Abstract
Combined hormonal contraceptives [combined oral contraceptives (COCs)] have been available for over 50 years and the impact of this invention may not be overestimated. Today over 100 million women are current users and in Western Europe and the United States approximately 80% of women of fertile ages can be considered as ever-users. Over the years several drawbacks have been identified and media alarms on risks are frequently presented, resulting in suboptimal compliance and low compliance and continuation rates. Poor compliance and discontinuation is a big problem and is not generally identified by prescribers. During ideal use COCs offer very good protection against unwanted pregnancies, however there is a big problem with compliance and continuation and thus the 'real-life' efficacy is much lower. Reasons for poor compliance include side effects and fear of side effects and it is crucial that the prescriber gives the individual woman thorough and balanced information on the benefits and risks. Most well known is the increased risk of venous thromboembolism, but also an elevated risk of arterial thrombosis and several types of cancer has been reported. The risk estimates are low but according to the large number of users a substantial number of extra cases will occur. However, use of COCs also offers several additional health benefits with significant impact on morbidity and quality of life. COC use is associated with a substantial decrease in the risk of ovarian cancer, endometrial cancer and colorectal cancer. Moreover, COCs are a major option of treatment for women suffering from heavy menstrual bleeding and dysmenorrhea as well as hirsutism and acne vulgaris. The net effect of the additional health effects of COC-use may very well be positive, i.e. a slight increase in life expectancy
Background
The oral contraceptive pill, 'the pill', was introduced in the beginning of the 1960s and the significance of this invention may not be overestimated. For the first time in history, the woman herself had the possibility to control her own fertility. The English magazine The Economist described the pill as 'one of the seven wonders of the modern world' and 'the one invention that historians a thousand years in the future will look back on and say: "That defined the 20th century"' [The Economist, 1999].
Rapidly after the introduction of the pill, a huge number of women became users; however, over time several health concerns became evident, but there was also evidence of additional health benefits. Presently, worldwide about 100 million women are current users of combined hormonal contraceptives, most frequently used in the western world [United Nations, 2007]. Moreover, approximately 80% of all women in, for example, the US can be considered as ever-users [Guttmacher Institute, 2013]. This might make hormonal contraceptives one of the most commonly used prescription drugs in the world
The combined oral contraceptive pill (COC) was discovered more or less by accident. During the first human trial, in Puerto Rico in 1956, the initial progestin products were contaminated with mestranol, a synthetic estrogen. When the products were purified and the estrogen content was lowered, the result was breakthrough bleeding and it was decided to retain the estrogen for cycle control thus establishing the principle of the combined estrogen–progestin oral contraceptive [Speroff and Darney, 2011].
The Estrogen Component
Estradiol (E2) is the most potent natural estrogen and is the major estrogen secreted by the ovaries. However, estradiol is low potency when given orally. The addition of an ethinyl group at the 17 position, ethinylestradiol (EE), makes the molecule highly orally active. The addition of the ethinyl group also changes the properties of the molecule making EE far more potent than E2 as EE does not bind to sex hormone-binding globulin (SHBG), is resistant to enzymatic degradation by 17-beta-hydroxylas and has a higher affinity for the estrogen receptor [Sitruk-Ware and Nath, 2013].
The major serious side effect of COC use, venous thromboembolism (VTE), is related to estrogen and the estrogen dose [Böttiger et al. 1980]. The dose of estrogen therefore is a critical issue. Over the years a successive decrease in estrogen dose has occurred and modern pills contain 15–30 μg EE. The metabolism of EE varies significantly both between individuals and within the same individual [Goldzieher, 1990].
Since the 1970s, strong efforts have been made in order to develop a COC with estradiol as the estrogen component. The major obstacle has been poor bleeding control. However, this problem now seems to have been solved in two different ways. First, using a four-phasic regimen with estradiol and dienogest (half-life 9 hours) and second using estradiol in combination with nomegestrolacetate, a progestin with a marked long half-life (46 hours). Consequently, there are now at least two different COCs available with estradiol as the estrogen component. These formulations minimize the risk of break-through bleeding but the bleeding pattern differs from the EE pill as a substantial number of users will be amenorrhoic [Mansour et al. 2011; Fraser et al. 2011].
