
Migraine, a headache disorder, occurs in up to 15% of the overall U.S. population.1 In childhood, rates of migraine are similar between boys and girls. Migraine prevalence in women of reproductive age in the U.S. is more than twice that of men in the same age group. In both sexes, the rate of migraine declines rapidly after age 65 years.1
Hormonal changes from menarche through adulthood affect the intensity and timing of migraine attacks in females. Adolescents and women describe migraine attacks associated with menstruation as more severe, prolonged, and difficult to treat than migraines occurring at other times.2,3 Up to 60% of female migraineurs experience migraine around the time of menstruation (i.e., menstrual migraine).4 Pure menstrual migraine (without aura and occurring 2 days before and up to 3 days after start of bleeding) occurs in only 10% to 15% of these patients. In menstrually related migraine, the headache occurs without aura perimenstrually, and with or without aura at other times of the cycle.5-7 More than half of patients with menstrual migraine have attacks at other times of the month.5
Diagnosis of menstrual migraine is made if attacks take place perimenstrually in two of three monthly cycles.3,5 Menstrual migraine most often begins at menarche, frequently is alleviated during the second and third trimesters of pregnancy, and diminishes a year after menopause is established.1
Pathophysiology
No definitive mechanism of migraine has been elucidated. Current theory is based on a neurovascular mechanism wherein the sympathetic nervous system causes changes in cerebral perfusion.8 Evidence is mounting that menstrual migraine is influenced by alterations in the woman’s hormonal milieu throughout her life cycle.9
There are various ways in which the central nervous system may be impacted by ovarian hormones. Estrogen and progesterone receptors are expressed in the cortical and subcortical regions of the brain. Migraines can potentially be triggered by the serontonergic and opiatergic neurotransmitter systems, which are shown—at least in animal models—to be modulated by ovarian hormones.2,3
According to the estrogen withdrawal theory, a decline in estrogen concentrations—as occurs during the late luteal phase of the menstrual cycle—correlates to diminished serotonin production and increased elimination of estrogen. This may lead to the vasodilation of cranial vasculature and a sensitization of trigeminal nerves, which could trigger migraine in some women.8,9Maintenance of serum estrogen levels in the range of 45 to 75 pg/mL seems to reduce migraine frequency and intensity.9Prostaglandins released during the endometrial slough also may be involved in increasing migraine occurrence in the late luteal and early bleeding phases of the menstrual cycle.6
Pregnancy triggers an increase in plasma levels of estrogen and progesterone. In many women, migraines are alleviated during pregnancy, with the greatest relief occurring in women with menstrually related migraine. Migraine frequency lessens throughout the pregnancy, with the most alleviation taking place in the third trimester.8 In women who experience migraines with aura, attacks may present for the first time, stay the same, or worsen during pregnancy. During the postpartum period, women whose migraines were alleviated during pregnancy may experience continued relief while breastfeeding. This protection may be attributed to increases in oxytocin and vasopressin or to the suppression of estrogen and progesterone.8
The hormonal changes that occur during perimenopause and menopause may worsen menstrually related migraine. Women experience an increase in migraine prevalence during this phase of life. During perimenopause, estrogen levels are variable and often higher than those in regularly menstruating women. In addition, the number of estrogen receptors may increase. About a year after spontaneous menopause is established, migraines are less frequent and may disappear. This reduction is thought to be related to the fairly low, stable level of estrogen.8 Hormonally related migraine that occurs postmenopausally often is associated with hormone replacement therapy.2
Treatment and Prevention
