Question
Why are cefazolin and vancomycin being used for surgical prophylaxis by cardiothoracic, vascular, and orthopedic surgeons?
Response from Michael Postelnick, BPharm
Lecturer, Department of Medical Education, Northwestern University Feinberg School of Medicine; Senior Infectious Disease Pharmacist; Clinical Manager, Northwestern Memorial Hospital Department of Pharmacy, Chicago, Illinois
With the publication of "Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery" by the American Society of Health-System Pharmacists, Infectious Diseases Society of America, Surgical Infection Society, and Society for Healthcare Epidemiology of America,[1] practitioners have access to comprehensive, evidence-based recommendations for preprocedural antimicrobial prophylaxis. Unfortunately, definitive evidence is lacking in the majority of surgical procedures due to the low rate of infection and the relatively small sample sizes in clinical trials. This is particularly the case when attempting to compare the relative efficacy of 2 different prophylactic antimicrobial regimens.
In these situations, decisions are often made by considering likely pathogens based on local epidemiology and susceptibility patterns as well as the potential catastrophic nature of an infection if it occurs. While cefazolin remains the mainstay of antimicrobial prophylaxis in most surgical procedures, there is a growing propensity to combine cefazolin with vancomycin in a number of procedures where postoperative infections may be serious or life-threatening. Although it would appear that there would be little gain from combining these 2 agents for use in surgical prophylaxis, there is some rationale for doing so.
1. Spectrum of activity and likely pathogens
Cefazolin provides activity against a wide variety of pathogens associated with surgical-site infections, including methicillin-sensitive Staphylococcus aureus (MSSA), streptococci, and some gram-negative organisms such as Escherichia coli. Vancomycin provides activity against potential gram-positive pathogens such as methicillin-resistant S aureus (MRSA), coagulase-negative staphylococci, and enterococci that cefazolin may not be routinely active against. If indicated by the epidemiology of surgical-site infections at a given institution, particularly if both MRSA and gram-negative organisms are potential pathogens, the combination of these 2 antimicrobials may be a reasonable strategy.
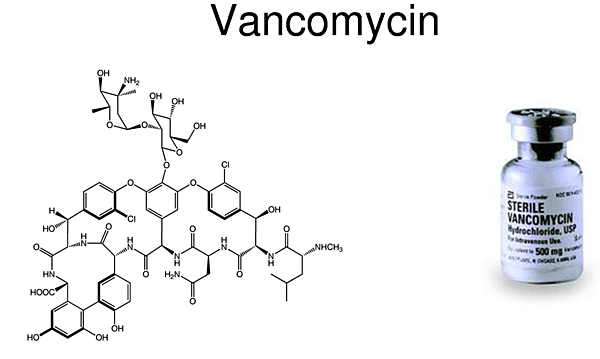
2. Mechanism of action
Beta-lactam antimicrobials have consistently proven to be more active and clinically effective against MSSA than vancomycin for both prophylaxis and treatment of infection.[1-3] In situations where the epidemiology of surgical-site infections includes both MSSA and MRSA, the combination of cefazolin and vancomycin likely provides better activity and potential protection against surgical-site infections than just vancomycin alone.
機轉也可以參考這邊:
3. Timing of administration
Administering prophylactic antimicrobials within the appropriate window (within 1 hour of incision) prior to a surgical procedure has been demonstrated to decrease the rate of surgical-site infections.[1] While cefazolin can be administered either by intravenous (IV) push or rapid IV infusion over 20-30 minutes, vancomycin must be infused slowly, over 1-2 hours. This complicates achieving the above stated goal. The administration of cefazolin by rapid infusion or IV push ensures adequate concentrations of antibiotic at the surgical site and coverage of all but a select few pathogens in situations where the necessity of prolonged infusion of vancomycin may preclude the administration of the full dose prior to incision.
Due to the fact that any infection associated with a cardiac, vascular, or orthopedic (particularly orthopedic implant) procedure can result in significant morbidity and potential mortality, close attention to adequate surgical prophylaxis administered at the appropriate time prior to the surgical procedure is important to minimize the risk for such an occurrence. The combination of cefazolin plus vancomycin for these high-risk procedures may provide a rational alternative. This combination is not indicated in all situations, and the decision for use should be made on an institution- and procedure-specific basis predicated on the epidemiology of surgical-site infections encountered when these procedures are undertaken in the given institution.
References
-
Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195-283. Abstract
-
Bull AL, Worth LJ, Richards MJ. Impact of vancomycin surgical antibiotic prophylaxis on the development of methicillin-sensitive Staphylococcus aureus surgical site infections: report from Australian Surveillance Data (VICNISS). Ann Surg. 2012;256:1089-1092. Abstract
-
Schweizer ML, Furuno JP, Harris AD, et al. Comparative effectiveness of nafcillin or cefazolin versus vancomycin in methicillin-susceptible Staphylococcus aureus bacteremia. BMC Infect Dis. 2011;11:279.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 