A new position statement for the treatment of type 2 diabetes takes an approach much more focused on the individual patient compared with the "one number fits all" target of glycated hemoglobin (HbA1c) used up to now.
These new recommendations from the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA), announced here today in a news conference at the European Association for the Study of Diabetes (EASD) 48th Annual Meeting, put the patient's condition, desires, abilities, and tolerances at the center of the decision-making process about the goals and methods of treatment. "Our recommendations are less prescriptive than and not as algorithmic as prior guidelines," the authors write.
In light of the increasing complexity of glycemic management in type 2 diabetes and the wide array of antidiabetic agents now available, as well as uncertainties about the benefits of intensive glycemic control on macrovascular complications, a joint task force of the EASD and the ADA sought to develop recommendations for the treatment of nonpregnant patients with type 2 diabetes to help clinicians determine optimal therapies. Their aim was to take into account the benefits and risks of glycemic control, the efficacy and safety of the drugs used to achieve it, and each patient's situation. The resulting guidelines are published simultaneously inDiabetes Care (2012;35:1364-1379) and Diabetologia (2012;55:1577-1596) by the EASD and the ADA and are available on the EASD Web site.
"What we're trying to do is encourage people to really engage in a complex world with the patient, given the variety of choices," said David Matthews, MD, DPhil, from the Oxford Centre for Diabetes, Endocrinology and Metabolism at Churchill Hospital and the National Institute for Health Research, Oxford Biomedical Research Centre, United Kingdom, and cochair of the Position Statement Writing Group of the EASD and ADA. "And the algorithmic approach, in our view, has finally had its day. We can't do that anymore."
Dr. Matthews said the EASD and ADA writing group decided not to issue guidelines but rather to take positions and issue recommendations. "Published guidelines tend to be algorithmic, yet few clinicians prescribe by algorithms...and so there's a lot of lip service to explicit guidelines," he said.
Furthermore, there's a danger in guidelines in that some payers and regulatory bodies focus on them as an absolute measure of success or failure and pay accordingly, or not. So for this reason, the authors did not put a specific HbA1c number in their position statement, and in addition, they did not want to give the impression that it is all right for the number to drift upward if it is below a certain level.
On the other hand, a lower HbA1c value may not be best for some patients. "We've got trial data challenging the simplistic view of the lower-the-better approach to glycemic control.... That tells us we need to be careful about just using numbers, however important they may be, to treat patients," Dr. Matthews said.
So the plan is to have the physician and patient combine the best available evidence with clinical expertise and patient preferences to determine the course of treatment, which may include lifestyle interventions such as physical activity, dietary advice, and oral or injectable antidiabetic drugs, including insulin.
Main Points to New Approach
The position statement lays out 7 key points:
- Individualized glycemic targets and glucose-lowering therapies
- Diet, exercise, and education as the foundation of the treatment program
- Use of metformin as the optimal first-line drug unless contraindicated
- After metformin, the use of 1 or 2 additional oral or injectable agents, with a goal of minimizing adverse effects if possible (despite limited data to guide specific therapy)
- Ultimately, insulin therapy alone or with other agents if needed to maintain blood glucose control
- Where possible, all treatment decisions should involve the patient, with a focus on "patient preferences, needs and values"
- A major focus on "comprehensive cardiovascular risk reduction"
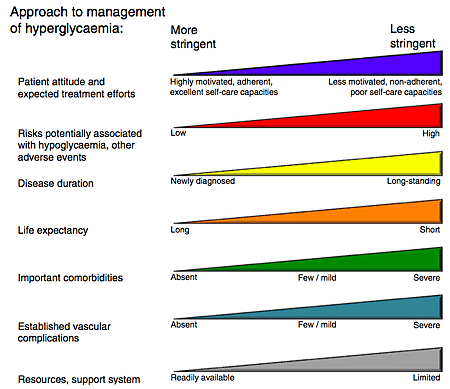
The authors highlight several elements that need to be gauged for making decisions about the appropriate levels of effort to reach glycemic targets. Patient attitudes and expected efforts may range from highly motivated with good adherence and self-care abilities to poor motivation, nonadherence, and poor self-care abilities. The potential risks for hypoglycemia and other adverse effects are another element in decision-making.
The recommendations also focus on duration of disease, life expectancy, significant comorbidities, established vascular complications, and the patient's resources and support system.