The treatment of menstrual migraine can be challenging and may be specific to the patient because of increased, prolonged symptoms and resistance to therapy.8 The goal of treatment and prevention should be a reduction in headache burden.3 Initially, the patient should keep a headache diary for 3 months to help determine the migraine pattern (menstrually related or purely menstrual).2Triggers for menstrual migraine may differ from those for migraines occurring at other times. Most women will benefit from discovering and avoiding migraine triggers, maintaining good hydration, and getting regular exercise and sufficient sleep.3
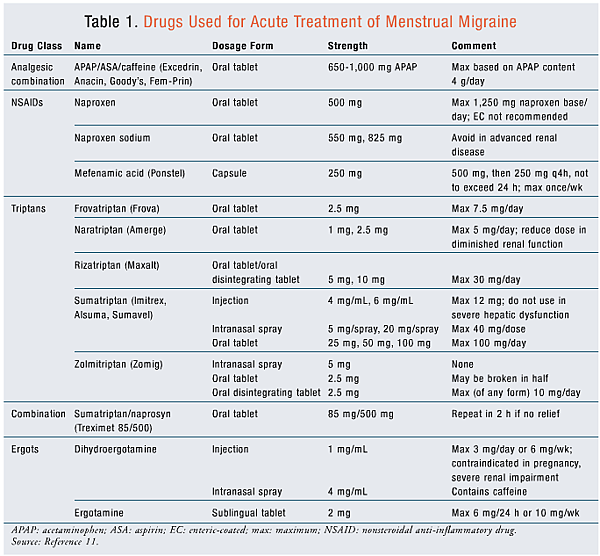
Acute pharmacologic therapies for menstrual migraine attacks are the same as those for migraines in general.10 Analgesics, ergots, and triptans (TABLE 1) have been used as abortive therapy in menstrual migraine.11 All are efficacious; however, drug choice and effective doses are patient specific, with varying percentages of response. Triptans have the best outcomes overall. The combination of a triptan with a nonsteroidal anti-inflammatory drug (NSAID) also is beneficial.12 Antinausea therapies may need to be added to increase the efficacy of therapy. Menstrual migraine may have a different regimen from attacks occurring at other times of the cycle.2,3
Prophylaxis: Prophylaxis should reduce the frequency, duration, and intensity of migraines of any source and reduce the need for abortive therapy.2 Short-term prophylactic therapy may benefit women who have a defined pattern of migraine associated with regular menstruation. Intermittent therapies reduce medication exposure and potential adverse effects expected with continued use. Premenstrual use of naproxen 500 mg twice daily with dosing extending to day 3 of menses has good tolerability and efficacy. Women experiencing nausea have been more likely to discontinue this regimen.2 Mefenamic acid 500 mg three times daily has also been shown to be effective.3
Triptans: Triptans have been used as short-term preventive therapy for menstrual migraine. They are dosed over 5 days: 2 days before menses is anticipated and 3 days into menses. Effective regimens are sumatriptan 25 mg three times daily, naratriptan 1 mg twice daily, frovatriptan 2.5 mg twice daily, and zolmitriptan 2.5 mg twice or thrice daily.3,10,13 These agents currently are not indicated to prevent pure menstrual migraine. Frovatriptan, which is effective for short-term prevention of menstrually related migraine, may have a pharmacokinetic advantage for menstrual migraine prophylaxis because of its prolonged half-life.13Naratriptan has demonstrated an increase in posttreatment headaches versus zolmitriptan or frovatriptan.10 Sumatriptan has been effective in open-label studies, but not randomized, controlled studies.10 Because of the increased costs associated with triptans versus analgesics, triptans should not be used first-line as prophylaxis. Daily use of triptans in the perimenstrual period reduces headache frequency and severity, but often requires the use of acute doses for breakthrough headache, and the maximum dosage still applies. Patients with prolonged, intractable attacks that are not relieved by acute therapy receive the most benefit from these agents.10
Supplements: Magnesium supplementation has been shown to reduce migraine symptoms in women with premenstrual syndrome.2Magnesium levels in the brain are low during migraine attacks, and reduced ionized magnesium levels have been proposed as a trigger for menstrual migraine.14 Magnesium supplements (360 mg elemental magnesium daily) taken during the last 15 days of the menstrual cycle have prevented attacks in some migraineurs. Gastrointestinal symptoms limit use in some patients.9
Vitamin E, which has antiprostaglandin effects, has limited efficacy in women with refractory migraine. In cases in which vitamin E had an effect, patients evidenced reductions in pain severity, functional disability, and NSAID doses when taking vitamin E 400 IU daily for 5 days perimenstrually.15
Estrogen Therapy: Because menstrual migraine has been linked to estrogen withdrawal, estrogen supplementation during the late luteal phase has been assessed for relief potential.16 Smoking, thromboembolic disorders, and estrogen-dependent tumors are contraindications to estrogen therapy.17 Hormonal prophylaxis has variable effects on migraine, and before estrogen therapy is begun the patient should be counseled on the possibility of worsening migraine attacks.3 The patient should keep a symptom diary for at least 2 months prior to and after initiating estrogen.
