A 62-year-old healthy woman presents for routine care. She has no history of fracture, but she is worried about osteoporosis because her mother had a hip fracture at 72 years of age. She exercises regularly and has taken over-the-counter calcium carbonate at a dose of 1000 mg three times a day since her menopause at 54 years of age. This regimen provides 1200 mg of elemental calcium per day. She eats a healthy diet with multiple servings of fruits and vegetables and consumes one 8-oz serving of low-fat yogurt and one glass of low-fat milk almost every day. She recently heard that calcium supplements could increase her risk of cardiovascular disease and wants your opinion about whether or not she should receive them. What would you advise?
THE CLINICAL PROBLEM
Both clinicians and patients are likely to be confused by the inconsistent and sometimes conflicting advice about the amount of calcium intake required to reduce the risk of fracture and, in particular, whether calcium supplements are necessary. Long-term calcium deficiency can clearly confer a predisposition to osteoporosis,1 but many persons mistakenly believe that postmenopausal and age-related bone loss and the associated increase in susceptibility to fracture can largely be avoided with the use of calcium supplementation. Although some persons remain at risk for calcium deficiency, other persons, particularly those receiving calcium supplements, may receive more than the recommended daily intake.
The complex and incompletely understood interaction between calcium and vitamin D intake complicates our understanding of the benefits and risks associated with either one alone.2,3 For example, a recent randomized trial showed that even high doses of vitamin D3 (4800 IU per day) had modest beneficial effects on calcium absorption (a 6% increase) among postmenopausal women with low serum levels of 25-hydroxyvitamin D.4 Furthermore, a number of clinical trials have studied the combination of calcium plus vitamin D in various doses, but fewer trials have examined the effects of calcium alone on the skeleton.
This review summarizes our current understanding of calcium intake as it relates to fracture risk and discusses concerns about the safety of calcium supplements. Other reviews have addressed the physiology of calcium metabolism and the ongoing controversies about vitamin D.2,5
KEY CLINICAL POINTS
Calcium Supplements and Fracture Prevention
-
The recommended dietary intake of calcium for women 19 to 50 years of age and men 19 to 70 years of age is 1000 mg per day; women older than age 50 and men older than age 70 require 1200 mg per day. Calcium intake above 2500 mg per day (2000 mg per day in persons >50 years of age) should be avoided.
-
Adequate calcium intake is important for skeletal health at all ages. Inadequate calcium intake in adults is common, particularly in men and women older than 70 years of age, and is associated with increased bone loss and an increased risk of fracture.
-
Consumption of calcium-rich foods and beverages is the preferred approach to ensuring adequate calcium intake. There is insufficient evidence to recommend routine calcium supplementation in community-dwelling adults, but supplements should be considered when dietary intake is inadequate.
-
Calcium supplements usually have few side effects, although constipation and bloating are common and nephrolithiasis occurs infrequently.
-
Recent studies have raised concern about an increased cardiovascular risk with the use of calcium supplements, but the findings are inconsistent and inconclusive.
Strategies and Evidence
Calcium Requirements
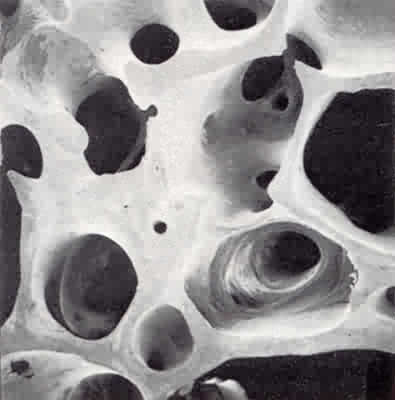
More than 98% of all calcium in the body is contained within the skeleton. Bone serves as a reservoir for calcium, which can be stored and released when needed. Calcium has at least two key physiological functions in adults: it is an intracellular messenger and it is a key component of hydroxyapatite, which is present in great quantities in the organic matrix of bone and provides strength and rigidity to the skeleton. Because of obligate losses in urine, sweat, and stool, insufficient calcium intake over a prolonged period may eventually affect important physiological processes.
