多數人看過的glucagon大概都是長這樣
其實也有專門的急救包
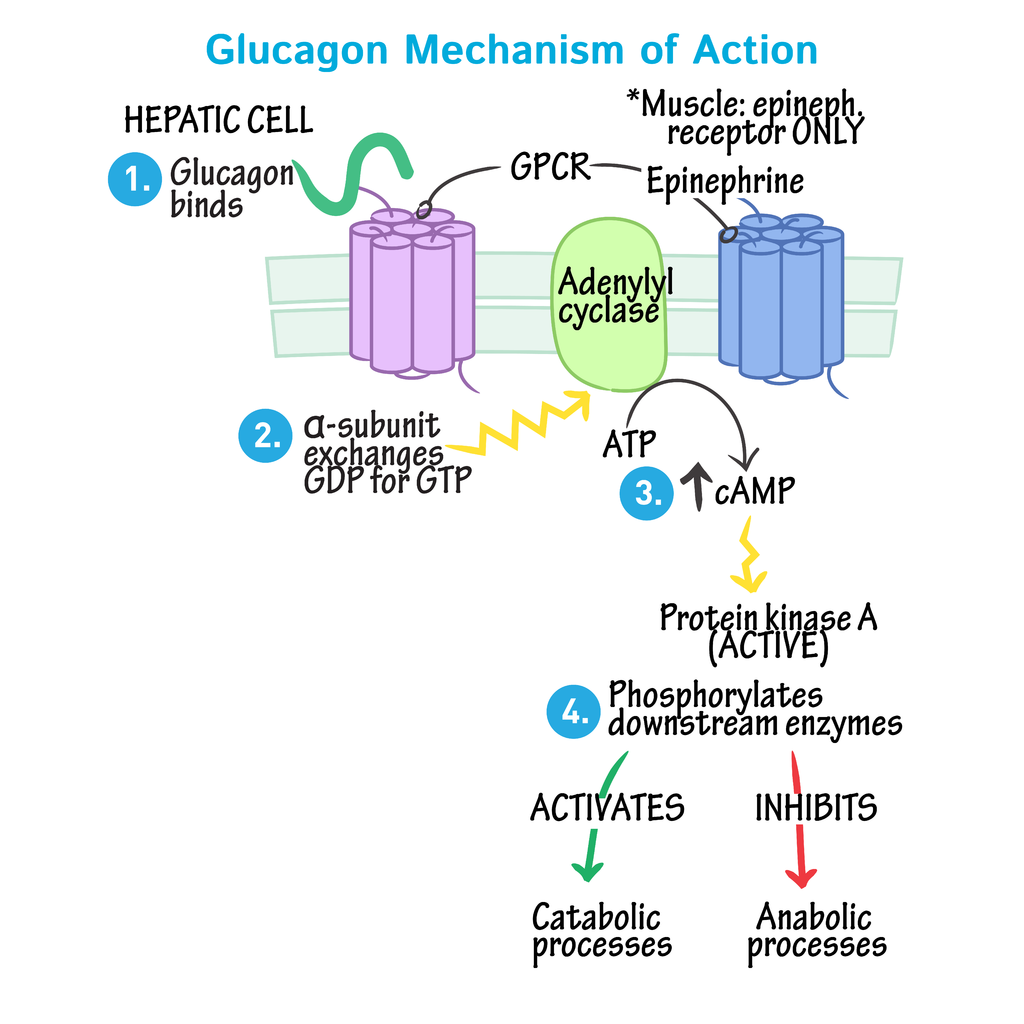
簡單來說機轉是:
What is Glucagon and how does it work?
Glucagon (Gcg) is a peptide hormone, made by alpha cells of the pancreas. When blood glucose level is too low, glucagon-secreting alpha cells produce glucagon and release it into the bloodstream. Glucagon acts primarily on the liver, promoting the conversion of liver glycogen into glucose and the release of glucose into the bloodstream, known as glycogenolysis. It also facilitates gluconeogenesis, the production of glucose from amino acid molecules. Besides, it reduces glucose consumption by the liver as much as possible to ensure that more glucose flows into the blood pressure to keep blood sugar stable. In all, glucagon counteracts the effect of insulin on blood sugar, thus making blood glucose level in a narrow range.
What is Glucagon Signaling Pathway?