Low-dose oral contraceptives (OCs) may be tried in childbearing-age women with menstrual migraine who have other medical indications for continuous hormonal treatment. The candidate should not have a history of worsening symptoms with estrogen therapy or other contraindications. A regimen of OCs using a 91-day pack (or the equivalent) that has fewer days off estrogen could be followed, theoretically reducing rebound migraine attacks during those months.16
There has been some success using estrogen as intermittent therapy in the late luteal phase to relieve menstrual migraine. Percutaneous estradiol applied as a 1.5-mg gel patch on the upper thigh or arm 6 days prior to anticipated menstrual bleeding through day 2 reduced the number of migraine days. Withdrawal migraine during the 5 days following the end of therapy was a source of concern for patients, although the total number of headache days was reduced.7 Supplementation with a 0.1-mg estradiol patch during the hormone-free interval of combined hormonal OCs has some benefit in relieving withdrawal migraines.2 Combined OC use in women with migraine without aura is discouraged in the 2010 CDC report, especially in women aged more than 35 years and those who smoke, have hypertension, or are obese.18
No large-scale randomized trials have established increased risk of stroke from OC therapy in women aged less than 35 years who have migraine without aura and have no other risk factors.17,18 Symptoms should subside after a few months of OC use in patients who experience worsening of headaches. If not, OC or other estrogen-containing therapies should be stopped and alternative contraceptive methods considered.16
MacClellan and colleagues studied nearly 1,000 female subjects aged 15 to 49 years, one-third of whom had suffered a stroke. Risk of stroke was increased in subjects with migraine with aura but no other risk factors. In the migraine-with-aura group, smoking increased the risk. Smoking plus use of OCs increased the risk more than three times that in the smoking-only group. Migraine-without-aura subjects did not have the same increased risk of stroke.19
Long-Term Prophylaxis: Long-term prophylaxis should be instituted in women experiencing three or more debilitating headaches monthly who have not achieved relief with acute regimens.3 Standard prophylactic regimens may be tried, including anticonvulsants, beta-blockers, calcium channel blockers, and antidepressants. Dosage increases during the perimenstrual period may be of benefit.3Long-term hormonal supplementation has also been studied. Estradiol implants in doses that suppress fluctuations of serum estrogen may improve menstrual migraine.16 Several studies have examined the use of tamoxifen and gonadotropin-releasing hormone agonists to reduce migraine. Variable results, adverse effects, and tolerance limit the use of these agents.2,16
Perimenopause: Women may experience worsened or renewed migraine attacks during the perimenopausal period, which can last well over 5 years. An OC regimen or supplemental estrogen may be used.16 Erratic endogenous estrogen levels during this time may increase the uncertainty of exogenous dosing.3 Hormone replacement therapy (HRT) may have varied effects depending upon the route of administration, type of estrogen, and cyclical versus continuous administration. Transdermal preparations may be less likely to exacerbate migraine, but this has not been consistently shown.2,16 Progesterone supplementation may be effective for treating menstrual migraine by suppressing menstruation.7 In general, progesterone dosing does not seem to change migraine frequency, duration, or severity.16 Once menopause is established and the hormonal milieu is settled, migraine diminishes in frequency and many women cease having attacks.3
Pharmacist’s Role
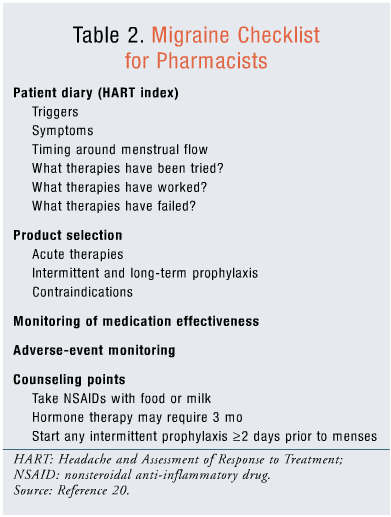
The pharmacist can help the patient determine triggers, symptoms, and timing of migraines. Helping determine the most appropriate treatment is important. The pharmacist can also counsel the patient and monitor for adverse events and medication effectiveness. See TABLE 2 for a checklist.20
Conclusion
Migraine in women often is associated with hormonal changes throughout the life cycle, from menarche to postmenopause. Hormonal changes, whether endogenous or exogenous, can be unpredictable. Many women experience more severe and debilitating migraines during menses than at other times. Menstrual migraine may be treated with acute therapies, intermittent prophylaxis, or long-term prophylaxis. Triptans may be used for acute or intermittent prophylaxis. Although these agents are highly effective, concerns exist regarding their cost. Hormone-based therapy for menstrual migraine can result in withdrawal headache, but is shown to decrease overall headache burden. Treatment choices should be individualized based on the patient’s needs regarding headache severity and frequency and on where she is in her life cycle, also taking into account contraception concerns or pregnancy.