The Progestin Component
Progesterone has low bioactivity and low oral potency. In 1951 Carl Djerassi and coworkers demonstrated that removal of the 19-carbon from ethisterone to form norethindrone changed the major hormonal effect from that of an androgen to that of a progestational agent [Djerassi et al. 1951]. The groups of progestogens derived from testosterone were accordingly designated as 19-nor-testosterones, denoting the missing 19-carbon. The androgenic properties of these compounds, however, were not totally eliminated and minimal, but sometimes clinically significant, androgenic potential may remain. Over the years new progestogens have been developed in order to minimize the androgenic effects. New 'members' of the 19-nortestosterone family as well as progestogens derived from spirolactone and progesterone are now available [Sitruk-Ware, 2005, 2008] (Table 1).
| Progesterone derivate | 19-nor-testosterones | 17-α-spirolactones |
|---|---|---|
| Chloromadinone acetate | Norethindrone | Drospirenone |
| Cyproterone acetate | Norethynodrel | |
| Medroxyprogesterone acetate | Levonorgestrel | |
| Nomegestrol acetate (NOMAC) | Desogestrel | |
| Nestorone | Etonogestrel | |
| Trimegestone | Norgestimate | |
| Norelgestromin | ||
| Gestodene | ||
| Dienogest | ||
| Lynestrenol |
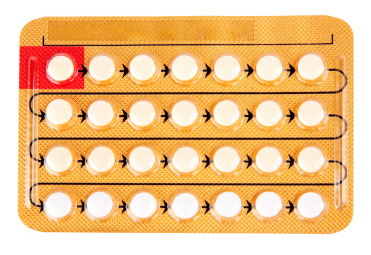
Formulations
The traditional COCs consist of 21 active pills with the same dose of estrogen/progestin, i.e. a monophasic pill followed by a 7-day pill-free interval, so called 21/7 pills. Three-phasic pills with a gradual increase in progestin dose were introduced in order to mimic 'natural cycles' and to minimize androgenic effects by creating a more 'estrogen-dominated' pill with a more pronounced raise in SHBG concentrations. However, only slight metabolic effects of questionable clinical importance have been the result and three-phasic pills do not seem to have any major advantages compared with monophasic regimens. On the other hand, different contents in different pills may cause problems for the user when it comes to missed pills or a wish for continuous use. The relatively new pill containing E2V/dienogest, on the other hand, is even a four-phasic pill. In this specific case, this regimen is a prerequisite for achieving bleeding control and maintained efficacy.
During the 21st century the obvious trend is abandoning the 21/7 regimen in favor of a 24/4 monophasic regimen. This is a consequence of a desire to maintain bleeding control and ovarian suppression despite lower doses of the pill. Data shows that a 24/4 regimen yields a more enhanced ovarian suppression with less follicular growth and consequently a slight but significantly higher efficacy [Dinger et al. 2011]. Moreover, the 24/4 regimen seems do reduce menstrual blood loss [Mansour et al. 2011; Christin-Maitre et al. 2011] and to diminish cycle-related symptoms such as headache, bloating and breast tenderness [Sulak et al. 2000].
Combined hormonal contraception is also available as a patch (EE/norelgestromin), a vaginal ring (EE/etonogestrel) and as injectables. One patch is used for one week. After use of three patches, one 'patch-free' week follows and a withdrawal bleeding will occur. The vaginal ring should be used for 21 days and followed by a seven-day ring-free interval. Combined hormonal injectables are administered once a month (for example, depo-medroxyprogesteroneacetate/E2cypionate).
