Kiran Panesar, BPharmS (Hons), MRPharmS, RPh, CPh
Consultant Pharmacist and Freelance Medical Writer
Orlando, Florida
US Pharm. 2011;36(9):56-61.
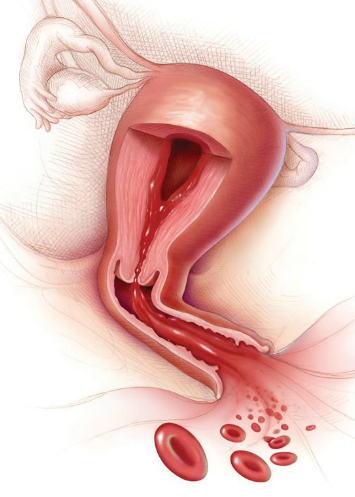
Excessive uterine bleeding may be cyclical or noncyclical.1 Average menstrual blood loss varies between 30 and 40 mL per cycle, the upper limit being 60 to 80 mL per cycle.1 Menorrhagia is heavy cyclical bleeding that occurs when menstrual blood loss exceeds 80 mL per cycle, and it is the most common gynecologic complaint.2 It is distinctive from excessive noncyclical bleeding. While many women may subjectively complain of excessive menstrual bleeding, data suggest that in fact around 30% of women of reproductive age experience menorrhagia.3,4 Furthermore, it is well established that normal menstrual loss increases with age, especially in perimenopausal women.5
MECHANISM
The normal menstrual cycle is the result of the interaction of estrogen, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH). At different times of the cycle, one or more of these hormones result in proliferation, differentiation, and necrosis of the endometrium, resulting in menstrual bleeding. The whole cycle can be divided into three phases: the follicular phase, the ovulatory phase, and the luteal phase.
FSH and LH released by the anterior pituitary stimulate the development of follicles and production of estradiol—the follicular phase. The elevated estrogen levels induce the proliferation of the endometrial lining through a negative feedback mechanism on FSH production. It also causes an increase in LH, which results in ovulation—the ovulatory phase. Once the oocyte is released from the mature follicle, the remaining corpus luteum releases progesterone. This prepares the lining of the endometrium for implantation. If that does not occur, the corpus luteum disintegrates and hormone levels fall—the luteal phase. This causes a breakdown of the endometrial lining and hence menstruation. The fall in estrogen and progesterone levels stimulates the production of FSH and LH levels through a negative feedback mechanism, and the cycle is repeated.6
Anything that causes thickening of the endometrium, and hence increases its vascularization, can cause menorrhagia. Menorrhagia may be idiopathic or as a result of underlying disorders such as tumors and endocrine or hormonal disorders.7 The most common symptom experienced by hemophiliac women is menorrhagia, and 5% to 24% of women with menorrhagia also have von Willebrand’s disease.1,8In addition to increased age, premenopausal leiomyomata, also known as uterine fibroids, and endometrial polyps are risk factors for menorrhagia.1
TREATMENT OPTIONS
Appropriate treatment should be initiated following a thorough history, examination, and investigation. Drug treatment is normally the first mode of management for patients with no underlying cause of menorrhagia. The options available are both nonhormonal and hormonal, and the choice of drug should take into account the amount of bleeding, any associated pain, existing conditions, and potential side effects of treatment (TABLE 1).3,7 Drugs include oral or intrauterine treatments, and surgical procedures are sometimes an option.
Perimenopausal women suffering from menorrhagia may, with sufficient information and support, opt for watchful waiting, although symptoms worsen with age.9 Many women with menorrhagia become anemic due to excessive blood loss. The anemia needs to be managed appropriately with iron supplements.10
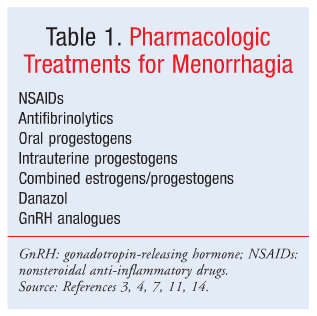
Nonsteroidal Anti-inflammatory Drugs
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) in the management of menorrhagia is based on the finding that the level of prostaglandins in the endometrium of women who suffer from excess loss of blood during menses is higher than in normal women.7Furthermore, elevated levels of nitric oxide enhance the production of prostaglandins via the cyclooxygenase (COX) pathway through a positive feedback mechanism.3 NSAIDs work by inhibiting COX enzymes and have been shown to be more effective than placebo at reducing blood loss.7 Since NSAIDs are less effective but also associated with fewer side effects than tranexamic acid, danazol, or the levonorgestrel-releasing intrauterine system (LNG-IUS),7 they are a particularly suitable option for milder menorrhagia or menorrhagia associated with pain.