REFERENCES
1. Victor TW, Hu X, Campbell JC, et al. Migraine prevalence by age and sex in the United States: a life-span study.Cephalalgia. 2010;30:1065-1072.
2. MacGregor EA. Prevention and treatment of menstrual migraine. Drugs. 2010;70:1799-1818.
3. Lay CL, Broner SW. Migraine in women. Neurol Clin. 2009;27:503-511.
4. IHS Classification ICHD-II. A1.1.2. Menstrually-related migraine without aura. http://ihs-classification.org/en/02_klassifikation/05_anhang/01.01.02_anhang.html. Accessed April 17, 2012.
5. IHS Classification ICHD-II. A1.1.1. Pure menstrual migraine without aura. http://ihs-classification.org/en/02_klassifikation/05_anhang/01.01.01_anhang.html. Accessed April 17, 2012.
6. Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis—part 1.Headache. 2006;46:3-23.
7. MacGregor EA. Oestrogen and attacks of migraine with and without aura. Lancet Neurol. 2004;3:354-361.
8. Gupta S, Mehrotra S, Villalón CM, et al. Potential role of female sex hormones in the pathophysiology of migraine.Pharmacol Ther. 2007;113:321-340.
9. Martin VT, Behbehani M. Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis—part 2.Headache. 2006;46:365-386.
10. Sullivan E, Bushnell C. Management of menstrual migraine: a review of current abortive and prophylactic therapies. Curr Pain Headache Rep. 2010;14:376-384.
11. Lacy CF, Armstrong LL, Goldman MP, Lance LL. Drug Information Handbook 2011-2012. 20th ed. Hudson, OH: Lexi-Comp; 2011.
12. Holland S, Silberstein SD, Freitag F, et al. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1346-1353.
13. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults; report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78:1337-1345.
14. Mauskop A, Altura BT, Altura BM. Serum ionized magnesium levels and serum ionized calcium/ionized magnesium ratios in women with menstrual migraine. Headache. 2002;42:242-248.
15. Ziaei S. Kazemnejad A, Sedighi A. The effect of vitamin E on the treatment of menstrual migraine. Med Sci Monit. 2009;15:CR16-19.
16. Loder E, Rizzoli P, Golub J. Hormonal management of migraine associated with menses and the menopause: a clinical review. Headache. 2007;47:329-340.
17. Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine. The International Headache Society Task Force on Combined Oral Contraceptives & Hormone Replacement Therapy. Cephalalgia. 2000;20:155-156.
18. U.S. medical eligibility criteria for contraceptive use, 2010. MMWR Morb Mortal Wkly Rep. 2010;59:1-86.
19. MacClellan LR, Giles W, Cole J, et al. Probable migraine with visual aura and risk of ischemic stroke: the Stroke Prevention in Young Women study. Stroke. 2007;38:2438-2445.
20. World Health Organization and European Headache Federation. Aids for management of common headache disorders in primary care. J Headache Pain. 2007;8:S1. www.who.int/mental_health/neurology/who_ehf_aids_headache.pdf. Accessed May 31, 2012.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 