Prescribing Patterns
Approximately fully 100 million women are presently current users of COC worldwide. The use varies widely over the world being most common in Western Europe, the United States and Northern Europe [United Nations, 2007]. In the US 17% of all women 15–45 years old use COC which corresponds to 27.5% of all contraceptive users [Guttmacher Institute, 2013]. In Western Europe the corresponding figures are 40–50% whereas only 7% of all women use COCs in Africa with big regional differences in prevalence. The same pattern is seen also in Asia.
The contraceptive patch is relatively commonly used in the US and the ever-use has increased from less than 1% in 2002 to 10% in 2006–2010. Also the vaginal ring is most commonly used in the western world although still quite uncommon. Only 6% of the women in the US had used the contraceptive ring in 2006–2010, the first time this method was included in surveys [Guttmacher Institute, 2013]. Combined injectables are most frequently used in China, South-East Asia and South America.
There is a huge number of different combinations of COCs concerning both compounds and doses. In a review of COC use in the United States, Stridham Hall and Trussell could show that almost 80 different formulations of COC were used [Stridham Hall and Trussell, 2012]. The prescription pattern differs between different parts of the world but also between different countries. This is partly due to different interpretations of safety data but traditions also play a part. In the US, COCs with norgestimate and drospirenone are the most commonly used and also triphasic pills are quite commonly used [Stridham Hall and Trussell, 2012]. In Europe, the European Medicines Agency (EMA) in 2001 recommended second-generation COCs, i.e. levonorgestrel containing COCs, monophasic, as the first choice because of the data indicating a lower risk of VTE in this group of users compared with users of third-generation pills (COC containing desogestrel or gestodene). This statement was confirmed in 2013 [European Medicines Agency, 2013] where it was concluded that also drospirenone containing COC implied a higher VTE risk (Table 3).
Consequently, levonorgestrel COC are more commonly used in Europe although there are big variations between countries. For example, levonorgestrel containing COCs constituted almost 57% of all first-time prescriptions in 2005–2010 in Sweden compared with approximately 5% in Denmark during the same period [Josefsson et al. 2013; Wilson et al. 2012].
Compliance/Continuation Rates
When COCs were first marketed in the beginning of the 1960s, many expected that all future pregnancies would be planned pregnancies. Although COC are nearly 100% effective if taken daily, a 9% typical use failure rate during the first year of use reflects the fact that pills are frequently missed [Trussell, 2011]. In fact, surveys from around the world have reported that as many as 60% of COC users report irregular use [Potter et al. 1996]. In the United States in 1995, 15.5% of COC users reported missing one pill and another 13.3% reported missing two or more pills in the past 3 months [Abma et al. 1997].
The reasons for poor adherence and discontinuation, leading to contraceptive failure, have been reported to be side effects as well as the fear of side effects. The reported side effects include mood disturbances, decrease in libido, weight gain and poor bleeding control, and the fear of side effects also includes the risk of VTE [Lindh et al. 2009; Larsson et al. 2007].
Most of these reported side effects can be attributed to the progestogen component of the pill. Consequently, new progestogens with the potential of a more beneficial profile concerning side effects have been developed. Despite these improvements, the discontinuation rates during the first 6 months of use are still high (20–25%) [Josefsson et al. 2013].
There is only sparse evidence of differences in continuation rates between different types of hormonal contraceptives. The type of progestogen [Lawrie et al. 2011; Maitra et al. 2004] and the number of oral contraceptive pill packages dispensed [Foster et al. 2006], prescription drug or over-the-counter [Potter et al. 2011] have all been proposed as determinants for continuation. Improvements of formulations of combined hormonal contraception, including new routes of administration and different regimens, that is, monophasic, biphasic, triphasic and quadriphasic pills, patches and vaginal rings, have been performed in order to increase compliance and continuation [Sucato et al. 2011; Murphy and Brixner, 2008], but, so far, there is only limited evidence that use of a specific formulation or route of administration would be a better choice concerning continuation rates.