While no one NSAID has been shown to be superior to another, studies have demonstrated that mefenamic acid or naproxen taken for 5 days starting at the onset of bleeding can reduce blood loss by 45%.4 Typical doses are 250 to 500 mg two to four times a day for mefenamic acid and naproxen and 600 to 1,200 mg/day for ibuprofen.3,4 Since NSAIDs are commonly associated with gastrointestinal (GI) side effects, they are contraindicated in women with peptic ulceration.11
Antifibrinolytics
The endometrium of women who experience menorrhagia has been shown to have higher levels of plasminogen activators than that of women with normal flow.4 Plasminogen activators are a group of enzymes that trigger fibrinolysis when they are in close proximity to plasminogen and fibrin.4,12 Lysine residues are made available when fibrinogen is converted to fibrin. The plasminogen binds to the lysine residues via lysine binding sites and is converted to plasmin by the plasminogen activator. Fibrin is degraded to smaller fragments by plasmin.12
Tranexamic acid is a synthetic lysine derivative that exerts its effect by blocking lysine binding sites on plasminogen, thus preventing fibrin degradation.4,12 Clinical trials have demonstrated that tranexamic acid is more effective at reducing blood loss in menorrhagia than mefenamic acid, flurbiprofen, and oral luteal phase norethisterone.10 If used over several cycles, it can reduce bleeding by up to 60%.3
The normal recommended dose of tranexamic acid is 1 to 1.5 g three to four times daily for 3 to 4 days initiated on the day heavy menstrual bleeding begins.12 The dose needs to be reduced in patients with renal failure due to the risk of accumulation.12
Tranexamic acid is also associated with GI side effects including nausea, vomiting, diarrhea, and dyspepsia, as well as disturbances in color vision.12 Since these adverse effects are dose dependent, they can be reduced by decreasing the number of days for which the drug is taken.4 Patients on tranexamic acid also run the risk of developing deep venous thrombosis (DVT), and its use is contraindicated in patients with a history of thromboembolic disease.12-14
While not as effective as LNG-IUS, tranexamic acid is a well-tolerated nonhormonal option for the management of menorrhagia that cannot be controlled by NSAIDs. Data on the use of tranexamic acid in women with bleeding disorders is still limited.13
Hormonal Treatments
Oral Progestogens: Oral progestogens, such as medroxyprogesterone, are the most commonly used medications for the management of menorrhagia.1 In women with anovulatory cycles, progestogens help coordinate shedding when given in days 15 to 26 of the cycle.4However, in those with normal ovulatory cycles, their use is yet to be established. Administration of cyclical progestogens from days 15 to 26 of the cycle offers no greater efficacy than danazol, tranexamic acid, NSAIDs, or LNG-IUS.4,15 It has been shown that oral progestogens given on days 5 to 26 of the menstrual cycle effectively reduce menstrual blood loss, but less than LNG-IUS.1 A typical dose of medroxyprogesterone would be 2.5 to 10 mg daily by mouth for 5 to 10 days starting on the assumed or calculated 16th to 21st day of the menstrual cycle.11
Oral progestogens are associated with irregular bleeding, headaches, and breast tenderness.1,4 The severity of these is based upon the dose and duration of the treatment.4 However, since these agents have few contraindications, they can be used to safely treat older women who smoke, women who present with risk factors for thromboembolic disease, and those who suffer from conditions that increase the risk for heart attack or stroke.3
Oral progestogens may be the drug of choice in patients with anovulatory cycles and useful in the short-term treatment of menorrhagia in patients with normal ovulatory cycles.1,15 Doses as high as 30 mg daily have been used to impede torrential bleeding.
