-thirds of the tongue. Ramsay Hunt syndrome may go unnoticed and be difficult to diagnose, especially in the elderly.[1]
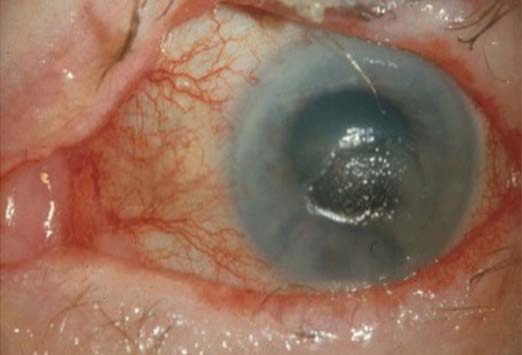
Herpes zoster may involve the ophthalmic division of the trigeminal nerve, leading to involvement of the forehead, nose, and eye, as shown. This involvement is associated with complications such as conjunctivitis, keratitis, corneal ulceration, iridocyclitis, glaucoma, and blindness. Early consultation with an ophthalmologist is recommended. Image courtesy of Manolette Roque, MD, Ophthalmic Consultants Philippines Co.
This patient presented with severe trigeminal herpes with uveitis and keratitis. Treatment with antiviral medication usually leads to a good visual outcome for patients with trigeminal herpes, although they can develop late VZV dendriform keratitis, which can recur even with treatment.[4,5] Image courtesy of University of Michigan Kellogg Eye Center.
Involvement of which of the following areas is a good predictor for corneal ulceration?
A. Forehead
B. Eyebrow
C. Tip of nose
D. Temple
Answer: C. Tip of nose
The image shown demonstrates epithelial defects and melting of the cornea. The nasociliary nerve innervates both the tip of the nose and the cornea. Anterior uveitis and Hutchinson sign (a lesion of the tip of the nose) are highly predictive of visual loss. Patients presenting with these signs should be monitored closely for corneal ulceration. Image courtesy of C. Stephen Foster, MD, Massachusetts Eye Research and Surgery Institute, Harvard Medical School.
Anogenital lesions (shown) may be misdiagnosed as herpes simplex virus (HSV) infection, but the association with more severe neurologic complications suggests a diagnosis of zoster. Recurrent dermatomal eruptions in the genital area are more likely to represent HSV infection than herpes zoster, especially in immunosuppressed patients. Recurrent dermatomal vesicular or crusted skin lesions can indicate underlying herpetic meningitis or encephalitis, which also occur more commonly with immunosuppression. These patients may present with classic meningeal symptoms of headache, neck stiffness, and photophobia or encephalopathic delirium. Image courtesy of Brooke Army Medical Center.
This patient presented with acute pain that responded dramatically to oral corticosteroids at a dose of 1 mg/kg per day. Acute pain can be debilitating and may require the use of nonsteroidal anti-inflammatory drugs or narcotic analgesia. Some data suggest that treatment with oral antiviral agents with or without oral corticosteroids can shorten the duration of postherpetic neuralgia, a painful complication occurring in ~20% of patients with herpes zoster.[6] Established postherpetic neuralgia can be treated with topical capsaicin, oral gabapentin, or oral pregabalin. Severe acute pain or postherpetic neuralgia may require a nerve block.
This patient experienced debilitating postherpetic neuralgia that had a severe impact on his quality of life. Postherpetic neuralgia is a more common complication in patients older than 50 years.[2] A zoster vaccine, Zostavax, is now available in the United States. Studies have shown it to be safe and effective in reducing the occurrence of herpes zoster and thus the development of postherpetic neuralgia in older patients.[2,6] It is recommended for people older than 60 years.[1] New drugs for treating postherpetic neuralgia are in clinical trials; valomaciclovir seems to be more effective than its predecessors.[7] However, vaccination is the single most important strategy for the prevention of complications related to herpes zoster.
Contributor Information
Authors
Carly A. Elston
Medical Student
The Commonwealth Medical College
Scranton, Pennsylvania
Disclosure: Carly A. Elston has disclosed no relevant financial relationships.
Editor
Lars Grimm, MD, MHS
House Staff
Department of Diagnostic Radiology
Duke University Medical Center
Durham, North Carolina
Disclosure: Lars Grimm, MD, MHS, has disclosed no relevant financial relationships.

















 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 