Most studies are hampered either by design or by the involvement of pharmaceutical companies, and the results must therefore be interpreted with caution [Lawrie et al. 2011; Maitra et al. 2004].
A Swedish register study found no difference in overall continuation rates between different COCs after first-time prescription but use of all COCs showed higher continuation rates than progestin-only pills [Josefsson et al. 2013].
Long-cycle use, also called extended cycle use, means that the woman uses the COCs without interruption and consequently no monthly bleeding will occur. This will lead to amenorrhea. Most women do not require the periodic experience of monthly bleeding and it is not necessary for the woman using COCs to experience a monthly withdrawal bleeding. The continuous regimen can be used with any monophasic COCs [Edelman et al. 2006; Archer et al. 2006] or using the patch or the vaginal ring. In the latter cases, the user will just continue to leave out the patch-free/ring-free interval and continue use. A continuous regimen provides a greater ovarian suppression reducing the potential for breakthrough bleeding [Archer et al. 2009]. The absence of a pill-free interval also reduces symptoms associated with menstruation such as dysmenorrhea, menstrual pain and bloating. All of these positive effects may increase the probability of compliance and continuation. Robinson and colleagues in 1992 showed that COC users who experienced other positive effects of their use were more likely to continue use [Robinson et al. 1992]. Despite these facts, many prescribers are unaware of this option [Seval et al. 2011; Frederick et al. 2011].
On the other hand, compliance with any method relying on the woman's remembrance seems to be rather low and there is a wide discrepancy between the efficacy during ideal and typical use. The use of long-acting reversible contraception (LARC), i.e. intrauterine contraception and implants, on the other hand, is not affected by forgetfulness and the ideal and typical use is similar and consequently also the efficacy.
There still is a great need for studies emphasizing continuation/discontinuation of COC and the following risk of unintended pregnancies.
Prescriptions Under Special Circumstances
Adolescents often have an irregular lifestyle, difficulties in assessing risk of unintended pregnancy and consequently run a high risk of contraceptive failure and unintended pregnancies. Winner and coworkers [Winner et al. 2012] showed that among users of pills, patches, or rings, those who were less than 21 years of age had a risk of unintended pregnancy that was almost twice as high as the risk among older women. Studies from the USA show a different prescription pattern of COCs in adolescents. COCs containing drospirenone, and the contraceptive patch, seem to be more frequently prescribed in teenagers [O'Brien et al. 2008]. However, adolescents may be even more susceptible to contraceptive failure due to missed pills and poor compliance than older women according to the high fertility in this age group. Promoting LARC may be an option with a great potential of success and is recommended by the American College of Obstetricians and Gynecologists [American College of Obstetricians and Gynecologists, 2012].
Also following an abortion, LARC may be a better option than COCs. Several studies have shown lower rates of repeated abortions in women using LARC after the index abortion [Heikinhemo et al. 2008; Langston et al. 2014] compared with women on COCs. An unintended pregnancy during COC use should be regarded as contraceptive failure and the woman should be recommended use of another, more effective method following the abortion. LARC is most often the method of choice in a woman who has become pregnant during COC use.
Despite the widespread belief, there are no substantial effects of COC use on weight. No excessive weight gain has been observed [Gallo et al. 2014] and no definite relation between weight and contraceptive efficacy has been established [Westhoff et al. 2010]. Data have indicated a decreased resorption of COC after bariatric surgery [Paulen et al. 2010] but so far, no studies of pharmacokinetics after bariatric surgery using modern surgical procedures have been performed.
Additional Health Benefits
Cancer
Much attention has been paid to the possible increase in cancer risk, i.e. breast cancer and cervical cancer, but the net effect of COC use on cancer risks seem to be positive. The results from the UK general practitioners study [Hannaford et al. 2007] concluded a 12% decrease in overall cancer risk in a group of women followed for almost 40 years and a recent systematic review of the associations between COC use and cancer found that the overall net effect of current patterns of oral contraceptive use on deaths from noncontraceptive outcomes is positive, with reductions in mortality from ovarian, colorectal, and endometrial cancers [Havrilesky et al. 2013].