Intrauterine Progestogens: The levonorgestrel intrauterine system (LNG-IUS), commonly used as a contraceptive, has shown significant benefit over oral progestogens that are given over days 5 to 26 in the reduction of menstrual blood loss.1 Recent reports have shown a reduction of menstrual blood loss by up to 96%.16 The side-effect profile is generally lower and the patient satisfaction higher in patients using an intrauterine device (IUD).1 The IUD progestogens provide therapeutic concentrations of hormone release that result in endometrial atrophy but minimize side effects.3,16 A typical device delivers a dose of 20 mcg of levonorgestrel every 24 hours in a sustained-release formulation that lasts up to 5 years.1
Patients using LNG-IUS may experience frequent and variable bleeding and spotting.1 Any pain experienced during insertion can be alleviated with the use of NSAIDs. LNG-IUS has the added advantage of providing effective contraception and may alleviate the symptoms of dysmenorrhea and reduce the incidence of pelvic inflammatory disease.1 These devices are also a suitable alternative to a hysterectomy, particularly in patients who wish to preserve fertility, and they offer rapid reversibility.1,17
Combined Estrogens/Progestogens: Studies have shown that the combined oral contraceptive pill provides some control over the menstrual cycle and thins the endometrium. The evidence is primarily practice based; there are insufficient trials to compare this form of treatment to other options available for the control of menorrhagia.1,18 The combination might be useful in women who require control of bleeding as well as a form of contraception.3 Since there is a risk of thromboembolism, the oral contraceptive pill is not the preferred method of controlling menstrual blood loss. For the same reasons, it is contraindicated in patients with predisposing factors or a previous history of thromboembolism.1 In addition, combined oral contraceptives may cause hypertension, reduced glucose tolerance, changes in lipid metabolism, and impaired liver function.11
Danazol: Danazol works by suppressing the pituitary-ovarian axis and inhibiting the pituitary output of gonadotropins, hormones that increase in the endometrium.11,19 It is a chemical derivative of testosterone that inhibits ovulation and reduces estrogen levels.19Danazol is more effective than placebo and NSAIDs but less effective than surgical procedures at reducing menstrual blood loss. Its efficacy as compared to the combined oral contraceptive pill, oral progestogens, and the LNG-IUS has not yet been established.10 So far, the most acceptable dose in terms of efficacy and adverse effects is 200 mg once daily.20
While danazol is effective at reducing menstrual blood loss, there is insufficient evidence to support its use in the management of menorrhagia.1,19 This is compounded by the fact that danazol can produce adverse androgen effects resulting in male-like symptoms together with weight gain and acne.19 Hence, danazol is not the treatment of choice for the management of excessive menstrual blood loss.
Conversely, since danazol has the ability to significantly increase the hemoglobin and serum ferritin levels, it may find its place in the management of menorrhagia in women who are anemic.19 However, the mechanism by which this is achieved and the importance of this effect have not yet been established.11 Danazol use can also result in irritability, musculo-skeletal pain, hot flushes, breast atrophy, and, when used for long periods of time, liver disorders.19 It is considered a second-line therapy for the management of excessive blood loss.
Gonadotropin-Releasing Hormone (GnRH) Analogues: GnRH analogues are competitive agonists at GnRH receptors in the pituitary. GnRH-releasing cells are eventually desensitized, resulting in a hypogonadotropic state, which causes hypoestrogenism, endometrial atrophy, and amenorrhea.20
There is not much evidence to support the use of GnRH analogues in the management of menorrhagia.21 To add to this, GnRH analogues are associated with a number of adverse effects that limit their use.21 They have been known to cause bone demineralization of up to 5% in women taking them for over 6 months.20 This adverse effect can be reversed upon the discontinuation of treatment.11Other side effects, also associated with the loss of estrogen, include hot flushes, night sweats, vaginal dryness, dyspareunia, and loss of libido.20
While they do not have a reliable contraceptive effect, one study showed that the addition of the GnRH analogue goserelin to a low-dose contraceptive provides effective control of heavy menstrual bleeding.22 An earlier study demonstrated that goserelin is a practical and safe treatment in the management of menorrhagia and severe anemia in women with leiomyomata uteri.23 Overall, GnRH analogues are considered second-line therapy in the treatment of menorrhagia.20
Surgical Options
As a last resort, women suffering from menorrhagia may opt for surgical procedures. First-generation procedures are performed with a hysteroscope and require general anesthesia, whereas second-generation procedures are blind techniques performed without a hysteroscope (TABLE 2). Both techniques offer similar rates of symptom relief and patient satisfaction.24
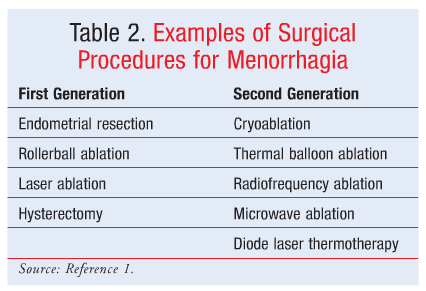
Hysterectomy is perhaps the most definitive treatment for menorrhagia, but it can be quite costly.1 It is a major surgical procedure that involves removal of the uterus and results in complete loss of fertility.9
Endometrial ablation is less invasive and more cost-effective, achieving patient satisfaction rates of about 90% and amenorrhea in about 50% of patients.3 While the uterus is maintained with ablation techniques, the patient loses fertility.9 This technique removes the entire thickness of the endometrium and is preferred by most women as it is a less invasive procedure. Both goserelin and danazol are useful in preparing the endometrium before a rollerball endometrial ablation procedure.25
A uterine artery embolization (UAE) is a procedure whereby both uterine arteries are occluded completely with particulate emboli.9 UAE reduces menstrual loss by about 85%, although it is associated with a higher number of complications and hospital readmissions than in patients who undergo hysterectomy.9
CONCLUSION
With the wide range of effective hormonal and nonhormonal treatment options available on the market, health care professionals, including pharmacists, are in a position to successfully manage menorrhagia. Women should be actively involved in the decision process when selecting a suitable mode of therapy.
