The US Food and Drug Administration (FDA) announced today the approval of ipilimumab (Yervoy, Bristol-Myers Squibb) for the treatment of advanced melanoma as a second-line therapy.
Ipilimumab is the first agent ever proven to improve survival in advanced melanoma. Its Biologics License Application was granted priority review designation in August 2010.
Melanoma is the leading cause of death from skin disease. An estimated 68,130 new cases of melanoma were diagnosed in the United States during 2010, and about 8700 people died from the disease, according to the National Cancer Institute.
"Late-stage melanoma is devastating, with very few treatment options for patients, none of which previously prolonged a patient's life," said Richard Pazdur, MD, director of the Office of Oncology Drug Products in the FDA's Center for Drug Evaluation and Research. Ipilimumab "is the first therapy approved by the FDA to clearly demonstrate that patients with metastatic melanoma live longer by taking this treatment."
The pivotal study of ipilimumab, known as 020, was conducted in previously treated unresectable stage III or stage IV melanoma patients. Results from this study made headline news when they were presented at last year's meeting of the American Society of Clinical Oncology (ASCO) and then published in full (N Engl J Med. 2010:363;711-723), as previously reported by Medscape Medical News.
In that study, patients receiving ipilimumab plus a peptide vaccine (glycoprotein 100) had a median survival of 10 months, compared with 6.4 months for patients receiving the vaccine alone (P < .001). Patients receiving ipilimumab alone had a nearly identical median survival — 10.1 months — in the 3-group clinical trial (P < .003).
The response to ipilimumab can be "dramatic," said Patrick Hwu, MD, from the University of Texas M.D. Anderson Cancer Center in Houston, in an editorial that accompanied the study (N Engl J Med. 2010;363:779-781).
Follow-up from the earliest cohort of patients who received ipilimumab "shows that ongoing complete responses in some patients with metastatic melanoma can continue past 6 years," said Dr. Hwu wrote.
However, on the downside of the data from the 676-patient study, the "best overall response rate" (patients with a complete or partial response) was limited to 10.9% of the ipilimumab recipients. In other words, a minority of patients respond to the new drug.
Nevertheless, experts have predicted great patient demand for the new drug, as reported by Medscape Medical News.
Bristol-Myers Squibb announced on March 21 that ipilimumab is also effective in previously untreated patients with metastatic melanoma.
In the new study, designated 024, ipilimumab met the primary end point of improving overall survival in these patients, according to the company. The study compared ipilimumab in combination with chemotherapy (dacarbazine) and chemotherapy alone.
An abstract of the 024 data will be submitted for potential presentation at the annual ASCO meeting in June, the company reports.
New Class of Drug
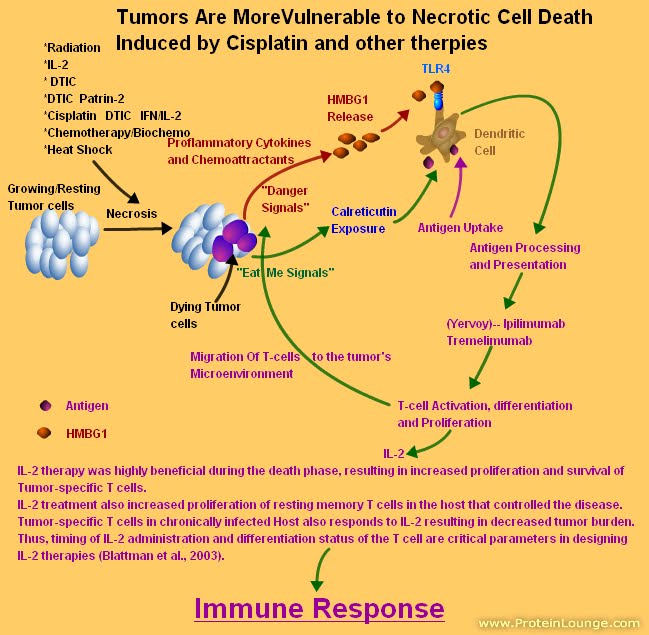
Ipilimumab is another targeted therapy for cancer, but represents a new class of drug, known as a targeted T cell antibody, said Steven O'Day, MD, one of the study authors, when the study was first presented last year. Ipilimumab is directed against an antigen on the surface of T cells. The antigen, cytotoxic T lymphocyte–associated antigen 4 (CTLA-4), acts as a brake on the T cell, explained Dr. O'Day, who is from the University of Southern California Keck School of Medicine in Los Angeles. By blocking the brake, the T cell goes into attack mode and kills cancer cells.
In the pivotal study, treatment with ipilimumab, which is administered intravenously, included some severe adverse events, including 14 deaths.
"This is a powerful drug," said Dr. O'Day, who noted that 10% to 15% of immune-related adverse effects were grade 3 or 4 and required immunosuppressive therapy with steroids.
"Steroids were quite successful in the vast majority of patients," said Dr. O'Day, "and they did not affect efficacy."
The "serious potentially life-threatening complications" with ipilimumab require a committed multidisciplinary team to manage them, explained Vernon Sondak, MD, from the H. Lee Moffitt Cancer Center in Tampa, Florida, who acted as a discussant of the study at ASCO in 2010.
The FDA noted in its approval announcement that the common adverse effects that can result from autoimmune reactions associated with ipilimumab use include fatigue, diarrhea, skin rash, endocrine deficiencies (gland or hormone), and inflammation of the intestines (colitis). Severe to fatal autoimmune reactions were seen in 12.9% of patients treated with ipilimumab. When severe adverse effects occurred, the drug was stopped and corticosteroid treatment was started. Not all patients responded to this treatment. Patients who did respond in some cases did not see any improvement for several weeks.
Because of the unusual and severe adverse effects associated with ipilimumab, the therapy is being approved with a Risk Evaluation and Mitigation Strategy to inform healthcare professionals about these serious risks. A medication guide will also be provided to patients to inform them about the therapy's potential adverse effects.
Dr. O'Day reports serving in a consultant or advisory role for and receiving honoraria and research funding from Bristol-Meyers Squibb, and receiving research funding from Medarex. Dr. Sondak reports being a speakers bureau member and providing consulting and expert testimony for Merck/Schering-Plough; he is also on advisory panels for Bristol-Myers Squibb, Genzyme, GlaxoSmithKline, Pfizer, and Provectus. Dr. Hwu has disclosed no relevant financial relationships.
不介意的話,也可以參考一下我的機轉圖,在最左上角
圖解藥理學 13抗腫瘤藥物10.2






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 