Ovarian Cancer
卵巢癌
Almost all studies that have studied the relationship between COC use and ovarian cancer have reported a decreased risk in COC ever-users. In 2008, Beral and coworkers presented a large systematic review concerning this matter [Beral et al. 2008]. The study included 23,257 cases and 87,303 controls. Users of modern low-dose COCs were also included. They found a significant reduction of overall ovarian cancer risk [relative risk (RR) 0.73; 95% confidence interval (CI) 0.70– 0.76] with an additional 20% reduction for every 5 years of use. These results have recently been confirmed [Havrilevsky et al. 2013] (Table 2). Moreover, the effect lasted at least 30 years after discontinuation [Beral et al. 2008]. This protective effect was also evident in BRCA1 and BRCA2 carriers [Havrilevsky et al. 2013].
Endometrial Cancer
子宮內膜癌
A huge mass of studies concerning COC ever use and protection of endometrial cancer exist. The results are consistent regarding a substantial protective effect [Gierisch et al. 2013; Schlesselmann, 1997; Mueck et al. 2010]. The total reduction of cases varies between studies. The reduction is 40– 50% depending on the duration of use. As is the case with COC use and ovarian cancer, the protective effect seems to last after the period of use, for at least 20 years [Mueck et al. 2010; Weiderpass et al. 1999]. These results have been confirmed in a meta-analysis of studies from the 21st century [Gierisch et al. 2013] RR 0.57 (95% CI 0.43– 0.77); see Table 2.
Colorectal Cancer
大腸癌
Also, the incidence of colorectal cancer is reduced in COC ever users [Bosetti et al. 2009; Fernandez et al. 2001]. A meta-analysis from 2013 [Gierisch et al. 2013] concerning studies performed after 1999 found an odds ratio (OR) of 0.86 (95% CI 0.79–0.95) and thus the previously described risk reduction could be confirmed. Moreover, this meta-analysis found a significant effect of duration of use: the longer the women had used COC, the greater was the effect (Table 2).
Menstrual Blood Loss
Heavy menstrual bleeding (HMB) and dysmenorrhea frequently complicates life for a substantial number of women. Prevalence rates for HMB range between 4% and 52%, with rates reported in studies based on subjective perception of the heaviness of menstruation tending to be higher than those where blood loss was objectively assessed [National Collaborating Centre for Women's and Children's Health, 2007]. About 1 in 20 women aged 30–49 years in England and Wales consult their general practitioner for HMB in any given year. Use of COCs has a consistent positive impact on work productivity and activities of daily living.
Modern low-dose COCs are as effective as older high-dose formulations in reducing menstrual flow [Milsom et al 1990; Larsson et al. 1992]. Blood loss has been reported to be reduced by almost 90% in users of E2/dienogest [Fraser et al. 2011; Jensen et al. 2011] and the use has a consistent positive impact on work productivity and activities of daily living in women with HMB [Wasiak et al. 2012]. COC use also has a significant impact on the occurrence and severity of dysmenorrhea [Milsom et al. 1990; Harada et al. 2008].
Ovarian Cysts
Studies with long-time use of high-dose formulations reported significant reductions of both corpus luteum cysts and functional ovarian cysts [Vessay et al. 1987]. Epidemiologic studies have indicated a decline in the incidence of ovarian cysts proportional to the steroid doses in COCs [Lanes et al. 1992; Holt et al. 1992]. Current low-dose COCs offer no protection against functional ovarian cysts [Lanes et al. 1992; Holt et al. 1992], but a protection against corpus luteum cysts seems most likely following the inhibition of ovulation.