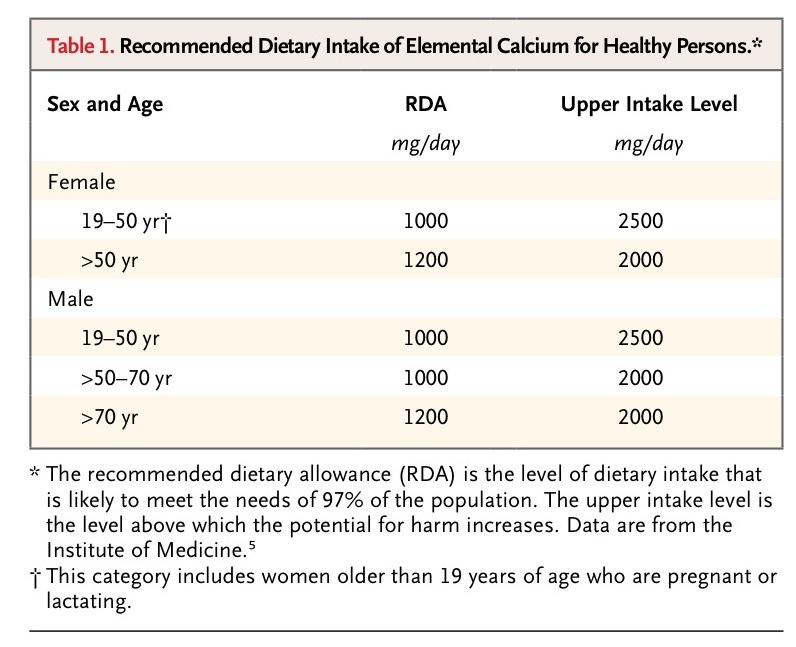
Primarily on the basis of studies of calcium balance in persons younger than 50 years of age and the known acceleration of bone loss that occurs with menopause and advanced aging, the Institute of Medicine (IOM) has issued guidelines regarding the dietary intake of calcium according to sex and age5(Table 1
).
The recommended calcium intake and the calcium content of various foods and supplements are quantified in milligrams of elemental calcium. Different supplement formulations provide different amounts of elemental calcium. The recommended dietary allowances are based on requirements for healthy populations. The recommended upper intake levels are based primarily on the risk of nephrolithiasis observed in studies of calcium supplementation in postmenopausal women. Calcium absorption is increased in pregnant and lactating women, but the recommended calcium intake for these women does not differ from that for other women in the same age group.
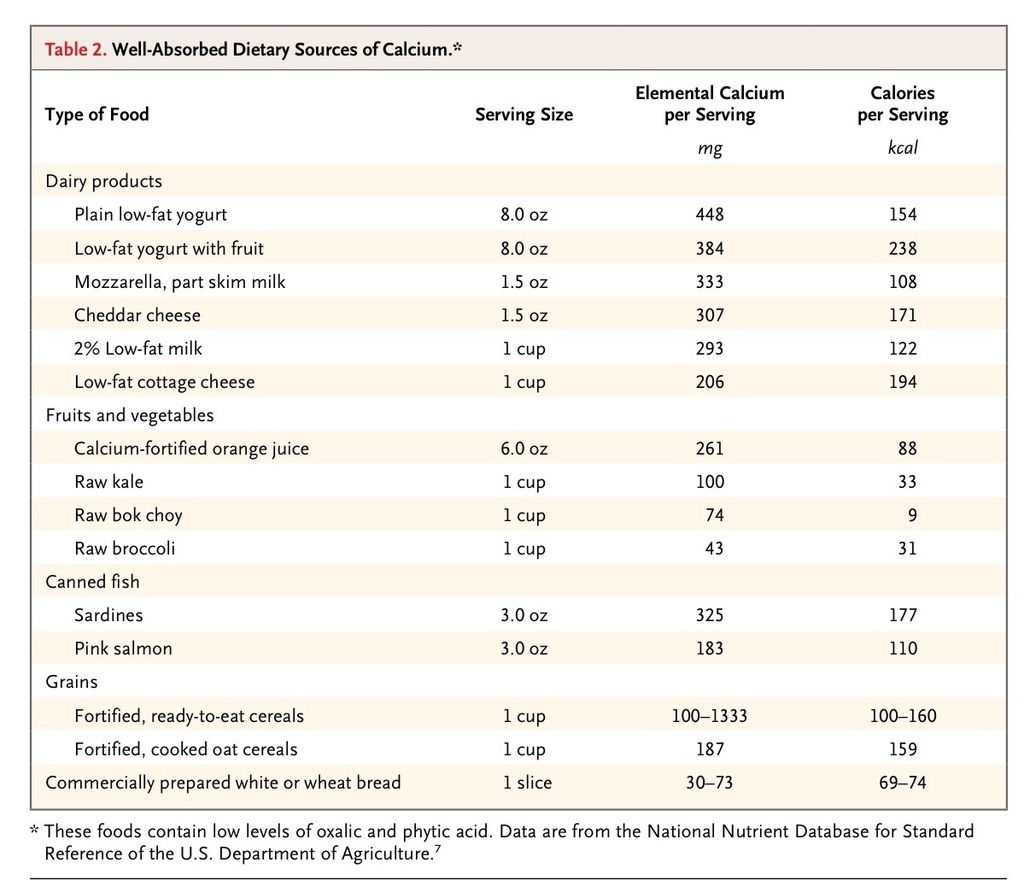
In a population-based study involving adults in the United States, the dietary intake of elemental calcium varied according to age group but averaged 900 to 1200 mg in men and 750 to 850 mg in women; the lowest intake was observed among men and women older than 70 years of age.6 More than 70% of dietary calcium comes from dairy products.5 To estimate a person's daily dietary calcium intake, clinicians can assume that most adults consume about 300 mg of calcium per day from nondairy sources (e.g., various vegetables and grains) and then estimate the total daily intake by calculating the additional daily intake of dairy products (Table 2
).
The use of calcium supplements is common; cross-sectional surveys have shown that 43% of U.S. adults (and almost 70% of postmenopausal women) regularly take calcium supplements.8 Despite frequent use of calcium supplements, many adults in the United States, particularly postmenopausal women, do not consume the recommended 1000 to 1200 mg of elemental calcium per day, and few consume more than the recommended upper intake level of 2000 to 2500 mg per day.
Dietary Calcium versus Calcium Supplements