REFERENCES
1. Apgar BS, Kaufman AH, George-Nwogu U, Kittendorf A. Treatment of menorrhagia. Am Fam Physician. 2007;75:1813-1819.
2. Shah AA, Grainger DA. Contemporary concepts in managing menorrhagia. Medscape Womens Health. 1996;1:8.
3. Lopes JE Jr, Sherer E. Managing menorrhagia. Evaluating and treating heavy menstrual bleeding. Adv NPs PAs. 2010;1:21-25.
4. Oehler MK, Rees MC. Menorrhagia: an update. Acta Obstet Gynecol Scand. 2003;82:405-422.
5. Hallberg L, Högdahl AM, Nilsson L, Rybo G. Menstrual blood loss—a population study. Variation at different ages and attempts to define normality. Acta Obstet Gynecol Scand. 1966;45:320-351.
6. Bieber EJ, Sanfillipo JS, Horowitz IR, eds. Clinical Gynecology. Philadelphia, PA: Churchill Livingstone; 1991:843-857.
7. Lethaby A, Augood C, Duckitt K, Farquhar C. Nonsteroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(4):CD000400.
8. James AH. Women and bleeding disorders. Haemophilia. 2010;16(suppl 5):160-167.
9. Duckitt K. Managing perimenopausal menorrhagia. Maturitas. 2010;66:251-256.
10. Duckitt K, Collins S. Menorrhagia. Clin Evid (Online). 2008;pii:0805.
11. Sweetman SC, ed. Martindale: The Complete Drug Reference. 34th ed. London, UK: Pharmaceutical Press; 2005 [electronic version].
12. Wellington K, Wagstaff AJ. Tranexamic acid: a review of its use in the management of menorrhagia. Drugs. 2003;63:1417-1433.
13. Philipp CS. Antifibrinolytics in women with menorrhagia. Thromb Res. 2011;127(suppl 3):S113-S115.
14. Hickey M, Farquhar CM. The reproductive years: update on treatment of menstrual disorders. Med J Aust. 2003;178:625-629.
15. Lethaby A, Irvine GA, Cameron IT. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016.
16. Bergqvist A, Rybo G. Treatment of menorrhagia with intrauterine release of progesterone. Br J Obstet Gynaecol.1983;90:255-258.
17. ESHRE Capri Workshop Group. Intrauterine devices and intrauterine systems. Hum Reprod Update. 2008;14:197-208.
18. Brown J, Farquhar C. Oral contraceptive pill for heavy menstrual bleeding. Cochrane Database Syst Rev. 2009;(4):CD000154.
19. Beaumont H, Augood C, Duckitt K, Lethaby A. Danazol for heavy menstrual bleeding. Cochrane Database Syst Rev. 2007;(3):CD001017.
20. Roy SN, Bhattacharya S. Benefits and risks of pharmacological agents used for the treatment of menorrhagia. Drug Safety. 2004;27:75-90.
21. Magos AL. Management of menorrhagia. BMJ. 1990;300:1537-1538.
22. Cetin NN, Karabacak O, Korucuoglu U, Karabacak N. Gonadotropin-releasing hormone analog combined with a low-dose oral contraceptive to treat heavy menstrual bleeding. Int J Gynaecol Obstet. 2009;104:236-239.
23. Candiani GB, Vercellini P, Fedele L, et al. Use of goserelin depot, a gonadotropin-releasing hormone agonist, for the treatment of menorrhagia and severe anemia in women with leiomyomata uteri. Acta Obstet Gynecol Scand. 1990;69:413-415.
24. Practice Committee of the American Society for Reproductive Medicine. Indications and options for endometrial ablation.Fertil Steril. 2008;90(5 suppl):S236-S240.
25. Fraser IS, Healy DL, Torode H, et al. Depot goserelin and danazol pre-treatment before rollerball endometrial ablation for menorrhagia. Obstet Gynecol. 1996;87:544-550





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 