Acne
Use of COCs induces an increase of the synthesis of SHBG by the liver and this increase occurs regardless of preparation [Odlind et al. 2002]. This increase in SHBG results in an increased androgen-binding capacity which results in a decrease in free testosterone levels. Consequently, use of COCs will improve acne regardless of which product is used [Rosen et al. 2003].
| Studied relation | Reference | Type | Level of evidence | Material | Main findings | Relative risk (95% confidence interval) |
|---|---|---|---|---|---|---|
| Use of COC in relation to risk of epithelial ovarian cancer | Beral et al. [2008] | Meta-analysis | 2 | 23,257 cases 87,303 controls | • Decreased risk in COC ever users • A more pronounced effect by duration of use |
0.73 (0.70–0.76) |
| Havrilesky et al. [2013] | Systematic review/meta-analysis | 657,055 women, 3,981,072 women years | • The protective effect lasts at least 30 years after use | 0.73 (0.66–0.81) | ||
| Hannaford et al. [2007] | Prospective cohort | 2 | 46,000 women 744,000 women years 17,032 women, 540,000 women years |
• Decreased risk in COC ever-users • A more pronounced effect by duration of use |
0.54 (0.40–0.71) | |
| Vessey and Painter [2006] | Prospective cohort | • The protective effect lasts at least 15–20 years | 0.5 (0.3–0.7) | |||
| Use of COC in relation to endometrial cancer risk | Gierisch et al. [2013] | Systematic review/meta-analysis | 2 | 308,198 women | • Risk reduction among COC ever-users • The effect lasts at least 20 years |
0.57 (0.43–0.77) |
| Use of COC in relation to colorectal cancer risk | Gierisch et al. [2013] | Systematic review/meta-analysis | 2 | 2,969,189 women years | • Risk reduction in COC ever-users • Big variation between studies • No established relation between duration of use and effect |
0.86 (0.79–0.95) |
| Use of COC in relation to breast cancer risk | Gierisch et al. [2013] | Systematic review/meta-analysis | 2 | 317,341 women | • Small increase in risk during current use • The increased risk declines and disappears 10 years after cessation |
1.08 (1.00–1.17) |
| Collaborative Group on Hormonal Factors in Breast Cancer [1996] | Systematic review/meta-analysis | 2 | 53,297 cases 100,239 controls | • The increased risk is highest among young users | 1.24 (1.15–1.33) | |
| Use of COC in relation to cervical cancer risk | Appleby et al. [2007] | Systematic review/meta-analysis | 2 | 16,573 cases 35,509 controls | • Increased risk in current users • The increased risk declines and disappears 10 years after cessation |
≥5 year 1.9 (1.69–2.13) |
| Longatto-Filho et al. [2011] | Prospective cohort | 2 | 12,114 women | • Presence of Hr-HPV was related to risk | No independent increased risk in COC users No trend if used <5 years; use 5–9 years: 2.82 (1.46– 5.42); use >10 years 4.03 (2.09–8.02) |
|
| Gierisch et al. [2013] | Systematic review/heterogeneity made meta-analysis impossible; pooled data from study of good quality | 2 | 1561 cases 1916 controls | • Increased risk only in Hr-HPV positive women |
Hr-HPV, high-risk human papillomavirus.
Risks
Venous Thromboembolism
VTE is the most common serious complication associated with COC use, known since the end of the 1960s. The VTE risk is an effect of the estrogen component. There is a clear relationship between the magnitudes of the risk in relation to the estrogen dose down to 20 μg EE. A number of studies have addressed differences in VTE risk between different formulations according to the progestogen component of the pill. The risk seems to be higher for users of preparations with newer progestogens, i.e. desogestrel, gestodene and drospirenone. This is most probably due to differences between progstogens in their capacity to balance an estrogen-dependent VTE risk and not an effect of the progestogen by itself. The risk of COC-associated VTE is highest during the firsts 3 months of use [Dinger et al. 2010b].
Recent data indicates that the risk in an unexposed population is higher than previously described and the annual incidence of VTE in this group is now considered to be 2–3 per 10,000. A huge number of studies have investigated the relative risk of VTE during COC use and risk estimates of 2–10 have been reported.