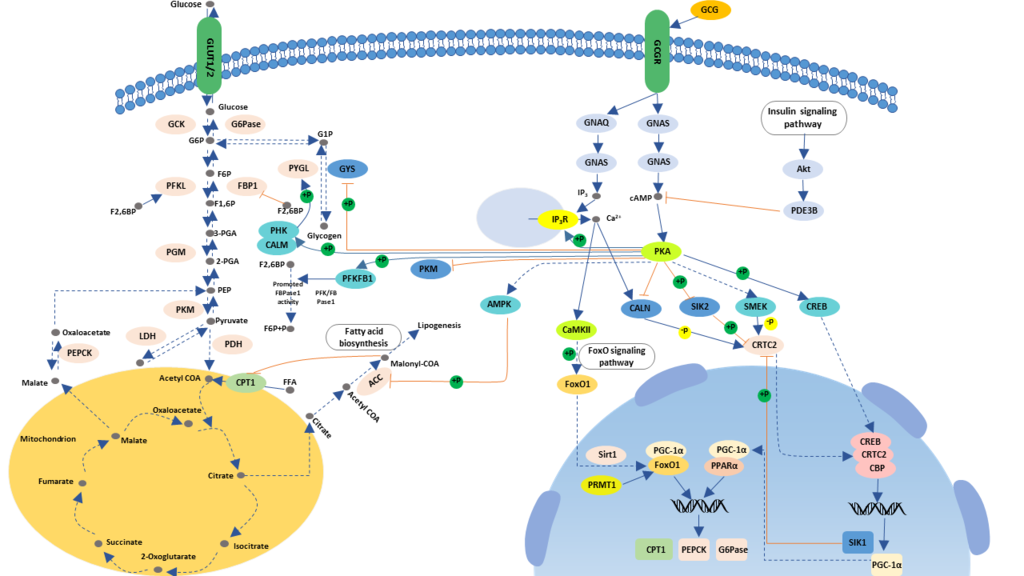
The glucagon signaling pathway is a process of a series of elevated blood glucose enzymatic reactions triggered by the binding of glucagon that produced by pancreatic islets alpha cells to the glucagon receptor on the surface of liver cells.
The Function of Glucagon Signaling Pathway
Glucagon signaling pathway mainly assists glucagon to exert its role of raising blood glucose to sustain blood glucose homeostasis in the body and synergizes with insulin. In other words, the glucagon signaling pathway can prompt the catabolism of glucose, which is opposite to the role of the insulin signaling pathway.
The Process of Glucagon Signaling Pathway
The glucagon receptor (GcgR) is a member of the family B receptors within the G protein-coupled superfamily of seven transmembrane-spanning receptors. Glucagon receptors primarily distribute on the surface of liver and kidney cells. When blood glucose levels are low, pancreatic alpha cells secrete glucagon. And then, glucagon binds to glucagon receptors on the target organ, which induces a conformational change in the receptors, resulting in activation of the G proteins conjugated to the receptors, mainly Gs and Gq.
● The cAMP Dependent Protein Kinase A Pathway
Activated Gs, in turn, activates adenylate cyclase, which catalyzes the production of cyclic adenosine monophosphate (cAMP) by ATP. The generated cAMP acts as a second messenger to activate the protein kinase A (PKA) pathway. In this pathway, elevated cAMP-activated PKA, in turn, activates glycogen phosphorylation kinase, which phosphorylates glycogen phosphorylase into an active alpha form that initiates the breakdown of hepatic glycogen, also known as glycogenolysis. cAMP can also phosphorylate glycogen synthase by PKA, inactivating glycogen synthase, thereby inhibiting glycogen synthesis. Besides, CAMP can also activate lipoprotein kinase via PKA to promote fat hydrolysis. The glycerin and fatty acid content in the plasma rises, and as a result, the gluconeogenesis is enhanced.
● The cAMP Independent Protein Kinase A Pathway
Upon the activation of Gq, the phospholipase c-inositol triphosphate channel is activated, resulting in intracellular Ca2+ release. Together with PKA, Ca2+ activates ERK1/2 protein, and ERK1/2 phosphorylation activates CREB. CREB is activated by ERK and binds to PGC-1 promoter to enhance PGC-1 expression. PGC-1 can up-regulate G-6-Pase and the transcription level of PEPCK, thereby increasing glucose.
Glucagon also stimulates beta-oxidation of liver mitochondria, which provides energy for glucose production.
Factors Causing Glucagon Signaling Pathway
DysfunctionGenetic variation and functional change of the protein molecules involved in the glucagon signaling pathway, as well as metabolic factors, cause abnormal signal transduction, which triggers hyperglycemia. So these abnormalities are also targets of drug therapy for hyperglycemia and related diseases.
The Diseases Associated with Glucagon Signaling Pathway
Studies have confirmed that disruption of the glucagon signal leads to hyperglucoseemia and alpha-cell proliferation. Abnormal high-level secretion in patients with type II diabetes may be due not only to dysregulation of glucose levels and "missing" in islets, but may also reflect impaired glucagon signaling in the liver.
It has been reported that some patients with glucagonoma have very low amino acid levels, suggesting that pathological glucagon levels may cause liver inhalation of amino acids to be converted to urea. And the conversion may lead to severe hypoamino acidemia. It is well known that glucagon is a powerful regulator of amino acid production of liver urea.
Commonly, obese patients have dysfunction both in islet alpha and beta cells, resulting in excessive secretion of glucagon, impaired insulin secretion, thus triggering severe disorder of blood glucose metabolism in the body. Therefore, having a deep understanding of the glucagon signaling pathway is very helpful to research therapy for obesity.
如果想看中文版,這邊勉強看看






 留言列表
留言列表
 線上藥物查詢
線上藥物查詢 