In general, calcium-rich foods and beverages, particularly dairy products, are the preferred sources of calcium because they are widely available, and with the exception of lactose intolerance, they are associated with few adverse effects. Some evidence suggests that a greater proportion of ingested calcium is absorbed from certain dietary sources such as broccoli and kale than from calcium supplements.5 Although data involving clinical outcomes (fractures) are lacking, physiological studies suggest no material differences in the metabolic actions of dietary calcium as compared with calcium obtained from supplements.9,10 Therefore, the decision about whether or not to receive supplements depends on the adequacy of dietary calcium intake and the balance between the potential benefits and harms of supplements. The safety and side-effect profile of calcium supplements are described below.
Calcium supplements are available over the counter; labels commonly include both the total milligrams of calcium salt and the milligrams of elemental calcium in each tablet. Determination of the dose required to meet daily calcium requirements is based on the amount of elemental calcium. Commonly used preparations include purified calcium carbonate, calcium citrate, and, to a lesser extent, calcium lactate and calcium gluconate; preparations differ in the amount of elemental calcium provided (Table 3
).
Calcium carbonate provides relatively high elemental calcium content (40%) and is inexpensive and widely available. As compared with other calcium supplements, calcium carbonate is more likely to cause constipation and bloating11 and should be taken with meals, since gastric acidity is required for sufficient absorption. As compared with calcium carbonate, calcium citrate provides less elemental calcium (21%), but it is a reasonable alternative in patients with bothersome gastrointestinal symptoms; it may be taken with or without meals, since absorption is not dependent on gastric acidity. If daily supplementation with more than 500 mg of elemental calcium is required, divided doses are recommended to improve absorption and minimize gastrointestinal side effects.