Factors Associated With an Increased VTE Risk
There are both hereditary and acquired risk factors for VTE and they may enhance the risk alone or in combination. These factors must be taken into account during contraceptive counselling and the prescription of COCs. The use of different biochemical marker, for example the factor V Leiden mutation, have been extensively discussed but as the predictive value of a positive test is very low there is no general recommendation to test. Also a positive family history has a low predictive value [Grimes et al. 2012] but can be used as a simple screening method.
Family History of VTE. A positive family history of VTE is three times more common in women with VTE than in controls [Cosmi et al. 2003]. Thrombophilia are more common with a positive family history. A meta-analysis found that the combination of COCs and factor V Leiden mutation yielded a relative risk of VTE of 17 [Dayan et al. 2011]. Consequently, women with a positive family history of VTE should not be recommended to use COC.
Acquired Risk Factors. The risk of VTE increases with age [Nightingale et al. 2000; Bergendahl et al. 2012]. A healthy, normal weight woman can be prescribed COC also during the ages 40–49 years but other potential risk factors must always be evaluated in relation to the age of the individual.
A woman with a history of VTE should not use COCs according to the high risk of a relapse [Hansson et al. 2000].
Obesity is a well-known risk factor of VTE [Nightingale et al. 2000; Bergendahl et al. 2012] and the increase in risk is about threefold. This increase is approximately of the same magnitude in COC users. However, the risk in obese women using COCs in relation to normal weight women without COCs has been reported to be 10–24 times higher. This increase in risk must be related to the even more pronounced risk during pregnancy but also to the nonexisting risk increase associated with progestin-only methods and intrauterine contraception. Therefore, if possible, an obese woman in the first place, should not be recommended COCs.
Immobilization and trauma are well-known risk factors for VTE. The use of anticoagulants decrease the risk but there is a lack of studies with reference to this risk in relation to COC use.
The risk for VTE is increased during surgery in premenopausal women (RR 5) [Bergendahl et al. 2012]. The duration and the localization of the procedure are important. Surgery on the lower extremity implies a higher risk. Treatment with anticoagulants is recommended in COC users. The recommendation of discontinuation of COC 4–6 weeks prior to elective surgery is widely used but there is a lack of information on the consequences of this kind of recommendation. There are also uncertainties, with this recommendation, when the use of combined hormonal contraceptives should be restarted after surgery. Moreover, it has been shown that repeated restart of COC use increase the VTE risk in the individual. Consequently, this method should not be recommended.
During the last 15 years there has been an intense debate regarding the clinical impact of the studies concerning differences in VTE risk between users of COCs with different progestogens. A majority of case-control studies undertaken have shown an approximately double VTE-risk for so-called third- and fourth-generation COCs containing desogestrel, etonogestrel, gestodene or drospirenone compared with the risk associated with the second-generation COCs containing levonorgestrel, norethisteron or norgestimate [Lidegaard et al. 2012]. However, in prospective cohort studies no differences were found except for the increased risk in the nonexposed population [Dinger et al. 2007, 2010a]. During the autumn 2013, however, the European Medical Agency [European Medicines Agency, 2013] pointed out that the benefits with COCs still out-weighed the risks but that the second-generation pills should be used in the first place because of a probable lower VTE risk. The matter of compliance must always be taken into consideration when choosing the optimal contraception for the individual.
Arterial Thrombosis: Myocardial Infarction and Stroke
Modern COCs containing less than 50 μg of EE do not increase the risk of myocardial infarction or stroke in healthy, nonsmoking women regardless of age [WHO, 1996, 1997; Margolis et al. 2007; Yang et al. 2009]. However, if hypertension is present, the woman may run an increased risk and thus COC use should be avoided in women with hypertension.
Migraine headache is common in women and is associated with an increased risk of ischemic stroke. If the migraine headache is with aura, use of COC implies an additional risk (RR 7.0; 95% CI 1.5–32.7) [Schürks et al. 2009].