The authors make the point that although the recommendations focus on glycemic control, clinicians and patients should also pay attention to other risk factors, and specifically, "aggressive management of cardiovascular risk factors" in light of the increased risk for cardiovascular morbidity and mortality among patients with type 2 diabetes. Physicians should encourage as much physical activity as possible, aiming for a minimum of 150 min/week, consisting of aerobic, resistance, and flexibility training if possible.
If newly diagnosed patients are at or near the HbA1c target of less than 7.5% and they are highly motivated, they should be given a trial of lifestyle changes for 3 to 6 months with a goal of avoiding pharmacotherapy. But for patients with moderate hyperglycemia or for whom lifestyle changes are expected to be unsuccessful, antidiabetic drug therapy, usually with metformin, should be initiated. If lifestyle efforts are eventually successful, drug therapy may be modified or discontinued.
Information to Guide Pharmacotherapy
Many of the drugs to control blood glucose have similar efficacy, said Writing Group cochair Silvio Inzucchi, MD, professor of medicine, clinical director of the Section of Endocrinology, and director of the Yale Diabetes Center at the Yale School of Medicine in New Haven, Connecticut.
Based on an extensive review of more than 500 articles, "all of these drugs work more or less to the same extent," he said. "In the grand scheme of things, when you're talking about a patient taking a medication for years, perhaps decades, and being faced with side effects of medications, the differences in hemoglobin A1c may actually pale in comparison to how they experience that medication."
To guide choices of glucose-lowering agents, the authors provide in tabular form summaries of the cellular mechanisms, physiological actions, advantages, disadvantages, and costs of classes of agents and drugs within the classes. They also show an algorithm for escalating treatment, starting with lifestyle changes and progressing to initial drug monotherapy, 2- and then 3-drug therapy, and finally to basal and then more complex insulin strategies.
The recommendations end with considerations of the effects of age, weight, sex/racial/ethnic/genetic differences, the comorbidities of coronary artery disease, heart failure, chronic kidney disease, liver dysfunction, and concerns about hypoglycemia. The authors also point out several areas where data are insufficient and therefore where research efforts should be aimed.
When asked if the new recommendations are feasible given the time allotted to seeing a patient, Andreas Pfeiffer, MD, DrMed, chief of the Department of Clinical Nutrition at the German Institute of Human Nutrition Potsdam-Rehbruecke in Nuthetal, Germany, and professor of internal medicine and director of the Department of Endocrinology, Diabetes and Nutrition at Charité Universitaetsmedizin Berlin, Germany, was cautious in his answer.
"If you calculate the time a doctor has per patient, it's something like 7 minutes or so, and most patients are used to the physician telling him what he's supposed to do," Dr. Pfeiffer said. "In some ways it's unrealistic" for a physician to explore a patient's desires, capabilities, tolerances, and social support systems in that amount of time. On the other hand, patients return to the doctor several times over the course of a year, so there are more chances to expand the discussion.
But Dr. Pfeiffer worries whether diabetes specialists may become lax if they are not trying to treat to a specific goal. "Diabetologists have average HbA1c's in Germany of around 7%, which is pretty good, actually.... And now if you relax the guidelines and say, 'You don't really have to care so much about it,' so where do they go?" he wondered.
Dr. Matthews has received advisory board consulting fees or honoraria from Novo Nordisk, GlaxoSmithKline, Novartis, Eli Lilly, Johnson & Johnson, and Servier. He receives research support from Johnson & Johnson and Merck Sharpe & Dohme. He has lectured for Novo Nordisk, Servier, and Novartis. Dr. Inzucchi has been an advisor or consultant to Merck, Takeda, Boehringer Ingelheim and has received research funding or supplies to Yale from Eli Lilly, Johnson & Johnson, and Servier. He has participated in medical education projects for Amylin, Eli Lilly, Boehringer Ingelheim, Merck, Novo Nordisk, and Takeda, for which Yale received unrestricted research funding. Dr. Pfeiffer is an advisor to AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, and Lilly.
European Association for the Study of Diabetes (EASD) 48th Annual Meeting. Presented October 2, 2012.
Diabetes Care. 2012;35:1364-1379. Full text
Diabetologia. 2012;55:1577-1596.





 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 