Potential Benefits of Calcium Intake
Perimenopausal and age-related bone loss, and the accompanying increased risk of fracture, occur when there is a net loss of calcium in the skeleton due to an imbalance between bone resorption and bone formation. Although perimenopausal bone loss is primarily related to the loss of estrogen, age-related bone loss in both men and women is determined by genetic, hormonal, and other factors. Observational studies suggest that bone loss and fracture risk increase when calcium intake is below 700 to 800 mg per day.1,12 Conversely, the effect of additional calcium intake on bone loss among persons who do not have a calcium deficiency is less clear and is probably modest.13
Many trials have assessed the antifracture benefits of calcium supplements, but most, such as the Women's Health Initiative (WHI) Calcium/Vitamin D Supplementation trial, included vitamin D as part of the intervention and did not preferentially recruit persons with low dietary calcium intake.14 The WHI trial did not show a significant reduction in hip fractures or other fractures in women randomly assigned to 1000 mg of elemental calcium plus 400 IU of vitamin D per day as compared with women assigned to placebo, perhaps because the mean calcium intake in the placebo group was 1154 mg per day.15However, pooled analyses of the combination of calcium plus vitamin D have suggested a modest protective effect on fractures, particularly among frail and elderly persons.16,17 For example, a meta-analysis of 16 placebo-controlled trials of calcium and vitamin D supplements (including the WHI trial) recently performed for the U.S. Preventive Services Task Force showed an overall 12% reduction in the risk of any fracture.16 In this analysis, the benefits of calcium and vitamin D with respect to fracture risk were significant among institutionalized persons (relative risk, 0.71; 95% confidence interval [CI], 0.57 to 0.89) but not among community-dwelling persons (relative risk, 0.89; 95% CI, 0.76 to 1.04) (P=0.07 for interaction). Fewer trials have specifically examined the skeletal effects of calcium supplements alone, but a meta-analysis that pooled the results of 9 randomized trials of calcium supplements alone (involving a total of 6517 persons) showed that the overall reduction in fractures was 10%.17Conversely, a pooled analysis of 3 trials of calcium alone showed an unexpected 50% increase in the risk of hip fracture.18 Thus, current evidence suggests that supplementation with calcium and vitamin D or with calcium alone has a modest overall effect on the risk of fracture, and whether or not routine use of supplements is beneficial for community-dwelling persons remains uncertain.
Potential Harms of Calcium Intake
Although calcium supplements have few side effects, minor constipation and dyspepsia are common. The risk of nephrolithiasis is increased with the use of calcium supplements (the relative risk was 1.17 in the WHI trial),19 and the risk appears to be dose-dependent.20 Conversely, in observational studies, a higher dietary intake of calcium has been associated with a lower risk of nephrolithiasis, perhaps because of a reduction in the intestinal absorption of oxylate.21 Early studies suggested that the use of calcium supplements might increase the risk of prostate cancer among men, but a recent meta-analysis that included more than 4000 cases of prostate cancer showed no association with the use of calcium supplements.16
Several studies have raised concerns about a possible increase in cardiovascular risk associated with calcium supplementation. A meta-analysis of published results of 15 placebo-controlled trials of calcium supplements without vitamin D showed an increased risk of myocardial infarction among persons randomly assigned to calcium (odds ratio, 1.31; 95% CI, 1.02 to 1.67).22 The authors speculated that transient supplement-related increases in serum calcium levels18 might precipitate arrhythmias or perhaps promote vascular calcification. This meta-analysis received considerable attention but was criticized because of inconsistent adjudication of events, marginal statistical significance, and exclusion of trials assessing calcium plus vitamin D. Among the trials not included in this meta-analysis was the WHI trial,14 which involved more than 36,000 women and showed no significant increase in adjudicated cardiovascular events23 or overall mortality24 among women who received calcium plus vitamin D. In a subsequent meta-analysis, the same investigators included data from trials of calcium plus vitamin D, including some of the WHI trial data,25 but they still excluded WHI participants who were receiving calcium supplements at baseline (approximately 54%14,23); the pooled summary estimate of the risk of myocardial infarction associated with supplementation in this updated analysis yielded similar results (odds ratio, 1.21; 95% CI, 1.01 to 1.44). The exclusion was based on the argument that a risk associated with supplements might be obscured among these women if it was attributable to abrupt changes in plasma calcium concentrations after the consumption of supplements. This approach has been subject to criticism and to considerable debate.26-30 A 2010 meta-analysis31 that included all participants in the WHI trial showed no significant relationship between supplementation and cardiovascular events in pooled analyses of 2 trials of calcium plus vitamin D (relative risk, 1.04; 95% CI, 0.92 to 1.18) or in 3 trials of calcium supplements alone (relative risk, 1.14; 95% CI, 0.92 to 1.41). In another placebo-controlled trial of supplementation with calcium carbonate (1200 mg of elemental calcium per day) involving 1460 older women (mean age, 75 years),32 calcium supplementation did not result in an increase in the risk of death or atherosclerotic events requiring hospitalization (identified through a validated registry) over a follow-up period of 5 years.