Cancer
Although premenopausal breast cancer is rather uncommon, it is the most common cancer in women of fertile ages. The risk is, however, very low in the ages where COC-use is most prevalent, under the age of 30. Several factors for breast cancer reflect the lifetime exposition of female sex hormones, which makes the question of COC use and breast cancer highly relevant.
The knowledge today is to a large extent still based on the findings from the meta-analysis performed by the Collaborative Group on Hormonal Factors in Breast Cancer [Collaborative Group on Hormonal Factors in Breast Cancer, 1996], a meta-analysis of 53,297 cases and 100,239 controls. The main findings in this study was that current users had a slightly increased risk (RR 1.24; 95% CI 1.15–1.33) and that this small increase disappeared 10 years after cessation. The risk for young users, under 20 years old, was slightly higher. There were, however, some inconsistency in the results as COC users, despite the increased risk of breast cancer, to a lower extent had advanced disease. Different sources of bias have been discussed, for example surveillance bias.
During the last 10 years a huge number of new studies have been published. In a recently published systematic review and meta-analysis 44 studies could be identified [Gierisch et al. 2013]. A total of 23 of these could be included in a meta-analysis. The included studies also embrace third-generation COCs. Briefly, a very small, just significant, increase in risk was found during ongoing use [odds ratio (OR) 1.08; 95% CI 1.00– 1.17]. No relation was found between risk and duration of use (OR 0.95; 0.83–1.09). Like the collaborative group study, the risk vanished 10 years after cessation. The results from the collaborative group were thus confirmed, i.e. a statistically significant but small increase in risk during ongoing use. Interpreted to absolute terms, however, this increase will lead to few extra cases as the incidence during these ages is very low.
Women with a family history of breast cancer have been studied without any demonstrated risk elevation in these groups [Colditz et al. 1996; Grabrick et al. 2000; Silvera et al. 2005]. In BRCA1 and BRCA2 carriers it has not been able to draw any definite conclusions regarding the effects of COC use on breast cancer risk. Results show both increased and decreased risk and the interpretations have been hampered by different populations, different design and different control groups [Cibula et al. 2010]. The net effect for this group may, however, be positive as BRCA1 and BRCA2" carriers have a substantial risk of ovarian cancer where COC use offers protection [Havrilevsky et al. 2013].
A significant increased risk for cervical cancer has been reported in association with COC use of more than 5 years. As is the case with the COC-use-associated risk for breast cancer, the risk of cervical cancer also disappears within 10 years after cessation. Recent analyses have not revealed an independent relationship between COC use and cervical cancer. The risk seem to be related to the presence of high-risk human papillomavirus (Hr-HPV) [Appleby et al. 2007; Longatto-Filho et al. 2011].
Conclusion
The invention of the oral contraceptive pill has certainly meant a revolution to women and society. The possibility for the woman herself to control her fertility cannot be overestimated. However, a prerequisite for this effect is that the woman uses the pill in the way it is intended. We have learned that it is easy to overestimate compliance and continuation rates. Many women discontinue use because of side effects and the fear of side effects. Proper and balanced information is crucial for compliance and should be based on facts and knowledge, not on opinions. In addition to the obvious benefit of avoiding unwanted pregnancies, the positive side effects of COC may overwhelm the risks and use of COC may in fact increase life expectancy [Havilevsky et al. 2013].
Conclusion
The invention of the oral contraceptive pill has certainly meant a revolution to women and society. The possibility for the woman herself to control her fertility cannot be overestimated. However, a prerequisite for this effect is that the woman uses the pill in the way it is intended. We have learned that it is easy to overestimate compliance and continuation rates. Many women discontinue use because of side effects and the fear of side effects. Proper and balanced information is crucial for compliance and should be based on facts and knowledge, not on opinions. In addition to the obvious benefit of avoiding unwanted pregnancies, the positive side effects of COC may overwhelm the risks and use of COC may in fact increase life expectancy [Havilevsky et al. 2013].





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 