Observational studies have also yielded conflicting results.33-41 For example, whereas two large, prospective cohort studies showed that the use of calcium supplements was associated with an increased risk of cardiovascular events or death,33,34 a large Canadian prospective cohort study35 and the extended follow-up of the WHI trial36 showed no significant association between the use of calcium supplements and cardiovascular events. Several studies have shown no relationship between higher dietary intake of calcium and adverse cardiovascular outcomes.33-35,37-39 In contrast, a recent study involving a Swedish cohort showed that, as compared with women with intakes between 600 and 999 mg per day, rates of death from cardiovascular causes and death from any cause were higher among women with a dietary or total calcium intake of 1400 mg per day or more but there was no increased risk with intakes of 1000 to 1399 mg per day.40 Neither the prospective Framingham Heart Study41 nor the WHI trial42 showed a relationship between the use of calcium supplements and the coronary calcium score.
In summary, the evidence suggesting adverse cardiovascular effects of calcium supplementation is inconsistent, and an accepted biologic explanation is lacking; the clinical significance of transient supplement-related increases in serum calcium levels is unknown. However, pending further data, a reasonable approach is to preferentially encourage dietary calcium intake and discourage the routine use of calcium supplements.
Patient Education
Patients who can consume dairy products without adverse effects should be encouraged to regularly consume them along with other foods that have a high calcium content (Table 2). Since calcium fortification of processed food and beverages is variable, labels must be checked carefully to determine the calcium (and caloric) content per serving and the serving size. For persons who are unable to meet recommended daily calcium requirements with dietary intake alone, calcium supplementation should be discussed; the side-effect profile (Table 3) and cost should be considered in choosing a supplement.11Supplement dosing combined with dietary intake should be sufficient to approximate but not exceed the IOM daily guidelines.
Areas of Uncertainty
Further research is needed to determine whether clinically important differences exist between formulations of calcium supplements with respect to skeletal benefits and potential side effects and to establish calcium requirements for premenopausal women, men, and nonwhite populations.43 In addition, data from randomized trials that include systematic collection and adjudication of cardiovascular events are needed to clarify whether calcium supplementation increases cardiovascular risk.
Guidelines
The IOM has issued guidelines for daily dietary calcium intake in children and adults (Table 1).
An expert panel convened in 2011 by the American Society for Bone and Mineral Research found that the evidence was insufficient to conclude that calcium supplements cause cardiovascular events.44
In a 2013 update,45 the U.S. Preventive Services Task Force found insufficient evidence to assess the benefits and harms of daily supplementation with more than 1000 mg of calcium (or more than 400 IU of vitamin D) for the primary prevention of fractures in noninstitutionalized postmenopausal women. However, the task force cited the negative results of the WHI trial and recommended against routine daily supplementation with 1000 mg or less of calcium or 400 IU or less of vitamin D. They found insufficient evidence to recommend for or against the use of calcium supplements in men and premenopausal women. Although the authors of the recommendation statement acknowledged the importance of adequate calcium intake for skeletal health, they did not address supplementation specifically in persons with inadequate dietary intake.
CONCLUSIONS AND RECOMMENDATIONS
The healthy postmenopausal woman described in the vignette reports a current total daily intake of 2240 mg of elemental calcium: a dietary intake of about 1040 mg (approximately 300 mg from nondairy sources and 740 mg from dairy products) and supplements that provide 1200 mg of calcium. Since her calcium intake is substantially greater than the IOM recommendation of 1200 mg per day for postmenopausal women, I would recommend that she increase her dietary calcium intake by 200 mg per day and discontinue her calcium supplements. If increasing her dietary intake is not feasible, she can reduce her calcium carbonate supplementation to one 500-mg tablet each day. She should be informed that supplement use, but not increased dietary intake, modestly increases the risk of nephrolithiasis, and she should be advised about a potential increased risk of cardiovascular events, although the evidence of the latter is currently inconsistent and inconclusive. If she continues to supplement her dietary calcium intake, she should be advised to take calcium carbonate with meals to optimize absorption.






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 